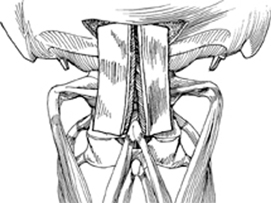
7 Robert K. Eastlack, Bradford L. Currier, and Alexander R. Vaccaro To facilitate arthrodesis of the occipitocervical or atlantoaxial segments. Thorough preparation of the grafting site and use of autograft bone with adequate stabilization should result in a healthy fusion mass. Grossly infected sites should be debrided and treated with appropriate surgical/medical management before application of metal instrumentation and bone grafting in some cases. The timing of the graft placement and instrumentation must be addressed on an individual basis. Shortened life expectancy (less than 3 to 6 months) may obviate the usefulness of bone grafting, but it is prudent to err on the side of overtreatment. Autograft bone may be harvested from the posterior-superior iliac spine or ribs. Bicortical specimens should be obtained when the graft is providing structural support in the area of fusion. If there is inadequate structural or morselized autograft bone specimen available, allograft bone may be used or autograft bone can be supplemented with demineralized bone matrix adjuncts. Do not place bone graft directly on neural elements, including the C2 exiting nerve root or ganglion. Prepare the atlas and axis similarly prior to graft placement. It is very important to adequately expose and decorticate the C1 arch and laminae of C2. Using a Kerrison rongeur to decorticate the caudal portion of C1 and cranial portion of C2 will avoid a dural tear from the burr. Absence of the C1 posterior arch, or the need for laminectomy at C1 or C2, may necessitate placement of bone graft into the atlantoaxial joints. Carefully elevate the C2 ganglion to expose the atlantoaxial joint on each side. Remove cartilage joints with a curette or burr and pack morselized cancellous graft into the joints. Corticocancellous strut grafts can be applied laterally and held in place with wires or cables secured to the bone or the instrumentation. This bone graft can be carried up to a prepared occipital bony surface when occipitocervical fusion is desired. The occipital bone should be prepared sufficiently laterally from midline to accommodate the graft placement over the C1–2 articulation. This step can be accomplished in a variety of ways, depending on the extent of fusion required below the axis, as well as the accompanying instrumentation. Corticocancellous strips placed parasagittally in a longitudinal fashion can be employed (Fig. 7.1). Alternatively, a large unicortical piece of iliac crest autograft can be placed over the occiput-C2 region, using a midline caudal notch to help with its positioning on the cephalad aspect of the C2 spinous process (Fig. 7.2). Prepare the dorsal aspect of the posterior elements and occiput by decorticating them, and ensure that the cancellous surface of the graft abuts those areas well. The graft can be secured to the occiput by a midline screw or wire, or held in place by the overlying soft tissues. With newer rod/screw fixation techniques, morselized cancellous autograft bone appears to be sufficient if applied liberally to well-decorticated surfaces. Bilateral instrumentation in combination with secure occipital fixation obviates the apparent need for structural bone graft material. Because of the small surface area comprising the posterior arch of C1, we typically use a supplemental interlaminar bicortical bone graft (via one of the methods described below) at the atlantoaxial site.
Grafting Methods: Posterior Occipitocervical Junction and Atlantoaxial Segment
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Occipitocervical Grafting
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








