(examine for the following)
(repeat at regular intervals, usually every 15 mins)
csf leak from nose/ear, usually clear
bleeding around eyes & subconjuctiva
bleeding from external ear
bruising over the mastoid (Battle’s sign)
confirm by testing fluid for glucose
no posterior limit indicates fractured skull
exclude laceration of external ear
may take 48 hours to develop
Imaging
All head injuries should be considered for imaging. Imaging includes plain X-rays of skull and spine, CT of the head and occasionally MRI of the brain and spinal cord. Indications for urgent CT include depression/loss of consciousness, focal neurological signs, seizures, fractured skull and CSF leak. CT may reveal evidence of fractures, intracranial haematomas and cerebral contusion (Fig. 19.1).
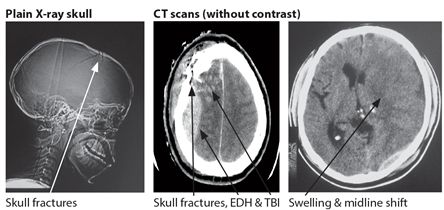
Figure 19.1 Traumatic brain injury
DIFFUSE AXONAL INJURY (DAI)
This occurs from the shearing of axons as a result of a high impact closed HI. It is usually associated with an immediate LOC which persists after the injury. Imaging initially by CT is normal in >50-70% of cases and this may need to be repeated after 24/48 hours before showing haemorrhages and cerebral oedema. MRI is more sensitive than CT in the early stages of DAI. Management includes sedation, ventilation and measures for intracerebral pressure monitoring and control.
Classification
The classification or grading of HI is based on the initial history, clinical evaluation and GCS. This is made in order to identify and treat patients at risk. It is important to remember that the majority of cases of HI do not result in TBI. Of those that do, TBI is graded as mild if the GCS at assessment is >12, or the period of unconsciousness is <30 minutes. The majority, 85-90% of all TBIs are classified as mild. TBI is classified as moderate if the current GCS is 9-12 or there is persisting coma for >30 mins or there is a skull fracture but no evidence of brainstem malfunction (Table 19.3). TBI is categorised as severe if unconsciousness is greater than 24 hours or current GCS ≤8 or there are focal neurological signs or intracranial haematoma or failing brain stem function. Patients with moderate and severe TBI represent about 10-15% of all cases.
Table 19.3 Traumatic brain injury, summary of main clinical features
| Grade | GCS | % | CT signs present* | Mortality % | Morbidity % | Disability |
| mild | 13-15 | 85-90 | in one third | 1 | 50 (minor) | none/minor |
| moderate | 9-12 | 5-10 | in two thirds | 2-5 | 60 | disabled |
| severe | 3-8 | 3-5 | in all** | 20-50 | 75 | severely disabled |
* includes fractured skull, contusion, bleeding, swelling
** except in diffuse axonal injury (DAI) when the initial CT of head may be normal
Key points
Management
The medical management of brain injured patients is complex. It involves 4 main sites/stages: pre hospital care, transport to hospital, in hospital care and rehabilitation. Any delay or failure at any of these stages results in increased mortality and morbidity.
Trivial and mild
Trivial head injuries and mild TBIs account for the majority of TBIs and most patients may be discharged home after initial examination with a warning about possible complications. The risk of complications for mild TBIs is low <1%. However patients with mild TBI and other clinical features of head injury should be admitted for 24 hours for closer neurological observations, care, possible CT scanning and a re-evaluation later. This group has an increased risk (1-5%), of serious neurological deterioration. The main indications for a CT scan in mild TBI include alteration in level of consciousness, confusion, a history of transitory loss of consciousness, post traumatic amnesia, the presence of focal neurological signs and a possible skull fracture. A skull X-ray should be performed if a CT scan is unavailable.
Moderate and severe injuries
This group represents 10-15% of all TBIs. Moderate and severe head injuries should all have a CT scan of the head, be admitted to an intensive care unit for observation and care and considered for any possible neurosurgical intervention.
Evaluation of moderate and severe TBIs
The first priority is to check that the airway is clear and that breathing and circulation are adequate. This may involve inserting an airway and ensuring that oxygen saturation is >95%. Circulation is maintained by starting emergency intravenous fluids and ensuring that ≤2 litres is given in the first 24 hours unless the patient is hypovolaemic for other reasons (Chapter 9). The next step is the evaluation of the extent and seriousness of the injuries. Many patients, in particular RTA cases, have concomitant injuries of the chest, abdomen, spine and extremities.
All patients with HI and altered consciousness should be assumed to have a neck injury and be immobilized until proven otherwise. This means a general evaluation in addition to measuring the level of consciousness, examining for neurological deficits and for evidence of head and spinal cord injury, and any skull or vertebral fractures. (Table 19.3) Check with family or friends for any history of any predisposing risk factors for head injury including loss of consciousness, stroke, seizures, alcohol and drugs. The GCS together with vital signs, pupil size and reaction to light should be checked every 15 minutes in unstable patients and then at 1-4 hourly intervals appropriate to the patient’s condition. Special attention should be paid to avoiding the risk factors for secondary brain injury; this includes maintaining adequate blood pressure and oxygen saturation. If the patient’s consciousness is deteriorating then mannitol 1 gm/kg/iv is given stat followed by iv boluses of 1-200 ml of 20% mannitol depending on the clinical situation. This may be helpful as a short term measure to reduce intracranial pressure. Prophylactic antibiotics and antiepileptics are indicated for all severe head injuries. Indicators of a poor prognosis are: coma for >6 hours, fractured skull, non reacting pupils and focal neurological deficits. The main indications for neurosurgical intervention are extradural and subdural haematoma, depressed skull fracture and occasionally intracerebral haemorrhage.
Key points
- 4 main stages, prehospital, transport, in hospital and rehabilitation
- aim is to prevent secondary complications of TBI
- brain damage is prevented by adequate evaluation & care
- this involves ABC & preventing seizures & infection
- CT head scan indicated in all moderate & severe TBI
- main indications for surgery are extradural & subdural haematomas and some ICH
OUTCOME
TBI accounts for up to half of all traumatic deaths with over half of these deaths occurring at the scene of the accident or on the way to hospital. The possible outcomes of TBIs are summarized in Table 19.3 and in the Glasgow Outcome Scale (Table 19.4). The initial grade of TBI after the primary injury is the most important predictor of outcome.
Table 19.4 Glasgow Outcome Scale
| Classification | Description |
| dead | |
| persistent vegetative state | awake but unaware |
| severely disabled | conscious but dependent |
| moderately disabled | independent but disabled |
| good recovery | may have minor sequelae |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








