Cryptococcus neoformans
Mycobacterium tuberculosis
Toxoplasma gondii
Cytomegalovirus
JC virus (progressive multifocal leucoencephalopathy)
Tumours
Primary CNS lymphoma (PCNSL)
meningitis
meningitis, *FND, paraplegia
*FND
retinitis, radiculopathy, encephalitis
quadriplegia, encephalopathy
*FND
<100
(0-500)
<100
<50
<100
<100
10-20%
1-10%
5-15%
1-1.5%
uncommon
<1%
vacuolar myelopathy
distal sensory neuropathy (DSN)
retinopathy
frontal lobe release signs
<100
<200
<200
<200
5-20%
20-30%
5-10%
50-70%
GBS
polymyositis
rare
rare
seizures
stroke
paraplegia
5-10%
<1%
1-2%
* FND: hemiparesis, seizures, ataxia, cranial nerve palsies, coma
The main clinical presentations are meningitis, focal neurological deficits, seizures and altered level of consciousness; these are mostly caused by opportunistic infections and frequently occur, when more than one HIV related illness is present. Disseminated TB occurs in >50% of patients with advanced HIV disease in Africa.
CLINICAL PRESENTATIONS
MENINGITIS
Meningitis is one of the common neurological presentations of HIV infection in Africa. The main causes are C. neoformans and M. tuberculosis (Chapter 6). Both cause chronic meningitis and occur predominantly in patients with CD4 counts <100/cm3 although TB meningitis (TBM) may also occur at higher CD4 levels. Acute forms of meningitis also occur but these are much less common; the main acute forms are acute bacterial (ABM) secondary to pneumococcus and viral meningitis. Cryptococcal meningitis (CM) is now the most common type of meningitis in many parts of Africa and after TB it is the leading cause of death in AIDS in parts of Africa, accounting for up to a quarter of all HIV related deaths there (Fig. 8.1). TBM is also common and has been shown at post-mortem in West Africa to be present in >10% of AIDS patients (Fig. 8.2).
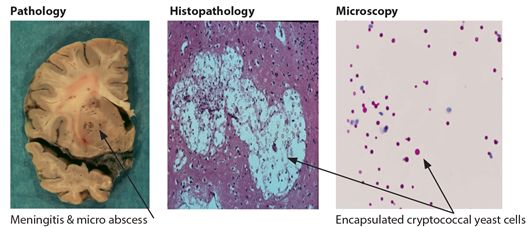
Figure 8.1 Brain & CSF in cryptococcal meningitis
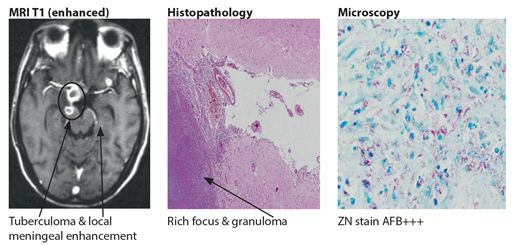
Figure 8.2 Brain in CNS tuberculosis
Clinically, CM and TBM may be indistinguishable from each other, although the onset of headache coupled with fever, nausea and vomiting evolving during the preceding week or two is more suggestive of CM. Definite signs of meningism are typically absent in CM in up to 75% of patients. Raised intracranial pressure with papilloedema is more common in CM but occurs in both types of meningitis.
Laboratory investigations can help to distinguish the different types of meningitis. In both types of meningitis the CSF shows an elevation in cells (mainly mononuclear) and protein but CSF can also be normal in 10-20% of patients. Distinguishing features in the CSF in CM are the presence of encapsulated yeast cells on India ink (60-80 %) and cryptococcal antigen (95%) and in TBM, AFB (<5% routine ZN staining). The percentage of positive AFB in CSF in TBM can be significantly improved (60%) by increasing the volume of CSF to 20 mls, centrifuging the sample and by microscopy for 20 minutes. The presence of cryptococcal antigenaemia may be detected in the blood during the 2-3 weeks preceding the onset of CM in some patients allowing for the possibility of earlier treatment. CT of the brain is usually not helpful but may show more basal meningeal enhancement in TBM and occasionally the presence of a tuberculoma. Supporting evidence for TBM includes the presence of concurrent systemic TB, (chest radiograph 40%) or failure to improve after 1-2 weeks of treatment for CM. Treatment of either or both CM or TBM is started immediately for suspected or confirmed infection as outlined in Table 8.2.
Table 8.2 Treatment based on presenting neurological disorder & likely cause
| Neurological Disorder | Opportunistic infection | Treatment Regime | When to start |
| FND | toxoplasmosis (TE) | TMP-SMX# | immediate |
| Meningitis | cryptococcus (CM) | fluconazole/ amphotericin B | immediate |
| Coma | toxoplasmosis cryptococcus | TMP-SMX & fluconazole/ amphotericin B | immediate |
| Meningitis or FND or Coma | tuberculosis* | isoniazid pyrazinamide rifampicin ethambutol & steroids | immediate/or added@ 2/52** |
# trimethoprim/sulphamethoxazole
* TB treatment is started or added if chest radiograph or other findings indicate TB
** if there is treatment failure after 2/52 for either TE or CM
FOCAL NEUROLOGICAL DISORDERS (FND)
Focal neurological disorders are among the most common neurological disorders in HIV disease. The main causes are Toxoplasma encephalitis (TE), tuberculoma and lymphoma. FNDs occur typically in patients with CD4 counts <100 cells/cm3 but can occur at higher CD4 counts. The main clinical presentations are hemiparesis, cranial nerve palsies and ataxia (50-60%), seizures, lethargy, confusion (40%) and coma. TE causing brain abscess is usually the most common cause of FND (Chapter 7), occurring in 5-15% of AIDS patients, although its frequency within Africa, will vary depending on the local prevalence of toxoplasmosis. Tuberculoma was reported to be the most common cause of focal brain lesions in HIV in one study area in South Africa. In TE there is usually a history of headache (60%) and fever (40-70%) over the preceding days or 1-2 weeks. Other indicators of TE include positive Toxoplasma serology and multiple ring-enhancing mass lesions on CT. A negative Toxoplasma serology makes the diagnosis of TE unlikely.
The main differential diagnosis in TE includes tuberculoma and lymphoma. However tuberculoma and primary cerebral lymphoma (PCL) are much less common and both have a slower clinical course than TE. On CT, while both tuberculoma and lymphoma can appear to be similar to TE, (Figs. 8.3–5) they may differ in their site and distribution in the brain (Chapter 7). Other less common causes of FND in HIV to be considered include stroke, occasionally syphilis and progressive multifocal encephalopathy (PML).
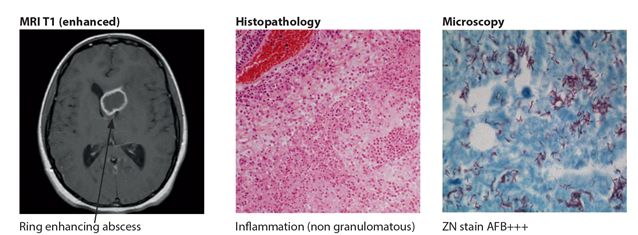
Figure 8.3 Brain in lymphoma
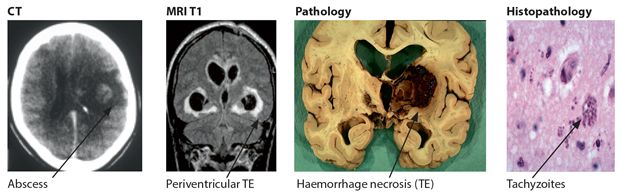
Figure 8.4 Brain in toxoplasmosis
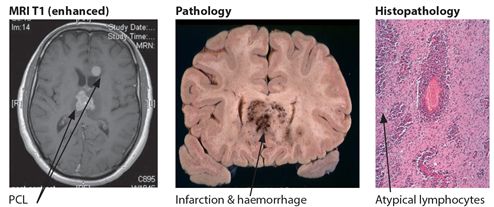
Figure 8.5 Brain in lymphoma
The choice of treatment in the management FNDs is based mostly on clinical suspicion and likely cause and the results of available investigations including a CT scan of the head (Table 8.2). Treatment is started immediately with high dose trimethoprim-sulfamethoxazole in those patients with suspected TE (Table 8.2). Clinical improvement is expected by day 3 in around 50% and by day 14 in 90% and if resources allow a follow up CT confirming improvement is helpful. TB treatment is indicated from the outset in all those suspected TB cases particularly if there is evidence of concurrent disseminated TB (e.g. AFB in sputum/typical chest radiograph findings for tuberculosis). The diagnosis of CNS TB should also be considered, if there is a failure or a poor response to treatment for TE after 7-14 days. If there is any indication from the start of either CM or ABM, then appropriate antimicrobials should be added from the start of treatment.
CONFUSION AND COMA
States of confusion, altered level of consciousness and coma are common clinical presentations particularly in the advanced stages of HIV disease in Africa. These states are mostly caused by the same opportunistic processes, usually infections that result in meningitis and FNDs but representing more advanced disease. Other causes of confusion and coma in HIV should also be considered, including metabolic disorders, organ failure particularly renal and cardiac, and side effects of ART medication, in particular efavirenz. If the cause is not known, then presumptive treatment should be started for the main OIs, CM, TE and ABM together until the precise diagnosis becomes clear (Chapters 6–7). If there is clinical evidence of TB, then TB treatment should also be added (Table 8.2).
STROKE
Stroke typically occurs during the otherwise asymptomatic phase of HIV infection when CD4 counts are 200-500 cells/cm3. An association between stroke and the persistent generalized lymphadenopathy (PGL) stage of HIV has been shown in South Africa. The accumulated lifetime prevalence of stroke in HIV disease is <1%. Stroke can be difficult to diagnose clinically, mainly because the presentation is very similar to the non vascular causes of focal brain lesions in HIV infection. The clinical diagnosis of stroke is suggested by its acute onset, non progressive course and better clinical outcome. A CT scan of the brain may be necessary to confirm the correct diagnosis. The majority of strokes are ischaemic and occur in the anterior circulation. Mechanisms include vasculitis, coagulopathies, meningitis and emboli secondary to cardiac disease. Investigations and management are the same as for any stroke patient and should include a serology test for syphilis.
SEIZURES
New onset seizures occur in up to 5-9% of HIV infected persons at some stage throughout their long illness. Seizures occur most commonly during the later stages of HIV infection mostly as a complication of focal brain lesions secondary to opportunistic processes, in particular toxoplasmosis and tuberculoma. However, they may also occur at higher CD4 levels during the asymptomatic stage of HIV infection without any obvious underlying focal cause when their aetiology is related mostly to vasculitis. The seizures, although focal in origin are secondary generalized tonic-clonic in type. Management is directed at investigating and treating the suspected cause and suppressing the seizures (Table 8.2).
PROGRESSIVE MULTIFOCAL LEUCOENCEPHALOPATHY (PML)
PML is caused by the reactivation of a latent virus (JC virus) which is carried by most healthy people. It appears to be uncommon in AIDS in Africa (<1%). PML occurs in advancing states of immunosuppression when the CD4 count is <50/cm3 but can occur in patients with higher CD4 counts <200 cm3. The clinical presentation is one of a devastatingly severe progressive neurological disorder occurring over weeks and months. It is characterized by motor dysfunction (hemiparesis, quadriparesis), ataxia, seizures and cognitive changes (60-70%) and aphasia, visual problems and cranial nerve palsies (30-40%). CSF examination is usually normal. Neuroimaging may show hypodense disease in the white matter brain and cerebellum (15%). The diagnosis is confirmed by brain biopsy showing the typical JC inclusions in the oligodendrocytes (Fig 8.6). There is no effective treatment for PML but all suspected patients should start ART with some showing stabilization or improvement.
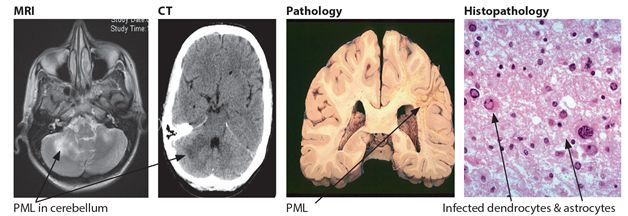
Figure 8.6 Brain in PML
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








