Imaging of Pediatric Spinal Injury
Avrum N. Pollock
Stephen M. Henesch
In children, fractures and severe injuries to the spine are relatively rare and represent between 1% and 10% of injuries reported by various authors (1, 2, 3, 4 and 5). Spinal fractures in children represent between 1% and 2% of all pediatric fractures (6). Compared with adults, spinal trauma is relatively rare in pediatric patients; however, the mortality rate is higher in children as a result of associated injuries (7, 8). The anatomy and biomechanics of the growing spine, which include larger head size relative to body size, greater flexibility of the spine and supporting structures, incomplete ossification, as well as greater elasticity and compressibility of the bone, produce failure patterns different from those seen in adults. Anatomic differences between the pediatric and adult cervical spine are prominent until approximately 8 years of age and persist to a lesser degree until approximately 12 years of age (9, 10, 11, 12, 13 and 14). By the time a child is age 8 to 10 years of age, his or her spine has reached near adult size. Younger children present an additional challenge, as they are developmentally unable to communicate crucial symptoms. Furthermore, the physical examination can be limited by lack of cooperation in an anxious, crying child.
Spinal Development
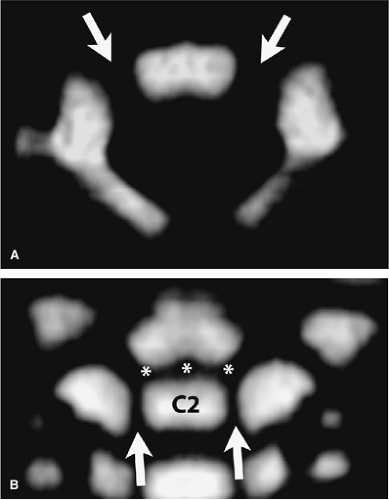
Differing spinal levels demonstrate variability in their development, and awareness of these developmental and anatomic variants is essential in detecting true abnormalities in the pediatric spine. Avellino et al. (15) noted that among the most common factors for misdiagnosis of cervical spine injuries were unfamiliarity with the pediatric spine and failure to recognize normal variants. Spinal development in the upper cervical vertebrae is different from that of the lower cervical vertebrae (Fig. 9-1). The C1 vertebra develops from three ossification centers (body and two neural arches) (Fig. 9-1A). Anomalies occur when these centers either fail to develop or fail to fuse. The posterior arch normally fuses by the age of three. C2 develops from four ossification centers (body, odontoid, and two neural arches) (Fig. 9-1B) that are present at birth and also fuse by the age of three. The body and odontoid are joined by the dentocentral synchondrosis, and the body and neural arches are joined by two neurocentral synchondroses. The remainder of the lower cervical spine vertebrae develop with three primary centers of ossification (two neural arches and one vertebral centrum) that
are joined by two neurocentral synchondroses, which fuse by the time a child is 3 to 6 years of age. The vertebrae of the cervical and thoracic spine also have five secondary ossification centers (one spinous process, two transverse processes, and two ring apophyses). In addition to these five secondary centers, the lumbar spine has two additional centers corresponding to the mamillary processes.
are joined by two neurocentral synchondroses, which fuse by the time a child is 3 to 6 years of age. The vertebrae of the cervical and thoracic spine also have five secondary ossification centers (one spinous process, two transverse processes, and two ring apophyses). In addition to these five secondary centers, the lumbar spine has two additional centers corresponding to the mamillary processes.
Imaging Modalities
Radiographs (Plain Films)
Radiographs of the cervical spine remain the initial imaging modality of choice for children of all ages following trauma. The Guidelines for the Management of Acute Cervical Spine and Spinal Cord Injuries published by the American Association of Neurological Surgeons/Congress of Neurologic Surgeons (16) suggest, however, that these films may not be necessary in children following trauma who are alert, conversant, have no neurologic deficit, no midline or cervical tenderness, no painful distracting injury and are not intoxicated; these criteria are those that have been used by the National Emergency X-Ray Utilization Study (NEXUS) (17). This recommendation has been based in part in a study by Viccellio et al. (18) who applied the NEXUS criteria to the pediatric population and noted that application of these findings could reduce cervical spine imaging in children by up to 20%. In this study, however, there were few injured patients below the age of 9, and none were under the age of 2, which would suggest caution in applying these criteria to patients nine and younger.
In those patients who undergo radiography, an adequate lateral view is essential when evaluating this region as this view alone has 79% sensitivity for spinal injury (19). In the same study, a three-view radiographic series was shown to have a sensitivity of 94%. In the pediatric age group, prevertebral soft tissue swelling is a poor predictor of underlying abnormality and is often dependent on the degree of neck flexion and adequate inspiratory effort. An odontoid view should not even be attempted unless a child is old enough to follow commands, which in our experience occurs by approximately 5 years of age (20). Any suggestion of an abnormality on radiographs or any clinically suspicious area that is not properly visualized on radiographs warrants a focused computed tomography (CT) scan of the level in question, as well as one level above and below the level of suspected fracture (Fig. 9-2).
The role of flexion-extension radiography in the pediatric population has been controversial. Dwek and Chung (21) performed a retrospective review of 247 children who underwent flexion-extension radiography following standard static cervical spine imaging and found that if the standard views were normal, flexion-extension films did not find abnormalities and were therefore of “questionable use.” Ralston et al. (22) also found that flexion-extension views were unlikely to be abnormal if standard radiographs showed no acute abnormality or isolated loss of lordosis (22). They also noted that flexion-extension views were of “limited usefulness” in confirming ligamentous injury in those patients with significant acute abnormalities on standard radiographs. However, they did note that flexion-extension radiographs could help rule out ligamentous injury in patients with suspicious findings on radiographs for occult ligamentous injury, including segmental kyphosis, prevertebral soft tissue swelling, and equivocal subluxation.
Computed Tomography
Complete CT scanning of the entire cervical spine, which may be the norm in adults, is not warranted in the child,
given the additional radiation dose to the thyroid. The thyroid gland has an increased sensitivity to radiation in the growing child, and thus a similar radiation dose per gram of weight of tissue has a greater potential for developing fatal cancer later in life (23, 24). Furthermore, the use of blanket trauma protocols increases the number of studies performed without a significant increase in injury identification, thus increasing cost without improving outcome (25).
given the additional radiation dose to the thyroid. The thyroid gland has an increased sensitivity to radiation in the growing child, and thus a similar radiation dose per gram of weight of tissue has a greater potential for developing fatal cancer later in life (23, 24). Furthermore, the use of blanket trauma protocols increases the number of studies performed without a significant increase in injury identification, thus increasing cost without improving outcome (25).
The standard multidetector CT (MDCT) technique of imaging the cervical spine consists of thin (0.6 to 1.3 mm) axial helically acquired images, which can then be further broken down to thinner increments, thereby optimizing reconstructed images in the sagittal and coronal planes. Images are routinely reviewed on soft tissue and bone algorithms/windows.
Hernandez et al. (26) retrospectively evaluated 606 pediatric patients under the age of 5 who were evaluated for cervical spine injury. Of these patients, 76% were cleared by plain films and clinical exam; of the remaining 24% (147 patients), only 2.7% (4 patients) demonstrated new traumatic findings, which in retrospect appeared to have been visible on plain films. Adelgais et al. (27) demonstrated that the use of screening CT for cervical spine injury in the pediatric population increased radiation dosage without decreasing either the time of the patient in the emergency department or reducing sedation usage. Therefore, considering the increased risk of cancer, CT should be used sparingly as a screening modality for cervical spine trauma in the pediatric population. Keenan et al. (28), however, identified subgroups that may benefit from screening CT without increasing radiation dose or cost. One such subgroup was patients with high risk for cervical spine trauma, including those unrestrained passengers in motor vehicle accidents with head trauma and Glasgow Coma Scale less than 8, for which
initial spine CT at time of cranial CT did not increase cost or radiation dose. It is worth noting that in pediatric patients with traumatic spinal injury, craniocerebral injury is the most common associated injury (29).
initial spine CT at time of cranial CT did not increase cost or radiation dose. It is worth noting that in pediatric patients with traumatic spinal injury, craniocerebral injury is the most common associated injury (29).
Magnetic Resonance Imaging
As children are more likely to have nonosseous cervical spine injuries than adults, magnetic resonance imaging (MRI), with its superior evaluation of soft tissue structures, would potentially be useful in the pediatric population. There have been relatively few articles, however, that address this issue. Keiper et al. (30) found that MRI could detect soft tissue abnormalities (including edema/ligamentous injury, spinal cord contusion, extra-axial hemorrhage, vertebral body subluxation/distraction occult fracture or disc protrusion) in 31% of patients who had normal radiographs or CTs and presented either with persisting or unexplained symptoms, signs of injury or instability not entirely explained by plain films, or with need for further evaluation of the extent of soft tissue injury not characterized by plain films.
Standard MRI technique, performed on a 1.5 Tesla system, consists of T1- and T2-weighted sagittal and axial imaging, as well as a sagittal short tau inversion recovery (STIR) and fat-saturated T2-weighted sequences.
A gradient echo susceptibility sequence can also be performed to assess for the possibility of blood products. If vertebral artery injury is suspected, additional axial fat-saturated T1-weighted images are required, with time-of-flight magnetic resonance angiography (TOF MRA) to assess the patency of the vertebral arteries.
Flynn et al. (31) found that MRI altered plain film diagnoses in 34% of patients who underwent the study in order to define the diagnosis or clear the cervical spine, because plain films and physical evaluation were inconclusive; they maintained that MRI was their imaging modality of choice in clearing the cervical spine for obtunded, intubated, or uncooperative children. A similar recommendation for obtunded and intubated pediatric patients is made by Frank et al. (32) who noted that MRI resulted in earlier clearing of the cervical spine with resultant cost savings of $7,000 per patient. Other indications
for MRI are potential spinal cord birth injuries (33) and spinal cord injury without radiographic abnormality (SCIWORA).
for MRI are potential spinal cord birth injuries (33) and spinal cord injury without radiographic abnormality (SCIWORA).
Spinal Cord Injury without Radiographic Abnormality
SCIWORA is far more common in younger children than in older children, and is far more common in the cervical spine than it is in the thoracolumbar region (34). SCIWORA is found in 30% to 40% of children with spinal cord injury (35) and was originally described with regard to plain radiographs, but has grown to include CT scans, and in most cases has excluded MRI. A substantial number of children with neurologic deficits, however, show no evidence of abnormality on either MRI or somatosensory-evoked potential (SSEP). Several studies have shown that the main predictor of long-term outcome in SCIWORA patients is the neurologic status at admission, in that only patients presenting with mild to moderate initial deficits attain full recovery (36, 37 and 38). Abnormalities visualized on MRI have more recently been shown to surpass clinical neurologic status with regard to prognosis, specifically with regard to cord concussion (39). In select cases, patients who have normal MRI examinations in the setting of complete sensorimotor paralysis have improved completely within 2 days (40). The agility of the pediatric spine creates the potential for serious spinal injuries in the setting of apparently normal initial radiographic evaluation. Therefore, it has been suggested that all patients with SCIWORA should obtain an MRI (35).
Upper Cervical Spine Injuries (Occipital, C1, and C2)
Distraction Injuries
Spines of neonates, infants, and young children are especially vulnerable to distraction injuries (Figs. 9-3,Figs. 9-4,Figs. 9-5,Figs. 9-6,Figs. 9-7 and 9-8) secondary to ligamentous injury/disruption in the upper cervical spine. Eleraky et al. (41) demonstrated that in children <9 years old, 78% of cervical spine injuries were in the upper cervical spine (occiput-C2) and 68% had either subluxation without fracture or SCIWORA. This contrasts with older children (ages 10 to 16) in which 70% sustained lower cervical spine fractures and 80% of the children in this group had fractures or a fracture with subluxation. Most distraction injuries in children occur before 5 years of age, with the vast majority occurring prior to 6 months of age (42, 43); however, it has been reported that atlanto-occipital dislocation is more common in the 5- to 9-year-old age range (44). This predilection for upper cervical spine injuries in younger children may be due to a combination of factors. One may be the relatively larger head mass which results in a higher center of gravity. Additionally, spinal immaturity and ligamentous laxity, which may be beneficial for lower cervical spine, may not be able to withstand the sheer forces in the upper cervical spine (7). Spinal distraction injuries are rare in children, however, they are often fatal, due to associated high cervical spinal and brainstem injury leading to respiratory and cardiac arrest (45, 46). In those patients who survive, they may be quadriplegic, as Leventhal (47) demonstrated that the spinal cord ruptures beyond a mere 1/4 inch of forced lengthening. Additionally, there may be associated cranial nerve and vascular stretch injuries (46), as well as diffuse axonal injury supratentorially (45). Certain congenital and acquired pathologies, including Down syndrome, Klippel-feil syndrome, Grisel syndrome, neoplasms, and myogenesis, may predispose to these injuries due to a combination of ligamentous laxity and bony abnormalities in the upper cervical spine (41).
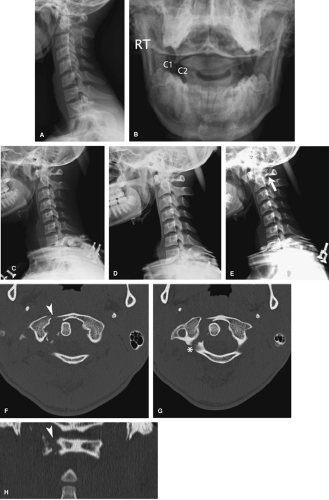
As with adults, diagnosis of atlanto-occitipital distraction (or disassociation) (AOD) may be made by plain film using Powers ratio (BC:OA), which is the distance between the basion and posterior arch of C1 (BC) divided by the distance between the opisthion and anterior arch of the atlas (OA).
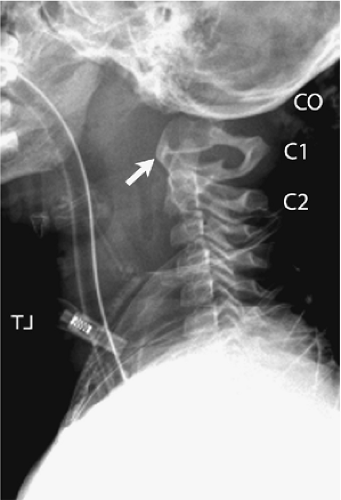
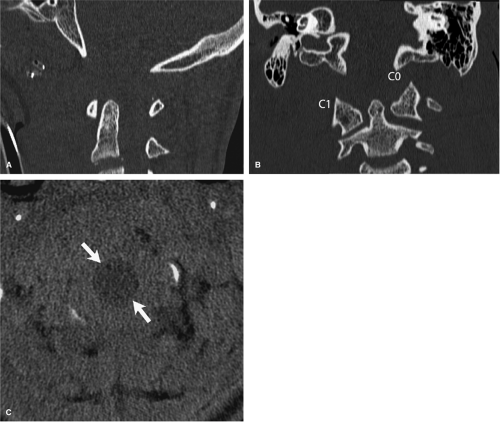
A ratio >1.0 is considered diagnostic for AOD, with 0.77 being the mean for a normal population (46). The basion-dental interval (BDI) may also be used, with a measurement of >10 to 12.5 mm considered abnormal (46, 48). Although other authors have found the BDI measurement to be unreliable in children (49), Bulas et al. (48), however, reported that in a series of 11 children with AOD, all had a BDI >14 mm and only six had a Powers ratio >1.0. Kenter et al. (46) suggest that both measurements be taken in patients with suspected AOD. CT with sagittal and coronal reformations may make the diagnosis easier as bony landmarks may be better visualized (Figs. 9-3, 9-4). Additionally, subarachnoid hemorrhage (SAH), which is seen in over 50% of patients with AOD, can also be visualized (Figs. 9-4, 9-8). This finding of infratentorial subarachnoid is important when reviewing cranial CTs following trauma, as, 2% of traumatic brain injury results in infratentorial SAH; thus the presence of this findings should prompt further evaluation for spinal injury (50). MRI may also be utilized to directly evaluate ligamentous injury as well as spinal cord parenchymal and vascular injury (Figs. 9-5, 9-7). Sun et al. (51) used MRI evaluation of ligamentous injury to define a new measure for detecting tectorial membrane injury from plain films. They found that in patients with tectorial membrane injury, the ratio of C1-2:C2-3 interspinous distances was >2.5 (Fig. 9-5).
A ratio >1.0 is considered diagnostic for AOD, with 0.77 being the mean for a normal population (46). The basion-dental interval (BDI) may also be used, with a measurement of >10 to 12.5 mm considered abnormal (46, 48). Although other authors have found the BDI measurement to be unreliable in children (49), Bulas et al. (48), however, reported that in a series of 11 children with AOD, all had a BDI >14 mm and only six had a Powers ratio >1.0. Kenter et al. (46) suggest that both measurements be taken in patients with suspected AOD. CT with sagittal and coronal reformations may make the diagnosis easier as bony landmarks may be better visualized (Figs. 9-3, 9-4). Additionally, subarachnoid hemorrhage (SAH), which is seen in over 50% of patients with AOD, can also be visualized (Figs. 9-4, 9-8). This finding of infratentorial subarachnoid is important when reviewing cranial CTs following trauma, as, 2% of traumatic brain injury results in infratentorial SAH; thus the presence of this findings should prompt further evaluation for spinal injury (50). MRI may also be utilized to directly evaluate ligamentous injury as well as spinal cord parenchymal and vascular injury (Figs. 9-5, 9-7). Sun et al. (51) used MRI evaluation of ligamentous injury to define a new measure for detecting tectorial membrane injury from plain films. They found that in patients with tectorial membrane injury, the ratio of C1-2:C2-3 interspinous distances was >2.5 (Fig. 9-5).
Occipital-atlanto-axial Instability
The atlanto-occipital joint allows extension and flexion, which in turn causes an anterior translation of C1 on C2. Movement >5 mm and 3 mm, in a child less than and >8 years old respectively, indicates atlanto-axial instability, which is suggestive of ligamentous laxity and possible
transverse ligament disruption. In equivocal cases, flexion and extension views have shown to be of some benefit, as opposed to their acquisition in clearly normal cases, where they have not shown to be beneficial (52). As noted above, many processes can cause ligamentous laxity, and thus atlanto-axial instability can also be seen in the nontrauma setting, most commonly with Trisomy 21 (Fig. 9-9), but also in spondyloepiphyseal dysplasia and mucopolysaccharidoses.
transverse ligament disruption. In equivocal cases, flexion and extension views have shown to be of some benefit, as opposed to their acquisition in clearly normal cases, where they have not shown to be beneficial (52). As noted above, many processes can cause ligamentous laxity, and thus atlanto-axial instability can also be seen in the nontrauma setting, most commonly with Trisomy 21 (Fig. 9-9), but also in spondyloepiphyseal dysplasia and mucopolysaccharidoses.
Pseudosubluxation
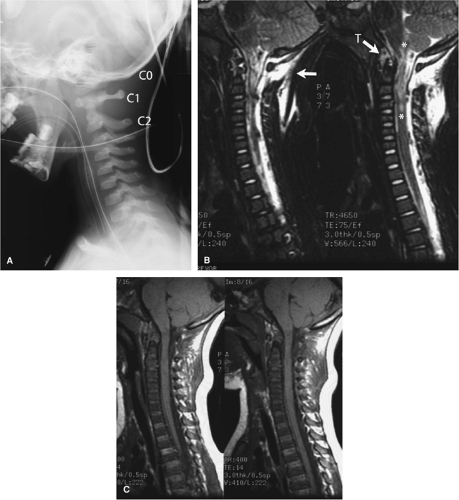
Pseudosubluxation, or normal physiologic displacement of C2 on C3, and to a lesser extent C3 on C4, can mimic
the appearance of a true cervical spine injury (Fig. 9-10). However, studies have shown that ∼ 40% of children under the age of 8 demonstrate pseudosubluxation at the C2-3 level (53). The spinolaminar line is a line drawn from the anterior aspect of the spinous process of C1 to the anterior aspect of the spinous process of C3. When the anterior edges of the respective spinous processes line up to within 1.5 mm of each other on both flexion and extension views, this confirms the pseudosubluxation, and consequently rules out suspected true injury (54). This is not the case with a true cervical spine injury associated with displacement/subluxation (Fig. 9-11). A measurement of >2 mm is definitely abnormal, indicating a true injury, while a measurement of 1.6 to 1.9 mm is considered indeterminate (54).
the appearance of a true cervical spine injury (Fig. 9-10). However, studies have shown that ∼ 40% of children under the age of 8 demonstrate pseudosubluxation at the C2-3 level (53). The spinolaminar line is a line drawn from the anterior aspect of the spinous process of C1 to the anterior aspect of the spinous process of C3. When the anterior edges of the respective spinous processes line up to within 1.5 mm of each other on both flexion and extension views, this confirms the pseudosubluxation, and consequently rules out suspected true injury (54). This is not the case with a true cervical spine injury associated with displacement/subluxation (Fig. 9-11). A measurement of >2 mm is definitely abnormal, indicating a true injury, while a measurement of 1.6 to 1.9 mm is considered indeterminate (54).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree