Figure 63-1 Thermoregulatory sweat distribution test, including the face. Areas with normal sweating are in purple. Areas with loss of sweating lack the purple color. Upper frame, before treatment; the patient shows a patchy distribution of anhidrosis, primarily involving his forehead, face, neck (arrows), and shoulder, and hypohidrosis of right upper thigh and feet suggesting a neuropathic process that is multifocal and non–length dependent that is often found in inflammatory sensory neuronopathies (ganglionopathies). Lower frame, 3 months after treatment; there is notably improved sweating in the forehead, face, neck (arrows), and right upper thigh and feet. The large white abdominal path and surrounding loss of sweating are due to a recent unrelated surgical scar.
The patient underwent a left greater auricular nerve biopsy that demonstrated a low rate of axonal degeneration, focal perineurial thickening, epineurial neovascularization, and large, moderate, and small epineurial inflammatory infiltrates that involved vessel walls. These results suggested an inflammatory/immune etiology, including microvasculitis (Fig. 63-2).
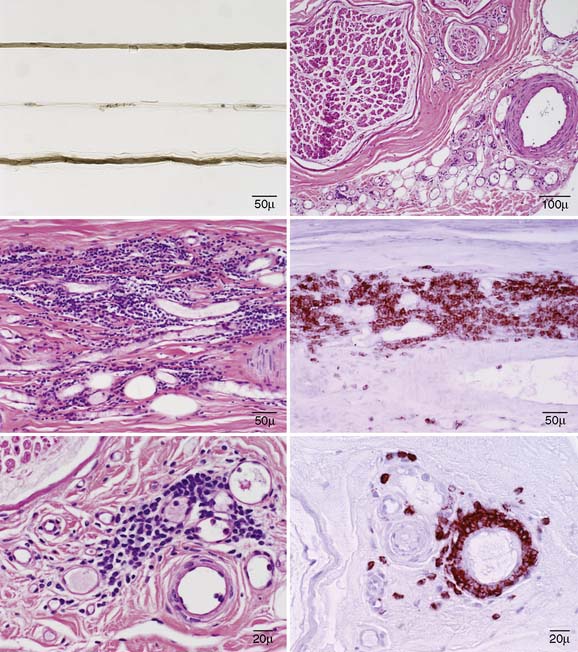
Figure 63-2 Left upper frame, teased fiber preparation showing a nerve fiber undergoing late axonal degeneration (middle fiber). Right upper frame, a transverse hematoxylin and eosin (H&E) paraffin section showing epineurial neovascularization adjacent to an arteriole. Left middle frame, a longitudinal H&E paraffin section, showing a large epineurial perivascular collection of inflammatory cells with involvement of the vessel wall that reacts to a leukocyte (CD45) preparation, right middle frame. Left lower frame, a transverse H&E paraffin section, showing one of multiple moderate collections of inflammatory cells surrounding epineurial vessels. Right lower frame, a transverse paraffin section reacted to CD45 showing a small epineurial perivascular inflammatory collection involving the vessel wall.
He was treated with intravenous (IV) methylprednisolone at 1 g per treatment. After 3 months of weekly infusion, his facial numbness stopped progressing and stabilized, his speech improved, his oral intake of ground food increased, he regained 14 kg in weight, his upper limb reflexes normalized, the left facial motor compound muscle action potential increased from 0.3 to 1.3 mV, the needle EMG of the left orbicularis muscle showed new nascent units, and his TST showed normalization of sweating in the forehead, neck and feet and improvement of sweating in the face and left clavicular region (see Fig. 63-1).
After 11 months of IV pulsed steroids and 3 months of mycophenolate mofetil, he started to regain sensation in his gums and teeth, and from the edges of his face toward the midline. After four years of immunosuppressive treatment, he has recovered sensation in his lateral cheeks, tongue, roof of his mouth, gums and teeth. He still has a dense sensory loss in the midline of his face. Salivation has significantly decreased, dysarthria has resolved, and he has regained a total of 22 kg.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








