Fig. 3.1
Sagittal parameters that are important in the evaluation of ASD and can be used for surgical planning. Sagittal vertical axis (SVA), pelvic tilt (PT), and pelvic incidence minus lumbar lordosis (PI–LL) are correlated with the disability of patients
SVA is used to determine global sagittal alignment and is the distance between a vertically drawn plumb line from the midpoint of the C7 vertebra and its offset from the posterior-superior corner of the sacral end plate.
PT is the angle between a line drawn from the center of the femoral head axis to the midpoint of the sacral plate and the vertical. PT denotes the spatial orientation of the spine.
PI-LL is a sagittal modifier that represents the difference between the angle measurement of PI and the angle measurement of LL.
PI is defined as the angle between a line drawn from the center of the femoral head axis to the midpoint of the sacral plate and the perpendicular to the sacral plate.
LL is measured as the angle between the plane defined by the superior S1 plate and the superior L1 plate.
Subsequent work determined radiographic measurement pain and disability thresholds as indicated by widely utilized pain and disability questionnaires. Schwab et al. delineate surgical radiographic parameter goals and confirm that improvements in sagittal modifier class correlate with pain and disability improvement. The threshold for disability is defined as an ODI score greater than 40, an SVA greater than 47 mm, a PT greater than 22°, and absolute value of PI minus LL greater than 11° [24]. Considering the radiographic parameter correlation with pain and disability, Schwab et al. define realignment objectives in the sagittal plane as an SVA less than 50 mm, a PT less than 20°, and LL equal to PI ± 9° (Fig. 3.2) [25].
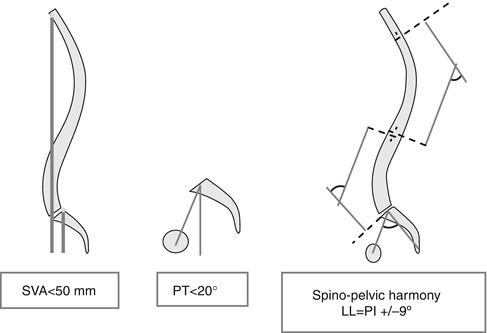
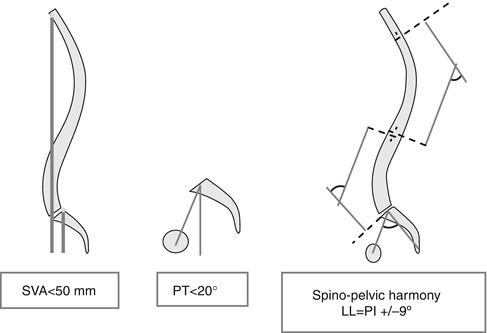
Fig. 3.2
Surgical parameter measurement goals based on correlations between these parameters and HRQOL survey scores
3.4.1 Imaging Analysis and Diagnosis
Radiographic measures in the context of ASD evaluation require images obtained in a freestanding patient position. This patient positioning is essential to effectively evaluate key aspects of a deformity and potential compensatory mechanisms that a patient may be recruiting. If a patient is not in a weight-bearing position, global deformity, truncal inclination, or compensatory mechanisms can be underestimated and lead to improper patient evaluation and treatment. Ideal standing radiograph position involves natural foot position, forward shoulder flexion, and elbow flexion to bring fingertips onto the cheekbones or midclavicles (Fig. 3.3) [26]. CT and MRI studies have quantified the response of the lumbar spine to rotatory torque and have correlated increased axial rotation in degenerated discs with pain provocation on discography [27, 28]. Additionally plain radiographic findings in patients with axial low back pain may demonstrate characteristics consistent with degenerative disc disease. While radiography does not demarcate soft tissue disc, film may reveal decreased disc height consistent with a collapsed or dehydrated disc. Sclerotic end plates or bone-on-bone appearance are commonly seen with severely degenerated discs and may indicate pain origin [5]. A review of common imaging techniques applied in the evaluation of symptomatic ASD follows.


Fig. 3.3
Proper standing position for ASD evaluation radiography
3.4.2 X-Ray
Conventional radiography with plain-film radiography is any easy procedure to perform. Whole spine images of the standing frontal (anteroposterior) and sagittal (lateral) view are required for adequate evaluation of the patient’s deformity. Radiographs should include the occiput superiorly and the femoral heads inferiorly. This process allows spinal assessment in a freestanding position (Figs. 3.3 and 3.4). However, this method utilizes ionizing radiations and can be harmful with prolonged exposure. Newer technologies, such as those employed by EOS imaging, may offer low-dose alternatives to traditional single-beam radiographs.


Fig. 3.4
Example of an AP X-ray image
3.4.3 MRI
MRI uses a strong magnetic field in the radio frequency range. This method is particularly useful for the visualization of soft tissue structures, especially the disc space and adjacent soft tissues. Nonetheless, major limitations of this process include the inability to obtain standing images and long acquisition times. The use of a strong magnetic field may also be problematic for patients with electronic devices such as a pacemaker or spinal cord stimulators.
3.4.4 CT
CT imaging produces tomographic slices of specific area of the body through the axial plane. Computer algorithms allow image reconstruction in the sagittal and coronal planes. This process is particularly useful for bone tissue visualization. Combination with myelography, which consists of an intrathecal contrast agent injection, allows a clear and accurate representation of the spinal anatomy. Results of this combination provide better osseous and joint anatomy than MRI. However, as with conventional radiographs, this method utilizes ionizing radiations that may be dangerous for patients (Fig. 3.5).


Fig. 3.5
Example of an AP CT scan in a scoliosis patient (Reprinted with permission from Ha et al. [53])
3.4.5 EMG
EMG may be helpful in identifying sources for radicular pain patterns and guide indications for surgery. EMG is defined as muscular electrical activity recording and forms a valuable aid in the neuromuscular function assessment. EMG and nerve conduction studies are routinely used to differentiate radiculopathy from peripheral symptoms and confirm the localization of radicular compression. Patients who present with abnormal EMG and signs of radiculopathy may be eligible for surgical decompression if focal pathology is confirmed on imaging.
Biomechanical studies have demonstrated that the spine itself cannot bear large loads and therefore recruits the paraspinal musculature to maintain shape [29]. In ASD evaluation, abnormal EMG recordings in one study were shown to be predictive relative to progression of deformity, as asymmetry in paraspinal EMG activity at the lower end vertebra of the curve was associated with deformity progression [30].
3.5 Operative Indications
The foremost indication for surgical ASD treatment is the lack of response to nonsurgical pain and disability management. Nonsurgical treatments include bracing, pain medication, exercise, and physical therapy. If these conservative treatments fail to provide satisfactory outcomes, ASD surgery may be indicated.
To determine whether or not a patient will likely benefit from surgical treatment for ASD, Schwab et al. describe a binary logistic regression method to build predictive models of certain independent variables including gender, age group, BMI, subluxation degree, osteotomy, and sagittal balance, among others [13]. The minimal clinically important difference (MCID) was determined by several widespread pain and appearance surveys. Patients most likely to benefit significantly from surgery had higher grades of deformity by the classification modifiers, more severe subluxation, and worse pain and disability scores. From a clinical perspective, patients with less morbidity before surgery have lower improvement potential in terms of disability and may be more affected by the difficulties associated with recovery than the clinical improvement realized by surgical correction of ASD.
A comparison study of matched pairs of operative and nonoperative ASD treatment by Glassman et al. demonstrated that nonsurgical patients have greater preoperative risk factors, while surgical patients have larger coronal curves and more frequent leg pain and more severe back pain [31]. Surgery is indicated in younger adult patients with large curvature of the spine accompanied by chronic pain or disability that is unrelieved by conservative management. Surgical correction may also be indicated when deformity is aesthetically unacceptable to the patient. Surgery is indicated in the elderly for the same reasons but is also indicated for significant loss of pulmonary function not attributable to underlying pulmonary disease [32].
The risks and potential benefits of any planned surgery must be carefully weighed and reviewed in open discussion with patients. The goal of ASD surgery is often not to completely restore function or remove all deformity and pain, but to offer improved alignment, halt progression, and provide stability to address the main components of deformity – disability and pain. The patient’s expectations regarding the surgery must be clearly established and managed, as unrealistic patient expectations lead to dissatisfaction with the end result.
It is important to underline the capabilities of any given surgeon and medical team in performing corrective surgery. For example, in a given case, a transforaminal lumbar interbody fusion (TLIF) may be the preferred technique compared to a combined anterior/posterior interbody fusion because it is associated with shorter operating time, less blood loss, shorter hospital stay, and lower incidence of complications including infection and pseudoarthrosis [33]. However, a TLIF should not be attempted by a surgeon without experience in this technique if he/she is more experienced with anterior/posterior interbody fusion.
3.6 Benefits of Surgical Treatment
The surgical treatment of ASD has become an extensively studied topic and the potential benefits of surgery have been widely established. Surgical treatment of ASD has been found to significantly improve spinal alignment and improve factors associated with QOL. ASD patients treated surgically report a greater reduction of total pain, leg pain, and fatigue and significant improvements in self-image and daily function in comparison to ASD patients treated nonoperatively [34–39]. The benefits associated with surgery should be considered by patients and physicians in the decision to choose surgical treatment.
Reduction of pain and disability: The surgical treatment of ASD can significantly reduce pain associated with spinal deformities. In a study of surgical versus nonsurgical treatment of adults with idiopathic scoliosis, surgically treated patients reported a significantly greater decrease in back pain, leg pain, fatigue, and disability than patients who were treated nonsurgically [34, 36, 39]. The management of pain and disability is a critical factor to consider in treatment decisions.
Improvement of QOL measures: Patients with ASD demonstrate greater functional limitations and greater daily analgesic use and report worse QOL measures than matched patients without ASD [2, 34, 40]. Patients should also be counseled that a major complication is more likely with revision, staged, and anterior/posterior surgery to improve understanding of risk profiles [2]. Studies have found that surgical treatment results in many benefits associated with improving the QOL of patients. Surgically treated patients experience a greater improvement in self-image and the ability to perform physical, functional, and positional tasks than nonsurgically treated patients [34, 37]. In a cohort study of patients with adult symptomatic lumbar scoliosis, operative treatment significantly improved QOL, whereas nonoperative treatment, whether observation, treatment with medications, or combining medication with injections and physical therapy techniques, did not significantly improve QOL for patients [35]. Furthermore, a retrospective review of conservative and surgical treatment of degenerative lumbar scoliosis found that patients who were treated surgically had significantly improved walking ability and QOL and experienced very few complications [38]. Though surgical treatment is often considered for the reduction of pain and disability for ASD patients, it is also imperative to consider QOL factors into the treatment decision. The changes in health-related quality of life (HRQOL) after surgical treatment of ASD can be predicted by the SRS-Schwab classification system.
In a study by Schwab et al., operatively treated patients had significantly greater disability and poorer HRQOL scores than the nonoperatively treated group. The operatively treated group also had significantly greater baseline deformity, reflected by worse scores for the SVA and PT modifiers by the SRS-Schwab classification parameters. However, at 1-year follow-up, the operatively treated patients showed significantly greater improvements than the nonoperatively treated group. These findings further support the potential for surgical treatment to improve the quality of life for adults with spinal deformity.
Improvements for elderly patients: The potential benefits of surgical treatment for ASD apply to all adults; however, a recent study has illuminated the possibility that surgical treatment provides disproportionately greater benefits to elderly patients [41]. A retrospective review of patients undergoing surgical treatment revealed that compared to younger patients, older patients were shown to have significantly greater baseline disability, greater severity of back and leg pain, and worse health status. Furthermore, elderly patients experienced significantly more complications with surgical treatment than younger patients. However, despite the greater disability and higher complication rate, elderly patients were found to have statistically indistinguishable postoperative outcomes measures of disability, health status, and back and leg pain as the younger age groups. This suggests that elderly patients may have a greater improvement in disability and pain with surgery, in comparison to younger patients. Another study demonstrated the substantial benefit of surgical treatment for patients over 65 years old with degenerative disc disease who are treated with decompression and arthrodesis [42]. Patients over 65 years old showed a greater improvement in back and leg pain scores than patients under 65 years old. Due to the increased risk of complications, surgical treatment might not always be advised for elderly patients. However, the findings that elderly individuals may have disproportionately greater benefits from surgical treatment can aid in the decision-making process for this patient population.
3.7 Risks of Surgical Treatment
Despite the proven potential benefits of surgical correction of ASD, there are many risks and complications associated with surgery. Patients who are deciding to undergo surgical treatment for ASD must balance the possible improvement from surgery with the inherent risks of the procedure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








