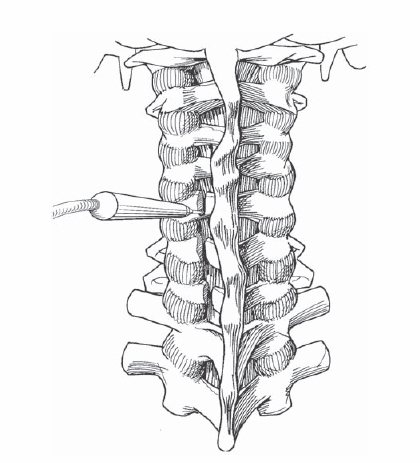
3 Kazuhiro Chiba To achieve adequate decompression of the spinal cord and the nerve roots by shifting the laminae posteriorly, yet preserving cervical stability by retaining the posterior bone-ligamentous complex. In addition to the local decompression effect by the posterior shift of the laminae, the total or indirect decompression effect by the posterior migration of the spinal cord away from anterior pathologic structures, such as disk herniation, osteophyte, and ossified ligament, can be expected in this procedure, unless the patient’s cervical alignment is kyphotic. Preserved laminae provide protection to the spinal cord and serve as an attachment to the stripped muscles and preserved ligaments, including the supraspinous, interspinous, and yellow ligaments. Relief of myelopathy caused by multilevel compression due to cervical degenerative diseases and ossification of the posterior longitudinal ligament. Long-term outcomes of expansive laminoplasty are satisfactory, for example, neurologic improvement assessed by the Japanese Orthopaedic Association (JOA) scoring system is approximately 50 to 60%. Adjacent segment disease and nonunion, which are noted after anterior fusions, can be avoided. No postoperative external support is necessary. Patients with multilevel spinal cord compression due to cervical spondylosis, or ossification of the posterior longitudinal ligament. Patients who have developmental spinal stenosis are also good candidates for laminoplasty even if they have single-level disease, such as a disk herniation. Preoperatively established severe kyphosis (C2–C7 kyphotic angle over 10 degrees); severely unstable cervical spine, for example, athetoid cerebral palsy, rheumatoid arthritis, and destructive spondyloarthropathy. Careful evaluation of the lateral radiographs to assess for developmental spinal canal stenosis (anteroposterior diameter of the spinal canal <13 mm), which, if symptomatic, is an indication for this procedure. Computed tomography (CT) is used to measure the thickness of the laminae and to decide the optimal positions of the gutters. Magnetic resonance imaging (MRI) is used to assess the laterality of spinal cord compression, thereby deciding the side of laminar opening. Laminae are usually opened at the side of predominant compression. A prone position with a Mayfield pin headrest. Flex the neck slightly to open up the space between the occiput and cervical spine to obtain adequate exposure. Tilt the surgical table about 30 degrees to bring the flexed neck parallel to the horizontal plane. Use endotracheal general anesthesia. Incise the nuchal ligament and paracervical muscles at the exact midline, and strip the muscles subperiosteally to avoid bleeding. Complete the hinge side gutter last, after completion of the open side gutter and the resection of the ligamentum flava at both ends of the laminar door. Check the stability of the hinge frequently while making the hinge gutter. Preserve the spinous process of C7 whenever possible, to reduce postoperative axial symptoms. Encourage early active neck exercise. Uncontrollable epidural bleeding is sometimes encountered during the laminar opening procedure, especially in ossification of the posterior longitudinal ligament (OPLL) procedures. In some cases, the laminar door cannot be opened readily, due to remaining bony continuity on the open gutter side, inadequate resection of the ligamenta flava, and inadequate drilling of the hinge gutter. The laminae, in most cases, from C3 to C6 or C7, are exposed through a midline incision followed by dissection of bilateral paracervical muscles. At the junction of the lamina and the facet joint, the open side gutter is made using a high-speed drill. The ventral cortex of the laminae is perforated using a diamond burr (Fig. 3.1). Ligamenta flava at the cranial and caudal ends of the intended laminar expansion, usually at the C2-3, C6-7, or C7-T1 interspaces, are resected using a thin-bladed Kerrison rongeur, while opening the interspace with a small laminar spreader. Another gutter in the contralateral side is made, while preserving the ventral cortex. This side now functions as a hinge. Make the hinge gutter slightly wider and more lateral than the open gutter side to avoid abutting of the cut edges of the lamina and facet joint and to allow adequate opening (Fig. 3.2). To prevent hinge problems, the stability of the hinge is checked frequently while deepening the hinge gutter by applying a gentle bending force to the spinous processes.
Laminoplasty
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








