42 Lateral Extracavitary Approach
I. Key Points
– The posterolateral approach allows for circumferential neural decompression under direct visualization with extrapleural/extravisceral dissection.
– Single-stage ventral and dorsal column support can be achieved using the same incision.
– Thoracic disc herniations or osteophytes
– Thoracic fractures
– Anterolateral decompression for neoplasms
– Osteomyelitis with anterior column compromise
– Lesions located between T3 and L2
III. Preoperative Preparation2
– Sagittal magnetic resonance imaging (MRI) should include “scout radiographs” because of the ability they provide to count to the precise spinal level of interest.
– Anteroposterior (AP) chest x-ray confirms presence of 12 ribs.
– Spinal angiogram is useful in case of lesions between T6 and L2 to identify the radiculomedullary artery of Adamkiewicz.
– Computed tomography (CT) scan can be helpful for studying the bony anatomy.
– The patient is intubated and general anesthesia is administered.
– Antiembolism stockings and Foley catheter are placed.
– Large-bore peripheral and central catheters are necessary given the possibility of rapid blood loss during the procedure.
– Patient is placed in the prone position on a spinal table.
• The patient must be well secured to the table to allow for safe lateral tilting during surgery.
• Arms are tucked at the sides or above the head and all pressure points are padded.
– Spinal cord monitoring is optional.
– Incision is made in the midline with a “hockey stick”–shaped curve.
• Incision is carried through the subcutaneous tissue to the thoracolumbar fascia.
• Self-retaining retractors are placed, and the fascia is opened vertically over the spinous processes.
• Exposure of the spinous process, lamina, facets, costotransverse junction, and rib at each level is performed.
– The curved portion of the skin incision is made just caudal to the last level to be instrumented and is angled 8 cm laterally to allow adequate soft tissue retraction.
– The fascial incision is curved laterally to expose the lateral border of the erector spinae muscles.
– The erector spinae muscles are dissected off the ribs and reflected medially.
• The muscle group can be tented up with a Penrose drain.
– Reconfirm the spinal level and rib of interest with AP fluoroscopy.
– Remove the rib 7 to 10 cm lateral to the costovertebral junction.
• Rongeuring the tip of the corresponding transverse process may facilitate this procedure.
• Special attention should be given to ensure the pleura is not punctured.
– Identify the neurovascular bundle and follow it medially to the vertebral foramen.
• If necessary, ligate the intervening intercostal vessels and nerves.
• The nerve should be sectioned proximal to the dorsal root ganglion prior to closure to prevent anesthesia dolorosa.
– The sympathetic chain is encountered and displaced ventrally in a subperiostal fashion.
– A localization radiograph is taken with a spinal needle placed into the disc space.
– Visualization of the vertebral body and pedicle is enhanced by tilting the operating table 15 to 20 degrees away from the surgeon.
– The foramen is enlarged with the use of curettes until the lateral aspect of the thecal sac is exposed.
• Consider starting with a midline laminectomy in case of severe ventral thecal sac compression.
• Epidural bleeding can be controlled with a hemostatic agent and Cottonoids (Saramall, Buenos Aires, Argentina); electrocautery should be avoided adjacent to the thecal sac.
– The rostral portion of the pedicle just inferior to the disc space is removed.
– The annulus of the disc is incised just ventral to the posterior longitudinal ligament.
– Disc material and bone ventral to the thecal sac are broken down into the cavity with the use of curettes or thin, flat instruments.
– After removal of adjacent discs, corpectomy can be completed with a high-speed drill.
• The adequacy of ventral decompression is determined by use of dental mirror.
– Anterior stabilization can be achieved with the placement of an anterior graft into the corpectomy site.
• The use of expandable cages is recommended to provide anterior support.
– The operating table is tilted back to the neutral position.
– AP/lateral x-rays can aid in assessing the position of the anterior graft and facilitate placement of posterior instrumentation.
– The wound is closed in a multilayered fashion (Fig. 42.1).
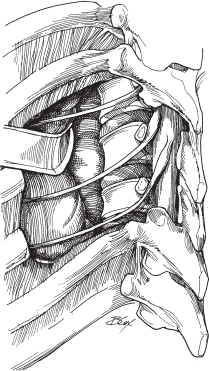
Fig. 42.1 Lateral view of the retracted paraspinal muscle bundle medially and the myocutaneous flap laterally, the lateral dural sac and exiting nerve roots, and the lateral vertebrae.
– Pneumothorax
– Hemothorax
– Pleural effusion
• Significant pleural fluid collections are best treated with tube thoracostomy rather than thoracentesis.
– Dural tear
– Spinal cord injury
– Anesthesia dolorosa
VI. Postoperative Care
– Aggressive pulmonary toilet is necessary to prevent postoperative pneumonia.
– Surgical drains and chest tubes are typically discontinued at 48 to 72 hours.
– External orthosis is recommended following instrumentation cases for up to 12 weeks.
VII. Outcomes2
– Reported series showed 70% improvement in myelopathy from thoracic disc herniation.
– Eighty percent improvement is reported in neurologic condition from traumatic lesions of thoracic spine.
– Morbidity rate is significant and reported to be as high as 55% in one series.2
VIII. Surgical Pearls
– The intercostal nerve should be divided proximal to the dorsal root ganglion to prevent anesthesia dolorosa.
– Meticulous dissection of the rib and rib head to avoid pleural injury along with gentle retraction of the lung may help minimize pulmonary morbidity.
Common Clinical Questions
1. Where should the nerve be sacrificed in relation to the dorsal root ganglion?
A. Proximal to the dorsal root ganglion
B. Distal to the dorsal root ganglion
2. The benefits of the lateral extracavitary approach include:
A. Circumferential neural decompression can be achieved under direct visualization.
B. Single-stage ventral and dorsal column support can be achieved using the same incision.
C. Both A and B
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







