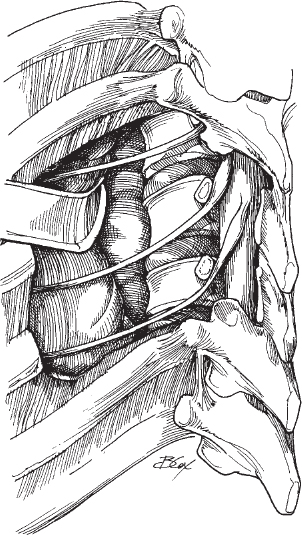
26 Howard B. Levene and Jack I. Jallo The lateral extracavitary approach has been developed to approach the posterior lateral and anterior lateral aspects of the spine and dura without the need of an anterior thoracic or abdomen exposure. The approach allows the surgeon to manipulate instruments in a direction away from the dura. The lateral extracavitary approach was originally developed for Pott’s disease but has proven effective for diskectomy, vertebrectomy, biopsy, and fusion. This approach affords the spine surgeon visualization of the posterior lateral and anterior lateral vertebral body. If a corpectomy is performed, the surgeon can visualize the posterior lateral and anterior lateral dural surfaces. The surgeon can perform a diskectomy, vertebrectomy, biopsy, or fusion with instrumentation through one incision. If posterior instrumentation (i.e., thoracic pedicle screws) is desired, the incision allows the additional placement of instrumentation. The surgical approach is technically challenging. The procedure requires expertise, experience, and a comfortable knowledge of thoracic and retroperitoneal anatomy. A lateral extracavitary approach is indicated for anterolateral dural compression. Compression may arise from trauma, neoplasm, infection, or degenerative changes. The approach is ideal when an anterolateral decompression is necessary to perform a vertebrectomy, diskectomy, biopsy, and or fusion. Patients who have had thoracic or pulmonary trauma or cardiopulmonary limitations may not be good candidates for any type of surgical intervention. Patients with severe abnormalities of the ribcage or spine (e.g., severe scoliosis) are less than ideal candidates for an extracavitary approach. Exposure at the limits of the approach (T1–T5 and L5-S1) is difficult. For lower lumbar dissections, dissection of the lumbar nerves off the iliopsoas muscle is required. The artery of Adamkiewicz has an unpredictable origin. Preoperative spinal angiography may be considered. Approaching the spine from the contralateral side to the artery of Adamkiewicz may be desirable. The fascia of the middle to lower thoracolumbar spine forms an aponeurosis, which when incised to expose the erector spinae muscle, often creates a large potential space. The space must be closed meticulously to prevent seroma formation. For exposure of a single vertebrae, the ribs above and below must be excised. The operating table may be angled to provide better visualization. It is important, therefore, to make sure the patient is well secured to allow rotation. When nerve roots are encountered, gentle retraction using vessel loops are useful. Tracing intercostal nerves/arteries back to the dura will identify the pedicles above and below the entrance to the foramen. Neuroelectrophysiology (somatosensory evoked potential [SSEP], motor evoked potential [MEP]) monitoring is highly advisable as an early-warning method for neural irritation. When planning for anterior grafting, it is advisable to leave the posterior cortex intact, if possible, to protect the dura. Close consultation with the anesthesiologist is required. Some authors have recommended single-lumen intubation with high-frequency ventilation. Prior to closure, fill the wound with saline to inspect for a pneumothorax or air leaks. The approach has limits depending on the level of the spine. The confines of the upper thoracic spine include the narrowing of the thoracic inlet, and the presence of great vessels, mediastinum, and lung apices. At the middle to low thoracic spine, the diaphragm is an impeding anatomic structure. Anatomic constraints in the lumbar spine include the abdominal viscera, kidneys, and great vessels. Unique anatomic challenges of the lumbosacral junction include the narrow pelvic inlet and the iliac vessels. During dissection, dividing the intercostal nerves distally allows better access to the foramen. Dividing the intercostal nerves creates a tolerable band of hypesthesia and avoids a dysesthetic pain syndrome from stretch injuries. Some difficulties inherent in the procedure include persistent bleeding, which may require fresh frozen plasma (FFP) if there is greater than 2 L of blood loss. The anesthesiologist must be alerted to the possibility of lung intubation. Central IV access or large-bore IV access and an arterial line are recommended. For nononcologic cases, Cell-Saver is recommended. The patient may be positioned on chest rolls and secured tightly. The ipsilateral chest roll can be placed medially to allow the scapula to fall away for high thoracic approaches. Depending on the levels to be approached, consider a Mayfield pin frame versus face pad support. Create a midline curvilinear hockey-stick skin incision three segments above and below the target level for a corpectomy and fusion. For a diskectomy, only 1.5 segments above and below the target level are required for adequate exposure. Alternatively a para-median linear incision can be used for exposure. For autograft, the incision is extended to the lateral crest for bone harvesting. The exposure allows visualization of the spinous processes, laminae, and transverse processes. There will be aponeurotic attachments at the transverse process. Dissect laterally to find the lateral margin of erector spinae muscles and retract the superficial soft tissues medially. For exposure up to C7, identify and separate the fascial planes of the trapezius and rhomboids and reflect them laterally as a myocutaneous flap. For exposure of the lateral thoracic or thoracolumbar junction, rib removal is required frequently at and below the vertebral level of interest. The rib may be dissected in its entirety (subperiosteal circumferentially) or dissected as a vascularized bone graft with preservation of the neurovascular bundle. During dissection, identify nerves and tag them with vessel loops. Intercostal nerves may be sacrificed proximal to the dorsal root ganglion for exposure (Fig. 26.1).
Lateral Extracavitary Approach
Description
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








