Figure 2.1 Main sites of neurological disorders
MOTOR SYSTEM
CNS
The motor system in the CNS consists of the brain and spinal cord, beginning in the motor cortex and extending down the brain stem and spinal cord to end at the lower border of L1. The motor tract begins in the frontal lobe, descends via the corona radiata on the same side to become the internal capsule. It then descends into the brain stem as the pyramidal tract and mostly (85%) crosses at the lower end of the medulla to the opposite side. From there it descends into the spinal cord as the lateral corticospinal tract and finally synapses with the anterior horn cells at the front (anterior) of the spinal cord on the same side (Fig. 2.2). A lesion anywhere along this pathway in the brain or spinal cord results in an upper motor neurone lesion (UMNL). The neurological signs of an UMNL are loss of power, increased tone (hypertonia), clonus, increased reflexes (hyper-reflexia) and extensor plantar response (up going toes or Babinski sign). The presence of these signs localise the site of the lesion to the CNS. The main UMN disorders presenting with these signs are hemiplegia arising from lesions in the brain and quadriplegia arising from lesions in the brain stem. The other main UMN disorders are quadriplegia and paraplegia arising from the spinal cord depending on the level of the lesion.
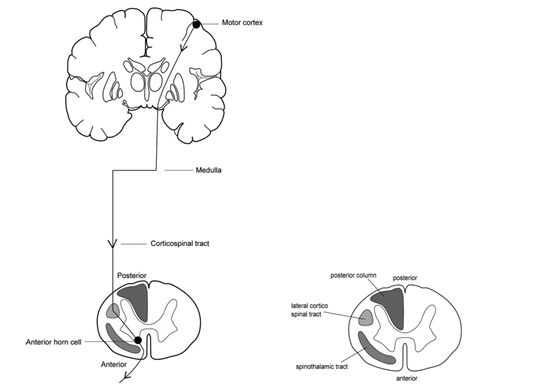
Figure 2.2 The corticospinal tract (left). Spinal cord section. Main motor and sensory tracts (right).
PNS
The motor system in the PNS consists of cranial and peripheral nerves, extending from their nerve nuclei in the brain stem and anterior horn cells in the spinal cord to the neuromuscular junction in muscle (Fig. 2.3). A lesion anywhere along this pathway is called a lower motor neurone lesion (LMNL). The neurological signs of a LMNL are loss of power, muscle wasting, fasciculation, decreased tone (hypotonia) and decreased or absent reflexes (hyporeflexia or areflexia). The presence of LMN signs localise the site of the lesion to the peripheral nervous system. The main clinical disorders causing these signs are peripheral neuropathies, mononeuropathies and cranial nerve palsies.
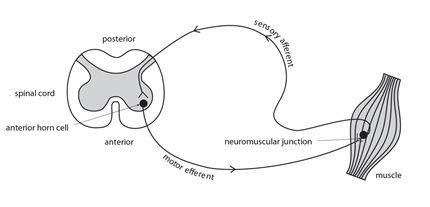
Figure 2.3 The peripheral reflex pathway
The diagram “the peripheral reflex arc” outlines the pathway of a peripheral reflex. It is essential to be able to distinguish clinically between an UMNL and a LMNL, in order to be able to correctly localise a neurological disorder to its main site of origin. It is important to note that loss of power is common to both and therefore does not help to distinguish between them, and that these signs may not all be present in any one individual patient. The main differences between them are summarized in the Table 2.1 below.
Table 2.1 Key differences between UMNL & LMNL
| Neurological findings | UMNL* | LMNL* |
| wasting | yes | |
| fasciculations | yes | |
| tone increased decreased clonus | yes yes | yes |
| reflexes increased decreased/absent | yes | yes |
| Babinski sign | yes |
* a blank space means no
SENSORY SYSTEM
The sensory system comprises of nerves and tracts which carry stimuli arising from the periphery including skin, joints, muscle and viscera via the peripheral nervous system (PNS) to the brain. In the CNS there are two main sensory pathways, the dorsal columns and the spinothalamic tracts (Fig. 2.4). The dorsal columns transmit joint position sense, vibration sense and light touch. The peripheral nerves transmitting these sensations enter via enter the posterior roots of the spinal cord and ascend in the dorsal columns to the lower end of the medulla, where they synapse. They then cross the midline and ascend to reach the thalamus, from where a further relay goes to the sensory cortex in the parietal lobe of the brain on the same side. Sensory symptoms arising from the posterior columns are numbness, tingling and loss of co-ordination. The spinothalamic tract transmits pain, temperature and crude touch. These enter the posterior spinal cord ascend a few segments, and then cross the midline to ascend in the anterolateral spinothalamic tract via second order neurones to the ipsilateral thalamus, and finally to the parietal lobe on the same side. The main sensory symptoms arising from disorders of the spinothalamic tract are pain and dysaesthesia. Sensory symptoms arise from disease at different levels in the nervous system. The main sensory sites of clinical interest are at the level of peripheral nerves, spinal cord and brain.
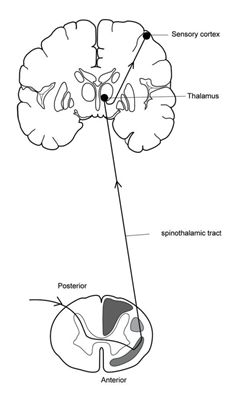
Figure 2.4 The spinothalamic tract (left).
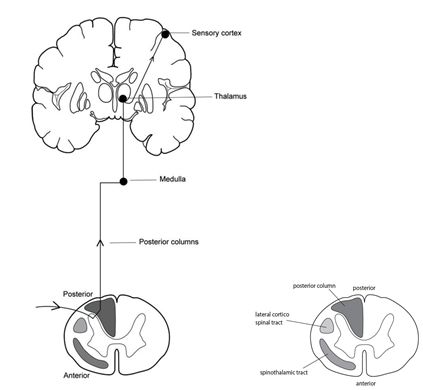
Figure 2.4 Spinal cord section. Main motor and sensory tracts (right). The posterior columns (left).
The anatomical pattern of sensory loss helps to localise the site of the underlying disorder. The main patterns of sensory loss are outlined in the following figures 2.5–7.
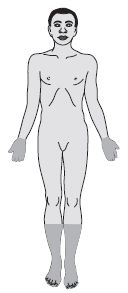
Figure 2.5 Sensory loss in peripheral neuropathy glove and stocking distribution (left)
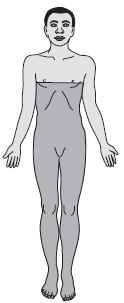
Figure 2.6 Sensory loss in paraplegia (right)
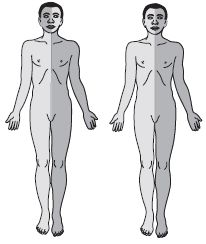
Figure 2.7 Sensory loss in brain stem lesion (left). Sensory loss in hemiplegia (right).
In peripheral nerve disorders the most common pattern of loss is that seen in peripheral neuropathies where the loss is mainly distal and affects the feet and hands in a glove and stocking distribution. The main causes of this are HIV and diabetes mellitus.
In spinal cord disorders the loss involves the limbs (usually the legs) and the trunk below the level of the lesion. The extent and pattern of loss depends on the underlying lesion, e.g. complete or partial cord involvement resulting in paraplegia. The main causes are trauma and infection.
In brain disorders sensation is lost or more commonly altered on the side of the body opposite the site of lesion. The main causes are vascular and space occupying lesions.
CEREBRAL HEMISPHERES
The brain has two hemispheres, each containing a frontal, parietal, temporal and occipital lobe, each lobe with their own distinctive functions. The main neurological signs indicating a lesion on one side of the brain are a loss of power or less frequently sensation on one side of the body, a loss of speech if the dominant hemisphere is involved and a loss of vision to one side if the optic pathway is involved. The presence of these focal neurological signs help to localize the site of the lesion to a cerebral hemisphere on one side and also to an individual lobe within that hemisphere (Fig. 2.8).
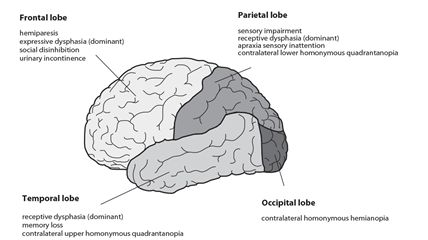
Figure 2.8 Cerebral hemispheres
Frontal lobe
The frontal lobe contains the motor cortex, which is responsible for motor function and movements of the opposite half of the body. Disorders affecting either frontal lobe result in weakness or a loss of power involving the opposite side of the body and also a loss or impairment (dysphasia) of speech (aphasia, expressive), if the speech area (Broca’s area) in the dominant hemisphere is affected. Personality changes with features of social disinhibition and urinary incontinence may also occur. Frontal lobe release signs, including the grasp reflex may also be present.
Parietal lobe
The parietal lobe contains the sensory cortex whose main function is discriminatory sensation involving the opposite half of the body. Patients with lesions in the parietal lobe have subtle sensory impairments, which require higher sensory testing to demonstrate. They have an inability to recognise familiar shapes, textures and numbers and an impairment of fine touch when tested on the opposite hand on either side. Lesions involving the dominant hemisphere result in difficulty with calculation, writing and apraxia (difficulty performing task related movements) and a receptive dysphasia if the dominant hemisphere is affected (Wernicke’s area). Lesions involving the non dominant hemisphere result in a lack of visuo-spatial awareness with hemineglect of the opposite side of the body. This can result in an inability to dress or wash on the affected side. A lesion in either parietal lobe may result in an inferior quadrantic visual field defect or a loss of the lower half of the visual field coming from the opposite side.
Temporal lobe
The temporal lobe contains Wernicke’s receptive speech area in the dominant hemisphere. Damage to it results in loss of understanding of speech and writing (aphasia, receptive) and loss of memory. Seizures originating in the temporal lobe may begin with a characteristic hallucinatory prodrome of smell, taste, vision, hearing or emotion. A lesion in either lobe may result in a superior quadrantic visual field defect or loss of the upper half of the visual field coming from the opposite side.
Occipital lobe
The occipital lobe is responsible for vision. Lesions of the occipital lobe may result in a contralateral homonymous hemianopia or loss of the visual field coming from the opposite side.
SPEECH DISORDERS
There are three main types of speech disorder: dysphonia, dysarthria and dysphasia.
Dysphonia
This is a disorder of voice production of sound as air goes through the vocal cords. It results in inability to produce a normal volume of speech or sound. It is usually recognized during the history taking, because the sound the voice generates is low, hollow or hoarse. It arises from failure of adduction of the vocal cords due either to paralysis or to local disease in the larynx. It can be suspected by asking the patient to cough, when instead of the normal sharp explosive cough there is a characteristic husky or bovine like cough. The diagnosis is confirmed by inspection of the larynx and vocal cords. The main causes are a local lesion e.g. a tumour, recurrent laryngeal nerve paralysis, and myasthenia gravis.
Dysarthria
This is an inability to coordinate the movements of tongue, lips and pharynx to articulate or produce understandable sounds. This makes words sound slow and slurred and leads to difficulty in their understanding. Any neurological disorder which affects the muscles or movements involved in speech production can produce a dysarthria. The main causes are stroke, cerebellar disease, and cerebral palsy.
Dysphasia
This is a disorder of language production resulting in either a loss of understanding or expression of words or both. It arises because of damage to the speech areas in the brain in the dominant hemisphere. The main speech centres are situated on the left side of the brain in >90% of right handed people and also in about two thirds of left handed people. Dysphasia and aphasia are clinically classified as either receptive, expressive or global.
Key points
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








