Chapter 7 Lower Limb Blocks
 Unlike the upper extremity, the entire lower extremity cannot be anesthetized with a single injection.
Unlike the upper extremity, the entire lower extremity cannot be anesthetized with a single injection. The lumbosacral plexus from a functional point of view comprises two distinct entities: the lumbar plexus and the sacral plexus.
The lumbosacral plexus from a functional point of view comprises two distinct entities: the lumbar plexus and the sacral plexus. This functional distinction frequently requires the performance of two separate blocks, increasing the requirement for local anesthetic and hence the likelihood of systemic toxicity.
This functional distinction frequently requires the performance of two separate blocks, increasing the requirement for local anesthetic and hence the likelihood of systemic toxicity. Because of overlying muscle and connective tissue, injections are generally deeper than those required for the upper limb.
Because of overlying muscle and connective tissue, injections are generally deeper than those required for the upper limb. Not surprisingly, ultrasonography has helped increase block success rates, performance times, and onset times for lower limb blocks.
Not surprisingly, ultrasonography has helped increase block success rates, performance times, and onset times for lower limb blocks. Ultrasonography helps identify anatomical variation in individual patients and reduces the incidence of vascular puncture.
Ultrasonography helps identify anatomical variation in individual patients and reduces the incidence of vascular puncture. Nerve imaging can be technically challenging in the lower limb; low-frequency ultrasound probes are needed for deep structures.
Nerve imaging can be technically challenging in the lower limb; low-frequency ultrasound probes are needed for deep structures. Stimulating catheters for continuous femoral nerve block are associated with decreased postoperative visual analog scale (VAS) scores.
Stimulating catheters for continuous femoral nerve block are associated with decreased postoperative visual analog scale (VAS) scores. Lower limb blocks may impair the patient’s ability to mobilize safely, increasing the likelihood of falls and injuries. Patient suitability, type of surgery, and day case or overnight stay all impact the choice of block (or not) to be performed.
Lower limb blocks may impair the patient’s ability to mobilize safely, increasing the likelihood of falls and injuries. Patient suitability, type of surgery, and day case or overnight stay all impact the choice of block (or not) to be performed. Lower limb surgeries frequently require the use of tourniquets; the combination of direct local anesthetic neurotoxicity, tourniquet-induced ischemia, or crush injury, together with patient factors such as diabetes, must be considered on an individual patient basis with regard to the potential for neurological injury.
Lower limb surgeries frequently require the use of tourniquets; the combination of direct local anesthetic neurotoxicity, tourniquet-induced ischemia, or crush injury, together with patient factors such as diabetes, must be considered on an individual patient basis with regard to the potential for neurological injury. The estimated distance from the skin to the lumbar plexus is 8.35 cm (range, 6.1–10.1) in men and 7.1 cm (range, 5.7–9.3) in women.4
The estimated distance from the skin to the lumbar plexus is 8.35 cm (range, 6.1–10.1) in men and 7.1 cm (range, 5.7–9.3) in women.4 The distance from the transverse process to lumbar plexus is consistently less than 2 cm in studies.4
The distance from the transverse process to lumbar plexus is consistently less than 2 cm in studies.4 The femoral nerve frequently divides in the proximal thigh; the practitioner should scan more cephalad if it is difficult to identify.
The femoral nerve frequently divides in the proximal thigh; the practitioner should scan more cephalad if it is difficult to identify. The anterior division of the femoral nerve supplies a motor branch to sartorius muscle. Medial and intermediate cutaneous branches supply the skin of the medial and anterior surfaces of the thigh.
The anterior division of the femoral nerve supplies a motor branch to sartorius muscle. Medial and intermediate cutaneous branches supply the skin of the medial and anterior surfaces of the thigh. The anterior division is most likely to be stimulated first, so the needle should be moved lateral and slightly deeper to stimulate the posterior division.
The anterior division is most likely to be stimulated first, so the needle should be moved lateral and slightly deeper to stimulate the posterior division. The minimum local anesthetic volume to produce successful block in 50% of patients is 14 to 16 mL of 0.5% bupivacaine and ropivacaine, respectively.
The minimum local anesthetic volume to produce successful block in 50% of patients is 14 to 16 mL of 0.5% bupivacaine and ropivacaine, respectively. The distance from the anterior superior iliac spine to the pubic tubercle is consistently 12 to 15 cm.
The distance from the anterior superior iliac spine to the pubic tubercle is consistently 12 to 15 cm. There is a low chance of vascular injury given block anatomy even with the double-pop or “blind” technique.
There is a low chance of vascular injury given block anatomy even with the double-pop or “blind” technique. Asking the patient to cough increases intraabdominal pressure, resulting in retrograde expulsion of local anesthetic from the needle hub and confirming correct fascial plane location.
Asking the patient to cough increases intraabdominal pressure, resulting in retrograde expulsion of local anesthetic from the needle hub and confirming correct fascial plane location. Deposition of local anesthetic in interfascial planes results in a greater than 90% success rate without the need for muscle stimulation as an end point.
Deposition of local anesthetic in interfascial planes results in a greater than 90% success rate without the need for muscle stimulation as an end point. Obturator block reduces opioid consumption and pain scores in patients undergoing major knee surgery.
Obturator block reduces opioid consumption and pain scores in patients undergoing major knee surgery. The posterior approach described by di Benedetto et al38 is associated with a low degree of patient discomfort during block performance for sciatic nerve block in the thigh.
The posterior approach described by di Benedetto et al38 is associated with a low degree of patient discomfort during block performance for sciatic nerve block in the thigh. More proximal approaches to the sciatic nerve are more likely to result in blockade of the posterior cutaneous nerve of the thigh, providing an advantage for procedures above the knee.
More proximal approaches to the sciatic nerve are more likely to result in blockade of the posterior cutaneous nerve of the thigh, providing an advantage for procedures above the knee. Popliteal fossa block anesthetizes the entire leg below the tibial plateau except the skin on the medial aspect of the foot and calf (saphenous nerve).
Popliteal fossa block anesthetizes the entire leg below the tibial plateau except the skin on the medial aspect of the foot and calf (saphenous nerve). If using a blind technique, saphenous paravascular injection greatly increases the chances of a successful block.
If using a blind technique, saphenous paravascular injection greatly increases the chances of a successful block. The saphenous nerve provides sensation to the medial aspect of the ankle and leg and may need to be blocked separately.
The saphenous nerve provides sensation to the medial aspect of the ankle and leg and may need to be blocked separately. If the saphenous nerve cannot be identified using ultrasonography, perivenous ultrasound-guided injection of local anesthetic is associated with a higher success rate than blind injection alone.
If the saphenous nerve cannot be identified using ultrasonography, perivenous ultrasound-guided injection of local anesthetic is associated with a higher success rate than blind injection alone. Epidural spread of local anesthetic is a common side effect with contralateral spread occurring in 9% to 16% of patients.
Epidural spread of local anesthetic is a common side effect with contralateral spread occurring in 9% to 16% of patients. High volumes of local anesthetics are injected into a vascular compartment. If a supplemental or subsequent lower limb block is added, local anesthetic toxicity can become an issue. This has been reported in older patients.
High volumes of local anesthetics are injected into a vascular compartment. If a supplemental or subsequent lower limb block is added, local anesthetic toxicity can become an issue. This has been reported in older patients. The obturator nerve is less frequently anesthetized than the lateral femoral cutaneous nerve when the classical three-in-one block is attempted.
The obturator nerve is less frequently anesthetized than the lateral femoral cutaneous nerve when the classical three-in-one block is attempted. The accuracy of catheter placement for continuous techniques is important, stimulating catheters result in consistently higher success rates. Motor responses at 1 mA (using the catheter) or less are associated with lower median VAS scores.
The accuracy of catheter placement for continuous techniques is important, stimulating catheters result in consistently higher success rates. Motor responses at 1 mA (using the catheter) or less are associated with lower median VAS scores. A motor response may be frequently difficult to illicit and often absent; when a response is elicited below 0.5 mA, intraneural needle placement is likely for this block.
A motor response may be frequently difficult to illicit and often absent; when a response is elicited below 0.5 mA, intraneural needle placement is likely for this block. Stimulation-only popliteal fossa blocks are better tolerated although less successful than classical higher approaches to the sciatic nerve.
Stimulation-only popliteal fossa blocks are better tolerated although less successful than classical higher approaches to the sciatic nerve.Lumbar Plexus Block
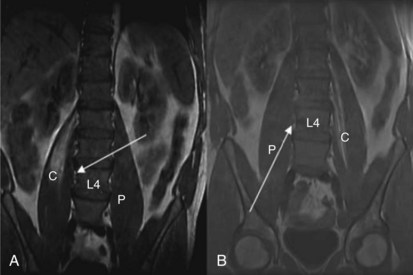
The anterior rami of T12-L4 form the lumbar plexus. The lumbar nerve roots emerge from the intervertebral foramina and immediately enter the body of the psoas muscle; divide into anterior and posterior divisions; and reunite as they course through the muscle to form the ilioinguinal, genitofemoral, lateral femoral cutaneous, femoral, and obturator nerves. The psoas muscle is enclosed in a fascial sheath continuous superiorly with the thoracic fascia, limited medially by the bodies of the lumbar vertebrae and posteriorly by the transverse processes, ligaments, and quadratus lumborum. Many approaches to the psoas compartment have been described, but probably the best known are those of Winnie and Capdevila. Both have an inferior (L4, L5) needle entry point and both result in spread of local anesthetic within the psoas compartment superiorly to L1 (Fig. 7-1).1
Winnie (1974) described the first posterior approach to the lumbar plexus and its subsequent modification with the use of nerve stimulation.2 Bilateral blockade, however, and concurrent epidural and spinal anesthesia occurring with the block led to concerns about its use.3 Capdevila, among others, proposed a number of modifications to the original description, designed to reduce the incidence of bilateral block (reportedly 10% to 20%).4 Capdevila reported a reduction in the incidence of bilateral block to 2%. Mannion et al5 compared both the Winnie and Capdevila approaches and randomized 60 elderly patients having lower limb arthroplasty to either technique for postoperative analgesia. Twelve patients in the Winnie group (40%) and 10 patients in the Capdevila group developed contralateral spread with many having evidence of bilateral thoracic and lumbar dermatomal spread (eight and five, respectively). Postulated reasons for bilateral spread have included (1) puncture of the epidural sleeve of the femoral nerve,6 (2) medial needle orientation leading to direct epidural or subarachnoid spread,4 and (3) spread occurring anterior to the vertebral bodies via areolar connective tissue within the subserous fascial layer as has been previously described to occur in the thorax.7 Gadsden et al8 recently demonstrated evidence of bilateral femoral nerve block or neuraxial anesthesia in six and five of 10 study patients, respectively, when injection pressure exceeded 20 psi. Neither effect occurred in 10 other patients randomized to injection pressure less than 15 psi when 35 mL of mepivacaine was injected. This appears to support the hypothesis that local anesthetic administered under high pressure causes extensive cleaving of tissue planes within the psoas muscle. Presumably, this opens up channels through which local anesthetic approaches the intervertebral foramina.
Clinical Utility
Perhaps more so than any other lower limb block, the clinical utility of a psoas compartment block in an individual patient must be weighed against the potential for the complications already discussed. A retrospective study by Macaire et al9 offers an insight into the incidence of such complications in clinical practice. The study itself involved 42 teams from the United States, Canada, France, Belgium, and Switzerland. In all, 4319 posterior lumbar plexus blocks were reported. Teams declared a 1% to 10% incidence of epidural spread, 11 total spinal anesthetics with one resulting death, 13 intravascular injections with three resulting seizures and one cardiac arrest, four delayed toxic reactions, and 13 incorrect catheter paths. Given the retrospective nature of this report, these figures may well be underestimated.9 A recent meta-analysis evaluated psoas compartment anesthesia for lower extremity surgery.10 Thirty studies were included, and the authors concluded that although psoas compartment block was superior to opioids for postoperative analgesia (providing 13 hours of analgesia after a single-shot block), there was insufficient data to recommend this approach as the sole anesthetic for hip or major knee surgery.10 Conversion rates to general anesthesia were typically in the order of 20% to 25%.
Landmark Technique for Psoas Compartment Block
The Capdevila approach to the psoas compartment block is outlined here because studies in general report lower incidence of bilateral spread. Venous access and standard monitoring (oxygen saturation, electrocardiography, and noninvasive blood pressure monitors) are secured. Because this is a deep block, patient discomfort can be a problem. It is our practice to administer fentanyl 0.5 to 1 µg/kg and 1 to 2 mg of midazolam if required. The patient is positioned in the lateral decubitus position with a slight forward tilt. The side to be blocked is uppermost. Both thighs are flexed, though the foot of the uppermost leg should be positioned over the dependent leg for ease of visibility. The spinous process of L4 is identified as the point at which the intercristal (Tuffier’s) line intersects the vertebral column. The posterior superior iliac spine is identified by palpation. From this point, the practitioner draws a line parallel to the spinous process extending cephalad. The practitioner draws out the intercristal line; this intersects with the line originating at the posterior superior iliac spines. The needle puncture point is at the junction of the lateral one third and medial two thirds of the line joining L4 and the line passing through the posterior superior iliac spine. At a minimum, an 80- to 100-mm insulated stimulating needle is needed for this block, and the stimulating current is set at 1.0 mA, 2 Hz, and 0.1 msec. The needle is oriented perpendicular to the skin and advanced until the transverse process of L4 is encountered. The needle is then directed caudally and advanced no more than 20 mm until a quadriceps muscle twitch is seen.11
Ultrasound-Guided Technique of Psoas Compartment Block
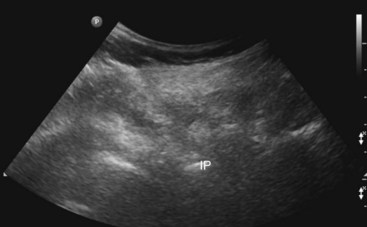
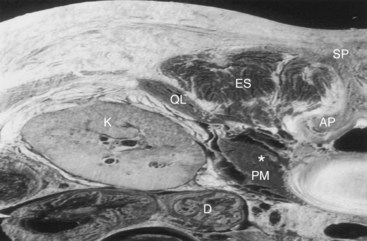
The patient is positioned similar to that used for the landmark approach. A low-frequency 2- to 5-MHz curved array transducer is used. It is our practice to begin by identifying the sacrum and turning the probe through 90 degrees to image the facet joints of the lumbar vertebrae: L3, L4, and L5. The transducer (with the long axis of the probe parallel to the lumbar spine) is moved laterally to identify the transverse processes of L3, L4, and L5. The hyperechoic transverse processes with the resulting acoustic shadow produce a characteristic “trident sign” shown in Fig. 7-2.12 The ultrasound machine settings (focal zones, depth of the scanning plane, and far-field gain) are now optimized. The psoas muscle has a striated appearance; although the lumbar plexus can be identified with ultrasonography, we have found this difficult to achieve in our adult practice.11 Local anesthetic (lidocaine 2%) is used to infiltrate the skin and deeper structures. The stimulating needle is introduced along the long axis of the probe in plane from cephalad to caudad (Fig. 7-3). We believe this approach is less likely to result in damage to structures such as the lower pole of the kidney (Fig. 7-4). The needle tip is angled away from the intervertebral foramina. In performing this block, it is frequently difficult to identify the needle shaft because of the curved array and angle of needle approach. Its position can often only be inferred from tissue movement around the needle when it is rocked side to side or gently probed forward. Entry of the needle into the posterior part of the psoas muscle results in contraction of the psoas muscle seen on the ultrasound screen. The needle is advance slowly to elicit femoral nerve stimulation (patellar twitch) not to be mistaken with hip flexion caused by psoas contraction. After negative aspiration, 10 mL of the local anesthetic solution is slowly injected. Further aspiration after each 10 mL is injected is advisable. It is our practice to use 20 to 30 mL of 0.5% ropivacaine solution. It should be pointed out that in obese patients, because of the technical limitations of ultrasonography, it can be frequently difficult to identify the psoas muscle and associated anatomy.13 It is thus up to the individual practitioner whether to abandon the procedure or attempt to perform it using stimulation alone.

Fig. 7-3 The same sonogram as in Fig. 7-2. The dashed line shows the current needle trajectory and needle tip position (NT) as it approaches the transverse processes (TP) of L4.
Femoral Nerve
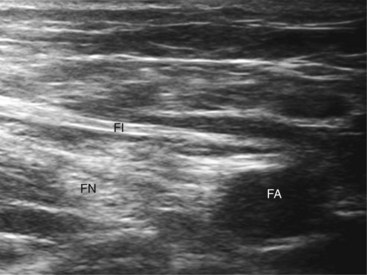
The femoral nerve is formed by the dorsal divisions of the anterior rami of the spinal nerves L2 to L4 as they condense within the psoas muscle. (Successful psoas compartment block results in almost 100% incidence of femoral nerve block.) The femoral nerve emerges from the lateral aspect of the psoas muscle at the junction of the middle and lower thirds and courses in the gutter between the psoas and the iliacus muscle lying inferior to the fascia iliaca. It enters the thigh when it passes inferior to the inguinal ligament. It lies deep to fascia lata and iliaca, lateral and at times somewhat posterior to the femoral artery (Fig. 7-5). At this level, the femoral nerve is rarely a single structure; rather, the nerve has rapidly divided into major anterior and posterior divisions. Other branches include the articular branch to the hip joint and branches to the rectus femoris, sartorius, and pectineus muscles. The anterior branches pierce fascia iliaca and supply sensory innervation to the anterior and medial aspects of the thigh. The posterior branches remain deep to fascia iliaca and innervate the quadriceps and the knee joint and terminate as the saphenous nerve, which supplies sensation to the medial aspect of the leg.
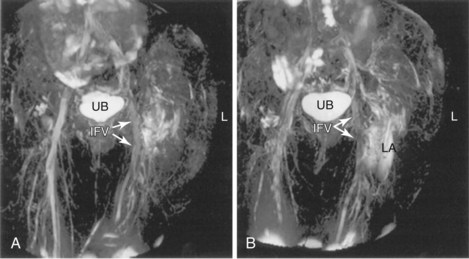
Winnie et al14 (1973) proposed the inguinal paravascular approach to the lumbar plexus (i.e., the three-in-one block), eliciting femoral nerve paresthesia at the level of the inguinal crease and using larger volumes of local anesthetic combined with pressure distal to the needle entry point. They described successful blockade of the femoral, ilioinguinal, and lateral cutaneous nerves simultaneously. Recent work has failed to demonstrate consistent block of all three nerves with high-volume local anesthetic injections. At least partial sensory blockade of the lateral femoral cutaneous nerve is achieved in almost all patients; the obturator nerve, however, is least likely to be blocked. In some series, the incidence of successful block is less than 10% irrespective of volume injected.15,16 This may be because of the medial location of that nerve at the inguinal crease level. Cephalad spread of local anesthetic to the lumbar plexus is limited on magnetic resonance imaging studies and does not appear to consistently occur to the extent postulated earlier by Winnie et al.14 Rather, the injectate spreads lateral, caudal, and slightly medial (Fig. 7-6).17
Ultrasound-guided femoral nerve block results in significantly faster sensory onset times over nerve stimulation alone (onset time, 16 minutes vs. 27 minutes using 20 mL bupivacaine 0.5%).18 Ultrasound guidance also significantly reduces the minimum effective anesthetic volume required for successful nerve block.19 A recent meta-analysis of 13 studies confirmed that regional blocks performed with ultrasonography were more likely to be successful, had faster onset, had on average a 25% longer duration of action, and took marginally less time to perform (1 minute). Perhaps of most importance, ultrasound guidance reduced the risk of vascular puncture by 80% in real terms (relative risk, 0.16; 95% confidence interval 0.05–0.47; P = .001).20 At our institution, we continue to use 20 mL of ropivacaine 0.5% as the standard bolus dose for ultrasound-guided analgesic blocks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree