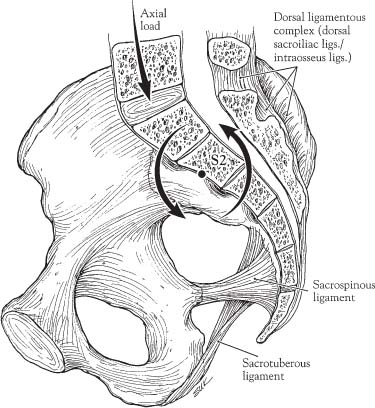
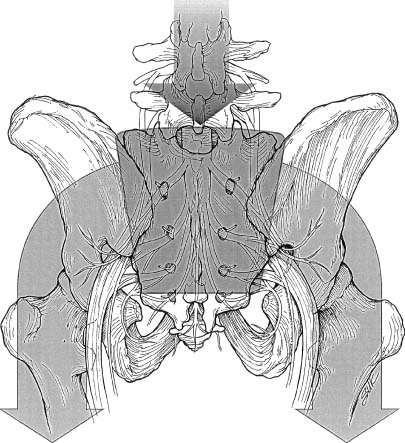
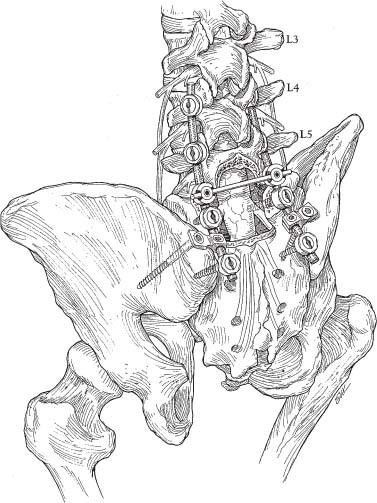
41 Biologic osseous union is the only reliable method of long-term spinal stabilization. Instrumentation provides stable fixation in a predetermined position until fusion occurs. Complex anatomic and biomechanical features of the lumbosacral region, coupled with the destructive nature of neoplastic processes and surgical resection, present challenging problems in terms of spinal stabilization. The lumbosacral junction represents a unique region of the spinal column. It is exposed to the largest loads encountered throughout the spine. Although it has the largest range of motion of any thoracic or lumbar level in the sagittal (flexion-extension) plane, it has the most limited range of motion of any spinal level in the axial plane and during rotation and lateral bending. Because of the normal lordotic curvature of the lumbar spine, the lumbosacral intervertebral disc possesses a steep angle with respect to the horizontal. The large load carried and the angular position of the sacrum result in unique load-bearing characteristics at the lumbosacral junction. In essence, the lumbosacral junction represents a transition area where the mobile lower lumbar segments meet the highly immobile sacrum and pelvis. The forward tilt of the sacrum causes the body load to be transmitted to the ventral surface of the sacrum as a potential rotatory force, with the axis centered at S2 (Fig 41-1). Ligamentous structures confer most of the stability at the sacroiliac joint. The dorsal ligamentous complex, including the interosseous and dorsal sacroiliac ligaments, is the strongest set of ligaments binding the sacrum to the ilium. These ligaments resist forward rotation at the upper end of the sacrum. The sacrospinous and sacrotuberous ligaments resist the tendency of the lower end of the sacrum and coccyx to rotate dorsally. Bony constraints offered by the wedgelike shape of the sacrum within the pelvis (Fig 41-2), and the interdigitating surfaces of the sacral alae with respect to the iliac bones provide additional resistance to sacral tipping. In the resection of sacral tumors, sacroiliac stability is affected little if the sacroiliac joints are left intact.1,2 Although the sacrospinous and sacrotuberous ligaments are often transected in lower sacral amputations, the dorsal ligamentous complex is preserved. Gunterberg et al1 evaluated pelvic strength after major amputations of the sacrum. Fifteen cadaveric pelvises were loaded to failure, composed of five unresected, five after resection of the sacrum between S1 and S2, and five after resection ~1 cm below the promontory. In these dissections, the second group (resections between S1 and S2) had about a third of the sacroiliac joint and the associated ligamentous structures resected. The third group (resection below the promontory) had about half of the sacroiliac joint and ligamentous structures removed. Weakening of the pelvic ring amounted to ~30% in the second group and 50% in the latter. In all of these experiments, the load to failure far exceeded physiologic loads. Based on their study, the authors concluded that weight bearing was safe for patients after sacral resection if 50% or more of the sacroiliac joint (corresponding to at least the upper half of the S1 segment) remained intact. Clinical reports have supported these conclusions.3–5 FIGURE 41-1 Rotational forces, centered at S2, act on the sacrum. These forces are largely counteracted by ligamentous structures. The dorsal ligamentous complex, including the interosseous and dorsal sacroiliac ligaments, resists forward rotation at the upper end of the sacrum. The sacrospinous and sacrotuberous ligaments resist dorsal tipping of the lower sacrum and coccyx. Some partial sacrectomies may involve the resection of a sacroiliac joint on only one side. Although such resections can be performed successfully without reconstruction, the patient may experience pain associated with proximal migration of the pelvis. Unless the contralateral joint is completely intact and there is no anterior pelvic deficiency, we believe that most cases require some form of fixation.6 Total sacrectomy results in complete dissociation of the spine from the pelvis and requires complex iliolumbar reconstruction for adequate mechanical support to preserve satisfactory walking ability. Although most authors recommend that reconstruction be performed,7–16 contrary views have been expressed.17,18 Edwards17 described two patients who did not undergo reconstruction after terminal resection of the spine for tumor. The patients were kept on rotating beds for 3 months while the lumbar spine gradually settled between the iliac bones. Edwards believed that the muscles and scar formation would act as a sling to achieve spinal stability. The patients were allowed to stand with the use of a brace and were able to function well and walk without pain. The long-term outcome of this procedure is unknown. FIGURE 41-2 “Keystone” configuration of the sacrum within the pelvis. Arrows demonstrate the transfer of weight from the spine to the pelvis and lower extremities. Methods of spinopelvic stabilization that have been used after the resection of lumbosacropelvic tumors can be classified into three main categories: those utilizing sublaminar devices, those utilizing sacral screw (or screw-plate) fixation, and those utilizing iliac rod (or iliac-screw) fixation. Sublaminar fixation techniques include the use of hooks, wires, or cables. These devices provide a dorsal tension band across the lumbosacral joint that resists flexion and lateral bending. Unfortunately, these methods of fixation do not provide substantial resistance to extension or torsional loads. Fusion rates similar to that achieved without internal fixation have been reported.19 In addition, the sacral laminae are often thin and inadequate to accommodate these devices. In many cases, the laminae are removed in the process of tumor resection, precluding the use of sublaminar fixation techniques. Sacral pedicle screws provide significantly increased rigidity as compared with sublaminar devices. The S1 pedicle is larger than other lumbar pedicles and can often be fitted with 7- to 8-mm screws. Additional bony purchase may be obtained if the screw penetrates the anterior S1 cortex or the superior end plate of S1. Medially directed S1 pedicle screws that are crosslinked and attached to rods create a triangulation effect, which greatly increases torsional stability and pullout resistance.20–23 Triangulation with an oblique orientation also causes less interference with the superjacent facet joint and allows more purchase with a longer screw.24 A method to enhance sacral fixation with screws is the placement of an additional pair of laterally directed bone screws into the sacral alae below the S1 level. This method provides a biomechanical advantage compared with a pair of S1 pedicle screws.21 Unfortunately, the bone of the ala is usually of low density, and purchase may be tenuous.25 Furthermore, the risk of neurovascular injury with laterally directed screws in this region must be kept in mind. Screw-plate devices such as the Tacoma plate (Sofamor-Danek, Memphis, TN) permit the insertion of multiple sacral screws and easily may be attached to the proximal lumbar component of the instrumentation. These plates act as a template for controlled insertion of laterally directed alar screws after placement of the S1 pedicle screws. S2 (or lower level) pedicle screws are often of little use because of the short length of the pedicle. Biomechanical testing has shown that pedicle screw placement below S1 does not enhance the security of fixation enough to warrant the use of pedicle screws.21 The thin sagittal dimension of the sacrum at lower levels increases the risk of penetration of its ventral surface with injury to the adjacent vascular and visceral structures. In addition, screws at lower sacral levels are often prominent and may tent the overlying skin. Sacral screw fixation may be sufficient when the fixation length is short (one or two levels) and instability is minimal. If a long instrumentation construct is placed, the sacral attachment is subjected to large cantilevered forces that can cause the screw to pull out.25 In addition, the pedicles, body, or ala of the sacrum may be involved with tumor, precluding the use of sacral screws. In these cases, more complex spinal-pelvic fixation methods, such as the modified Galveston technique, have been useful.12,16 A simple method of sacropelvic fixation involves the placement of long, variable-angle bone screws obliquely across the sacroiliac joint into the iliac bones (Fig 41-3). A tripod effect may be gained by combining the sacroiliac fixation with additional sacral fixation points.26 Although this technique is relatively simple to perform, its disadvantages include those related to the placement of pedicle screws caudal to the S1 segment, as described above. Allen and Ferguson from Galveston, Texas, first described this technique for the management of scoliosis,27 but it has since been used in a variety of disease states. The Galveston technique involves inserting an angled distal limb of the spinal fixation rod into the posterior iliac bones, just above the sciatic notch. Although the original description involved segmental spinal fixation with sublaminar techniques, we use lumbar pedicle screw fixation12 and place crosslinks between the rods (Fig 41-4).
Lumbosacral and Pelvic Reconstruction
 Biomechanics After Sacral Resection for Tumors: Indications for Lumbosacropelvic Fixation
Biomechanics After Sacral Resection for Tumors: Indications for Lumbosacropelvic Fixation
 Lumbosacral and Spinopelvic Fixation Systems
Lumbosacral and Spinopelvic Fixation Systems
Classification
Sublaminar Devices
Sacral Screws and Screw Plates
Bicortical Iliac Screw Fixation
Galveston Fixation and Related Techniques
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




