Chapter 163 Management of Far Lateral Lumbar Disc Herniations
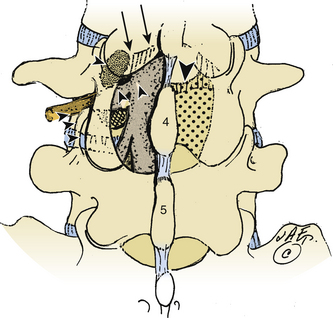
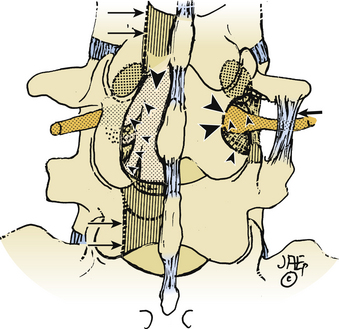
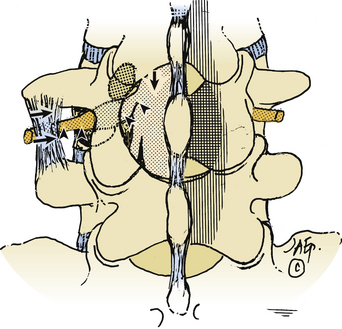
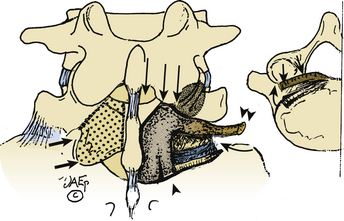
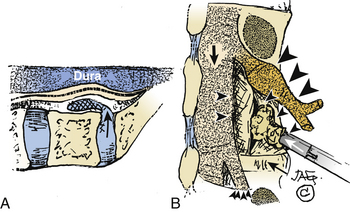
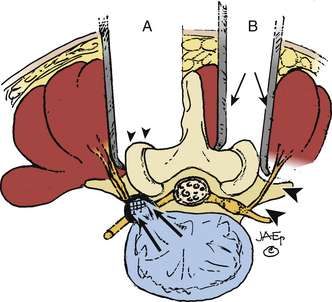
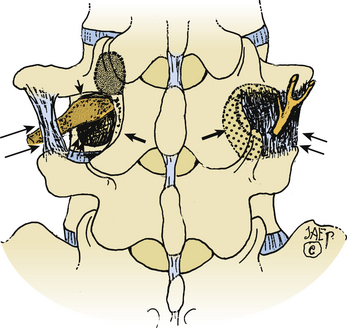
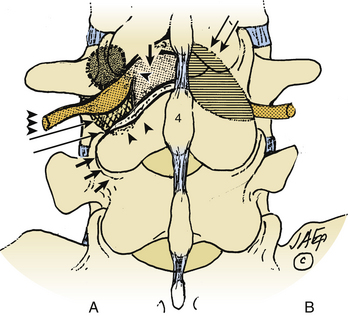
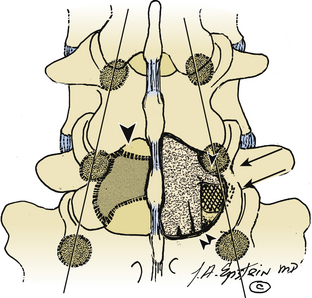
Far lateral disc (FLD) herniations account for between 6.5% and 12% of lumbar disc herniations.1–6 Operative resection techniques include minimally invasive procedures or microendoscopic alternatives, laminotomy, hemilaminectomy, and laminectomy with or without fusion (Figs. 163-1 to 163-9). The latter alternatives require differing degrees of facet resection depending on the location and complexity of the FLD and the accompanying degree and extent of spondylosis and stenosis. Minimally invasive techniques often include significant disruption of the ipsilateral pars and or facet joint, and they are typically performed with posterior lumbar interbody fusion and pedicle–screw instrumentation (open or percutaneous). Laminotomies and laminectomy decompressions rarely include just medial facetectomy or foraminotomy (possible only at the L5–S1 level) or the intertransverse approach, which are used primarily in younger patients who do not have significant attendant stenosis. Where patients have significant stenosis in conjunction with an FLD herniation, a single-level or multilevel laminectomy with focal full facetectomy are required along with non-instrumented and instrumented lumbar fusions. Alternatively, the extreme lateral approach performed either open or endoscopically removes little bone, thereby mitigating the requirement for fusion.
Attendant pathology can include foraminal, far lateral stenosis, degenerative spondylolisthesis, degenerative scoliosis, and/or limbus vertebral fractures. The type and extent of decompression and facet resection must be based on an individual patient’s pathology, because no single technique is universally appropriate.3 Clinical, neurodiagnostic, and surgical alternatives and outcomes for patients undergoing FLD surgery are reviewed.
Materials and Methods
Anatomy
Microdissection of more than 200 cadaver spines revealed that bony structures increasingly overlay the intervertebral foramen, resulting in less available space in the lateral and subarticular recesses as one progresses caudally in the lumber spine (see Figs. 163-1 to 163-9).7 Therefore, progressively more removal of medial bone from the pars interarticularis and facet joint are required at the lower lumbar levels to adequately expose the nerve root and ganglion. Typically, at the L5 and S1 level, where the interpedicular diameter is widest, almost no facet removal is required to expose the superiorly exiting nerve root as it extends into the foramen.
Cadaveric lumbar studies document that the foramen contains four distinct ligaments whose four bands extend radially from the nerve root sleeve.8 The first attaches posteriorly to the overlying facet capsule, two attach respectively to the superior and inferior pedicles, and the fourth is tethered to the disc annulus anteriorly. Additionally, a superolateral arterial arcade, which supplies the exiting nerve root, defines the vasculature of the extraforaminal compartment; to preserve this, dissection should be confined to its inferomedial aspect.9
Incidence and Location of Far Lateral Discs
Far lateral discs account for between 6.5% and 12% of all lumbar herniations and are typically sequestrated fragments found superolateral to the disc space of origin.1,3,10–16 In one series, FLDs were located foraminally (3%) or both intra- and extraforaminally (4%).17 FLD herniations compress the superiorly exiting nerve root and its dorsal root ganglion, producing deficits referable to the cephalad nerve roots. Thus, an FLD herniation at the L3–4 level contributes to L3 root compromise, and far lateral pathology at the L4–5 and L5–S1 levels contributes respectively to L4 and L5 root signs.
The majority of FLD herniations occur at the L3–4 or L4–5 levels, typically followed by L5–S1.2–4,11,14 FLDs rarely occur at the L5–S1 level, where the iliotransverse ligament provides excellent support if the L5 vertebra is located below the intercrestal line. More cephalad involvement at the L1–2 and L2–3 levels are rare, except in one study that cited a 28% incidence of FLDs at these cephalad sites.10 The location of 202 foraminal discs and FLDs in one series included the following levels: L1–2 (1 FLD), L2–3 (9 FLDs), L3–4 (48 FLDs), L4–5 (86 FLDs), and L5–S1 (58 FLDs).1
Clinical and Neurologic Parameters
Patients presenting with FLD herniations are typically in their mid-fifties (range, 19 to 78 years of age), with the ratio of male to female patients varying from 1:1 to 2:1.1–310 Severe radicular pain accompanies dorsal nerve root ganglion compression and inflammation in the far lateral compartment. Although the radicular pain is often excruciating and unremitting, the degree of back pain is significantly less. Patients with FLD compromising the femoral nerve roots (L2–4) complain of pain radiating into the hip, thigh, and medial aspect of the calf. Signs include a positive reverse Lasegue maneuver (femoral stretch test), iliopsoas and/or quadriceps weakness, a diminished or absent patellar response, and appropriate dermatomal sensory loss. As an example, the typical FLD at the L4–5 interspace compressing the L4 nerve root typically results in a positive femoral stretch test, weakness involving the tibial anticus and the extensor hallucis longus, a diminished Achilles response, and decreased pin appreciation in the L4 distribution. The more proximal location of complaints requires differentiation from intrinsic hip or knee pathology. X-ray and MR studies can identify intrinsic hip or knee disease, and arterial Doppler tests can help define whether vascular claudication is present.
Other Pathology Contributing to Far Lateral Root Compromise
Limbus Vertebral Fractures
Fractures of the vertebral limbus with or without lateral, foraminal, or far lateral stenosis or disc herniation can contribute to nerve root compression.18,19 There are four types of limbus vertebral fractures, I to IV. Type I fractures consist of a cortical rim separation of the posterior vertebral end plate, which extends across the full width of the disc space, resulting in central and foraminal stenosis. Type II fractures include both cortical and cancellous elements, with predominant midline intrusion on the thecal sac. Type III fractures are often found foraminally or far laterally, and may be noncalcified cartilaginous (III-A) or ossified (III-B). Type IV fractures involve the full sagittal length of the vertebral body, from one disc space to the next, and are often located centrally, resulting in significant thecal sac and nerve root compromise. Any of these fractures can arise from the cephalad or caudad vertebral end plates at any specified level.
Removal of limbus vertebral fractures located foraminally or far laterally often necessitates a full facetectomy to adequately expose the nerve root over its entire course.18 Resection first warrants removing the annulus from within the interspace. Next, morcellation of the bony limbus fracture is performed using a down-biting curette, tamp, and mallet technique, followed by delivery of these ossified fragments into the disc space cavity. Exposure for this type of decompression and resection may also be accomplished using microscopic endoscopic approaches with simultaneous fusion combining posterior lumbar interbody fusion and percutaneous pedicle screw instrumentation techniques. Nevertheless, manipulation and resection of the limbus fracture may be more readily and in many circumstances more safely accomplished with a larger exposure.
Stenosis and Spondylosis
Lumbar spinal stenosis and FLDs can coexist.8,12,19 In one series, FLDs were accompanied by stenosis, and surgical procedures were altered or extended in 72% of these older patients when magnetic resonance imaging (MRI) or noncontrast computed tomography (CT) studies were supplemented with myelo-CT examinations.2 An and colleagues similarly noted that 50 patients with FLDs and stenosis also required more extended decompressions.10 When Epstein reported on 857 patients undergoing surgery for lumbar stenosis, 40 patients demonstrated FLDs, and 5 exhibited far lateral stenosis.12,13,19
Degenerative Spondylolisthesis
Grade I degenerative spondylolisthesis or olisthy is most often encountered at L4–5, followed in descending order of frequency by the L3–4, L2–3, and the L5–S1 levels.15,16,20 Grade I olisthy is defined by a 25% slip of the vertebral body width and is usually limited by a locking of sagittally oriented, hypertrophied posterior facet joints.20 Disc herniations are encountered between 4.3% and 20% of the time with degenerative spondylolisthesis.
FLD herniations occurring at the level of a slip require a full unilateral facetectomy with instrumented fusion to prevent progressive instability in patients younger than 65 years, but many older than 65 years may be managed successfully with in-situ posterolateral intertransverse fusion.3,15 Good to excellent results are cited in up to 80% of patients.
Spondylolisthesis with Spondylolysis
When spondylolysis accompanies spondylolisthesis, the exiting nerve root becomes maximally compressed beneath the mobile and fractured pars interarticularis. Here, safe removal of an extruded or sequestrated disc fragment requires exposure of the nerve root along its entire intracanalicular, foraminal, and extreme lateral course. Many of these patients require simultaneous instrumented fusions, by either open pedicle screw-and-rod constructs or endoscopic posterior lumbar interbody fusions with percutaneous application of instrumentation. Good to excellent outcomes are typically reported in 80% to 85% of cases.16
Neurodiagnostic Evaluations
Magnetic Resonance Scans
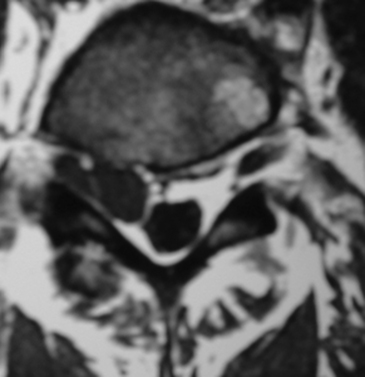
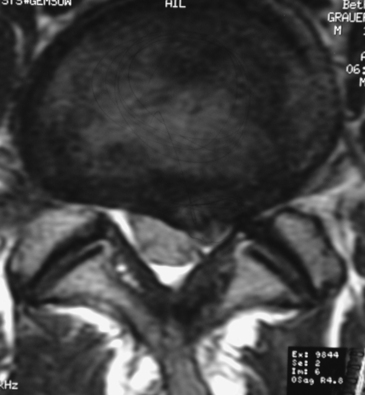
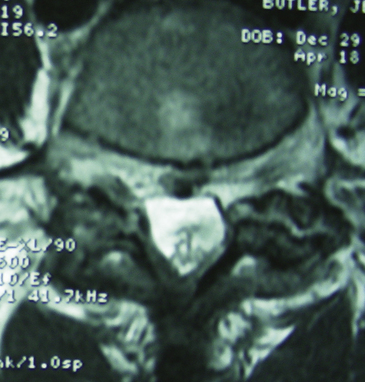
On MRI studies, far lateral soft disc herniations are located lateral to the pedicles and appear isointense or hypointense. Obliteration of the normally hypointense fat pad surrounding the dorsal root ganglion can signal the presence of an FLD herniation. Additionally, the presence of degenerative spondylolisthesis, spondylolisthesis and spondylolysis, or degenerative scoliosis can result in unilateral or bilateral foraminal or far lateral root compromise secondary to soft disc or calcified or ossified spondylosis. MRI studies document the multiple types of foraminal and far lateral nerve root compression (Figs. 163-10 to 163-12). However, CT better documents bony or ossified pathology, providing a direct hyperdense image, rather than the hypointense signal seen on MRI.
Gadolinium DTPA (diethylenetriamine-pentaacetic acid) enhanced MRI helps differentiate FLDs from other enhancing neoplasms.21 Postoperative enhanced MRI scans can distinguish between scar formation (enhancing) and recurrent disc herniations (nonenhancing).22
CT and Myelo-CT Scans
CT studies, with multiplanar reformations (two-dimensional to three-dimensional) or enhanced with iodine-based dyes, demonstrate foraminal and/or FLD herniations combined with spondylotic changes (Figs. 163-13 through 163-16).5,21 Soft FLDs can appear isodense, and accompanying limbus vertebral fractures, facet arthropathy, olisthy, and scoliosis appear hyperdense on CT-based studies. Additional intrathecal contrast used for myelo-CT studies better define central, lateral, and proximal foraminal stenosis. However, beyond the neural foramen, where the root is no longer invested with a subarachnoid sleeve, the addition of contrast does not provide any further imaging advantages. Noncontrast CT–based and myelo-CT studies better define the extent of stenosis when compared with MRI, and these added findings often significantly affect operative procedures performed in the elderly.2 Although CT discography can facilitate the demonstration of a far lateral lesion by revealing extravasation of dye far laterally, it is increasingly rarely used.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree