CHAPTER 209 Management of Severe Head Injury in Children
Pediatric traumatic brain injury (TBI) is a significant public health issue throughout the world. Although efforts at prevention and new safety technologies have led to a slight reduction in the rates of significant head injury in the United States, the rate of TBI is increasing in developing countries. TBI also remains the most common cause of death and disability in children in our country. In this review we discuss the background and epidemiology of pediatric TBI, followed by a review of management with use of a critical pathway. This pathway follows the 2003 “Guidelines for the Acute Management of Severe Traumatic Brain Injury in Infants, Children, and Adolescents,” a jointly sponsored guideline that addresses multiple facets of the management of severe brain injury in an evidenced-based fashion. In the guidelines, “standards” are accepted principles that reflect a high degree of certainty, “guidelines” reflect moderate clinical certainty, and “options” are strategies for which there is unclear clinical benefit.1
Background
Pediatric head trauma is an important public health issue with both high mortality and lifelong physical, cognitive, behavioral, and social implications. TBI accounts for 435,000 visits to the emergency department (ED), 37,000 hospital admissions, and approximately 2,500 deaths annually in the United States.2 These numbers do not include patients treated in offices or those who do not seek medical care for mild TBI.
The incidence of TBI is not consistent across sexes or age groups, with an overall male-to-female ratio of about 2:1. This gender difference does not start until after the age of 5; boys’ risk for TBI increases as they reach their teens, whereas girls’ risk declines after the age of 10.3 No group has a higher incidence of head injury than male adolescents aged 15 to 19, and only adults older than 75 years have a higher hospitalization rate.1 Studies have also shown that approximately 40% to 50% of all mortality after trauma is secondary to brain injury.4
Mild TBI is now being recognized in epidemic proportions. Ninety percent of patients with mild head injury (Glasgow Coma Scale [GCS] score of 13 to 15 and loss of consciousness for <30 minutes) seen in the ED are released.2,5 There are many more children who are never evaluated in the ED after a mild TBI. Although most obvious postconcussive symptoms improve within 1 month after injury and the majority of behavioral or attention problems resolve within 6 months after a mild head injury, a smaller subset of children will have prolonged symptoms.
Studies have shown that children with moderate (GCS score of 9 to 12) to severe (GCS score or 8 or less) head injuries are at significant risk for long-term problems with behavior and cognition. Although it had previously been thought that infants were at lower risk for long-term sequelae, it appears likely that the developing brain is even more susceptible to injury. Several recent studies have shown infants to have less positive acceleration in IQ than older children after similar head injuries and that children younger than 6 years had more difficulty in executive control and memory after head injuries than did older children. In addition, 40% of children have a persistent change in personality after severe head injury, and the incidence of behavioral problems correlates with increasing severity of head injury (36% in those with severe injury and 22% in those with moderate injury).6–12 Clearly, pediatric head injury is a significant public health issue not only in terms of the immediate hospitalization and health care costs but also with regard to the potential long-term implications on the neurocognitive development of these children.
Classification of Head Injuries
Hematomas
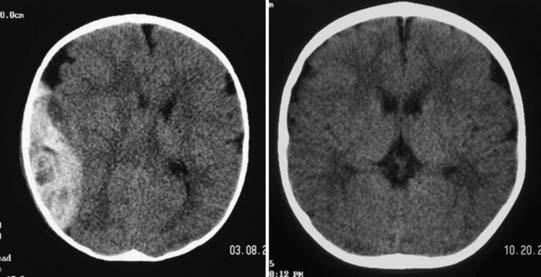
Epidural hematomas (EDHs) are collections of blood outside the dura that are usually arterial in origin, but they can be venous in up to 10% of patients. Very commonly, EDHs are associated with skull fractures, with the fracture resulting in an underlying injury to blood vessels. They often result from direct impact on the pterion of the temporal bone with the fracture injuring the middle meningeal artery, and they can enlarge rapidly and reach their peak size within 6 to 8 hours after injury. EDH forms a convex shape on imaging because the hematoma is contained by attachments of the dura to the skull at the cranial sutures. Classically, patients are described as having brief loss of consciousness initially because of a “concussive”-type injury, a lucid period during which the hematoma is expanding, and then neurological decline as intracranial pressure (ICP) increases. Unlike other head injuries, patients with poor GCS scores can have good outcomes postoperatively if there is no major concomitant brain injury and if the EDH is evacuated quickly. For patients with milder injuries and stable results on examination, it is possible that the EDH can be handled nonoperatively under the care and decision making of a neurosurgeon (Fig. 209-1).
Management of Traumatic Brain Injury
Prehospital Management
Trauma Systems
Prehospital identification as well as assessment of TBI appears to be an important factor for patient outcomes. There are no definitive outcome data on the effect of time from the injury to arrival at the trauma center, although good data do indicate that patients fare better when treated within a trauma system. Several studies have shown a significant decrease in mortality in adult patients with acute SDH who were operated on within 2 to 4 hours after injury.13,14 Two studies, from Washington, DC, and Pennsylvania, have looked specifically at pediatric TBI patients and found increased survival in those who were transferred directly to a trauma facility with special qualifications to treat children.15,16
Improved survival in a region is a function of not just meticulous postinjury care but also an overall plan that focuses on all aspects of TBI from prevention through community reintegration. A recent study reviewed pediatric deaths as a result of trauma between 2001 and 2003 versus deaths between 1985 and 1987, before the implementation of a trauma system. The system included injury prevention programs, field triage, and designated trauma centers. In that period, the incidence of identified preventable deaths declined from 21% to 7%, a 68% reduction in relative risk, thus showing the importance of not only a coordinated trauma system but also a concomitant focus on prevention programs.17
Based on the 2007 prehospital guidelines of the Brain Trauma Foundation, it is recommended that pediatric patients with suspected severe TBI be transported directly to a facility with specific qualifications to treat children.18
Airway
Hypoxemia has been shown to have a significant impact on the survival and outcome of patients with TBI in studies of both pediatric and adult populations.19,20 Accordingly, the first concern for emergency medical service personnel should be securing an airway. Prospective studies have compared bag-valve mask ventilation and endotracheal intubation and found no difference in outcome.21,22 One such study showed that either intubation or bag-valve mask ventilation provided effective ventilation in patients with head injury, and additional studies have supported these data.23,24
Whether the airway is secured through bag-valve mask ventilation or endotracheal intubation, it is essential to prevent hypoxemia in the prehospital setting. Many studies have shown the negative impact of hypoxemia on outcome in TBI patients, with significantly worsening outcomes and mortality being associated with worsening hypoxemia at an arterial oxygen saturation (SaO2) of greater than 90% (mortality, 14.3%), 60% to 90% (mortality, 27.3%), and less than 60% (mortality, 50%).19
Another consideration in prehospital management of the airway is prevention of significant hypocapnia or hypercapnia. Physiologically, there are clear links between PCO2 and cerebral blood flow (CBF), and currently, it is thought best to maintain normocapnia. Two studies have shown that capnography with ventilator adjustments en route can significantly reduce hypocapnia on arrival at the trauma center in comparison to standard settings.25,26 Because maintenance of normocapnia in transport appears to be important, it is generally recommended that emergency medical teams have the ability to monitor PCO2, especially if they have intubated the patient.27
Resuscitation
Once the airway has been secured, the next step in prehospital evaluation is to address resuscitation. Prehospital recommendations for fluid resuscitation have been evaluated in several studies. The Saline versus Albumin Fluid Evaluation (SAFE) study compared normal saline and albumin for resuscitation and found significantly worse outcomes in patients who received albumin.28 Two studies evaluated hypertonic saline; one compared hypertonic saline with normal saline for the prehospital treatment of hypotension and found an initial survival advantage with hypertonic saline but no significant difference in long-term survival, whereas the second compared treatment with hypertonic saline versus lactated Ringer’s solution and found no difference in survival or outcome at 6 months despite early promising effects on ICP with hypertonic saline.29,30
To summarize, the primary goals of prehospital treatment are to prevent hypoxia and hypotension en route to an appropriate trauma facility. A mortality rate of 55% can occur if hypoxia, hypotension, or hypercapnia is present in the setting of severe TBI; the rate is reduced to just 7.7% when none of these risk factors are present.31 In a prospective study of almost 7000 adult and 2000 pediatric patients with TBI, Luerssen and colleagues found that hypotension had a significantly greater negative impact on the outcomes of pediatric patients.1 The 2003 guidelines recommend that hypotension, defined as systolic blood pressure below the 5th percentile for age, or clinical signs of shock should be corrected as quickly as possible with fluid resuscitation and that the airway should be controlled to avoid hypoxia.32
Clinical and Radiographic Examination
Clinical examination can be unreliable in patients with TBI. Two prospective studies of pediatric trauma patients found that 33% of the patients with abnormal head CT findings had normal results on neurological examination.33,34 Therefore, almost all children who have sustained a significant injury or are suspected of having TBI should undergo imaging. CT remains the test of choice in the acute trauma setting, and MRI and adjuncts such as angiography should also be considered. On the negative side in children with severe TBI, the initial GCS score and pupil response have been significantly correlated with long-term outcomes. If a child is initially seen with bilateral fixed and dilated pupils, multiple studies have shown 100% mortality.35,36
Intensive Care Unit Management
Guidelines for Management of Intracranial Pressure and Cerebral Perfusion Pressure
As with adults, many pediatric studies have now demonstrated improved outcomes in patients who receive aggressive management of ICP. The 2003 guidelines reviewed nine studies that included 518 pediatric patients, all of which showed an association of persistently elevated ICP (usually ICP > 20 mm Hg) with poor outcome or increased mortality (or both) in comparison to patients with well-controlled ICP.37 Several studies using different modalities to control ICP, including early decompressive craniectomy, hypertonic saline, barbiturates, and hyperventilation, have revealed improved outcomes and decreased mortality with aggressive treatment of ICP.38–41
Although there are no specific guidelines in pediatrics on when to insert an ICP monitor, several studies have provided useful information. The presence of an open fontanelle or sutures does not preclude the development of intracranial hypertension, and the fontanelle should not be used as a guideline by which to judge ICP.40 In one study consisting of 22 pediatric patients with severe TBI and an initial GCS score of 8 or less, 86% were found to have ICP higher than 20 mm Hg during the monitoring period.42 In general, a threshold for placing a monitor at a GCS score of 8 or less is what is generally accepted in the pediatric population and supported by the pediatric guidelines.37 Although infant modifiers to the GCS score exist for pediatric patients, the neurological examination can be an unreliable predictor of outcome in infants and toddlers. There have been two studies reviewing pediatric patients who initially appeared well but suffered neurological deterioration, death, or both.
Ultimately, the goal of head injury management is to provide adequate CBF to allow delivery of oxygen and nutrients to the brain. After injury, there is both increased demand for these substrates and an impaired delivery system, thereby subjecting the brain to increased risk for an energy crisis. Consequently, many authors now think that CPP is a parameter as or more important than ICP. CPP is physiologically defined as the difference between mean arterial pressure and ICP. Early work showed significant improvement in the outcomes of adult patients with severe TBI when treatment was directed toward maintaining CPP at a level higher than 70 mm Hg.43–45 One study reviewed CPP and outcomes in pediatric TBI patients and stratified patients by those with CPP of less than 40 mm Hg and then in deciles from 40 to 49 mm Hg, 50 to 59 mm Hg, 60 to 69 mm Hg, and finally, higher than 70 mm Hg and found no significant difference in mortality or Glasgow outcome score (GOS) distribution in all patients with CPP higher than 40. However, no patient with a CPP lower than 40 mm Hg survived.46 This has helped support the need to maintain CPP at a level greater than 40 mm Hg in all pediatric patients.47
The 2003 guidelines state as a treatment option that ICP above 20 mm Hg is considered a pathologic elevation and treatment should be corroborated with the findings on clinical examination, physiologic monitoring, and cranial imaging.37,48 Although specific thresholds of ICP at which to initiate treatment have not been established, data support treating ICP elevated above 20 to 25 mm Hg for a prolonged period.42,49–51 Further investigation is needed to define age-specific ranges for both ICP and CPP thresholds to guide treatment, but persistent elevations in ICP above 20 mm Hg should be considered pathologic.
Intracranial Pressure Monitoring Technology
The accuracy of fiberoptic monitors in comparison to ventricular catheters has been evaluated in both children and adults and was reviewed in the 2003 guidelines.52 The Camino fiberoptic, in general, ranged 1 to 4 mm Hg higher than the ICP recorded in comparable patients measured with a ventricular catheter, which was corroborated by a study in adult patients that also showed slightly higher readings with the fiberoptic monitor.53,54
Typically, most monitors and drains are placed in the ED or ICU and tend to be used for relatively short durations of 7 days or less. One study reviewed complications associated with ICP monitors and found no difference in the incidence of colonization of ventricular catheters with hospital location of insertion or duration of monitoring, with a Staphylococcus epidermis colonization rate of 7% regardless of the location placed. No patients had clinical features of central nervous system infection.55
Because of the relatively low complication rate and high potential survival and outcome benefit in patients with severe TBI, the 2003 guidelines support the use of ICP monitoring as a treatment option in infants and children with severe TBI.52 As mentioned earlier, an open fontanelle or open sutures (or both) do not preclude the development of intracranial hypertension and should not be considered a contraindication to placement of a monitor.
Diversion of Cerebrospinal Fluid
Cerebrospinal fluid (CSF) diversion is an excellent treatment option to lower ICP by decreasing CSF fluid volume. This can be accomplished by external ventricular drainage alone or with the addition of a lumbar drain. Several studies in pediatric TBI patients evaluated the effectiveness of CSF diversion in lowering ICP.42 Other studies reported on lumbar drainage, in addition to ventricular drainage, for control of ICP with the theoretical benefit that it can reach subarachnoid fluid spaces not affected by the ventricular drain and therefore further lower ICP.56,57
The 2003 guidelines recommend ventriculostomy and CSF drainage as a treatment option for refractory intracranial hypertension. Lumbar drainage may be added if there are open cisterns and no mass lesions on imaging.58
Hyperosmolar Therapy
Hyperosmolar therapy has a long tradition in modern medicine. These agents were first shown to reduce ICP at the turn of the 20th century, and mannitol was introduced into clinical practice in 1961. Over the next 20 years, a variety of hyperosmolar agents, including mannitol, glycerol, and urea, were used clinically, with mannitol gradually replacing most other agents for the management of intracranial hypertension by the late 1970s.59
Several studies have investigated the use of mannitol versus other agents and found mixed success, with a 1.75 relative risk for death with mannitol versus saline placebo or hypertonic saline.60–62 A final study compared the use of mannitol as treatment based on ICP monitoring (with goals of ICP < 25 mm Hg) versus the use of neurological or physiologic indications for administration of mannitol. This study found a 0.83 relative risk for death with ICP-directed mannitol administration, thus indicating a small benefit for ICP-directed administration of mannitol.63
There has been recent interest in hypertonic saline as the agent of choice in hyperosmolar therapy for head injury. Webb and McKibben first used hypertonic saline as their hyperosmolar agent in 1919 to lower ICP, but it later fell out of favor as an osmotic agent. Many studies in animals and humans have investigated the mechanism of action of hypertonic saline solutions. Hypertonic saline, unlike mannitol, expands the plasma volume and also has a higher osmotic reflection coefficient. Consequently, it may be more efficient in creating an osmotic gradient even in damaged tissue and may be less likely to induce rebound edema. Hypertonic saline could also have beneficial effects by modulating inflammation, reducing serum viscosity, restoring normal cellular membrane potential, augmenting the cardiac index, and improving gas exchange and cerebral oxygenation.64–69 Several studies have shown that fluctuations in ICP vary inversely with the serum concentrations of sodium.70–72
Outcomes in pediatric TBI patients in whom hypertonic saline has been used either as fluid resuscitation or as treatment of refractory increased ICP have been evaluated in several studies. When compared with lactated Ringer’s solution, patients receiving hypertonic saline required fewer interventions for elevated ICP, including mannitol, and also had significantly shorter ICU stays and fewer days on mechanical ventilation; however, there was no significant difference in survival.70 In another study, continuous 3% hypertonic saline solution was titrated to control ICP higher than 20 mm Hg after other treatments had failed (on average, 3 days after injury). Although two patients required short-term dialysis for renal failure, there were no long-term complications noted and the average GCS in these patients was 4.71 In another study, the authors compared 3% hypertonic saline with 0.9% saline boluses for the treatment of intracranial hypertension and found that patients receiving hypertonic saline had lower ICP and less need for interventions, which included thiopental, mannitol, dopamine, and hyperventilation.73
Several recent studies have now compared mannitol with hypertonic saline for the treatment of intracranial hypertension. Two adult studies found an improved response of ICP to hypertonic saline alone versus mannitol or in conjunction with mannitol and also found that hypertonic saline improved cerebral oxygenation, as well as CPP and cardiac output, in comparison to mannitol alone.74,75 This was supported by another study in which it was shown that hypertonic saline appears to be more effective than mannitol in controlling cerebral edema.76
With regard to the 2003 guidelines, both mannitol and hypertonic saline are considered acceptable for use as hyperosmolar therapy after brain injury. Hypertonic saline (3%) can be used to control elevated ICP by administering between 0.1 and 1.0 mL/kg and using the lowest rate needed to control ICP. Mannitol is effective for control of ICP in bolus doses ranging from 0.25 to 1 g/kg. Serum osmolarity should be maintained below 320 mOsm/L with mannitol, but levels up to 360 mOsm/L are tolerated with hypertonic saline, even when used in conjunction with mannitol.59
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree