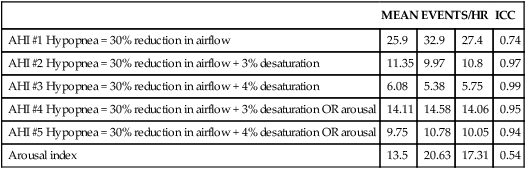
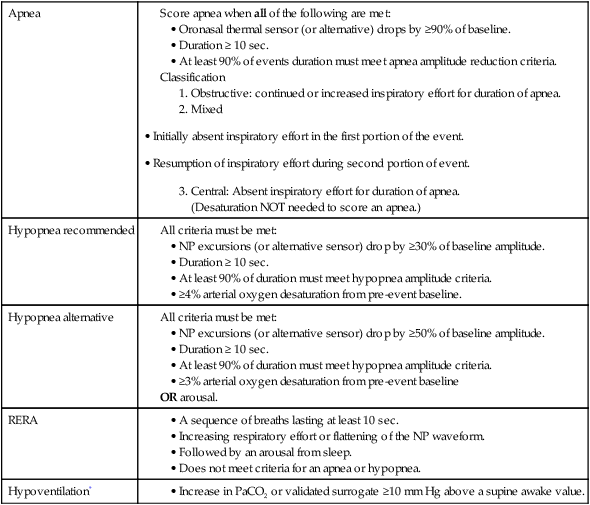
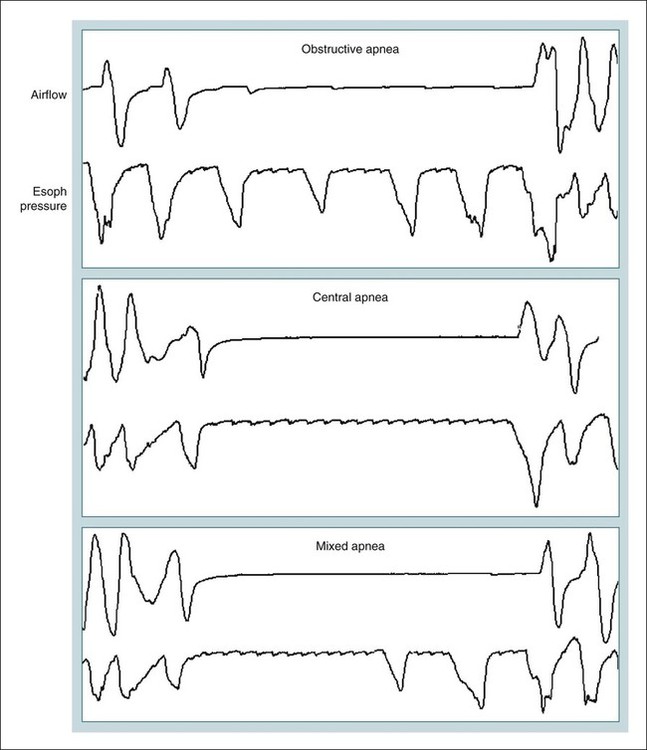
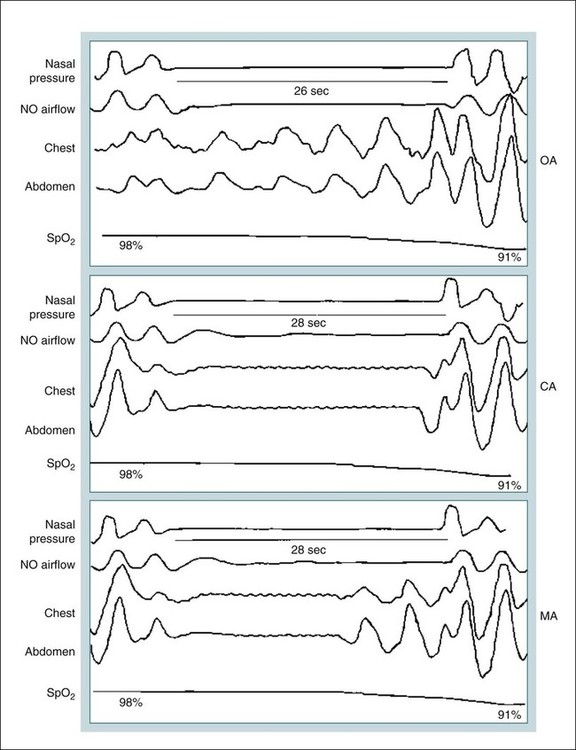
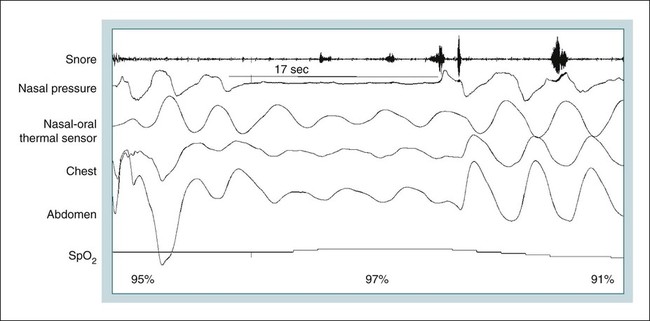
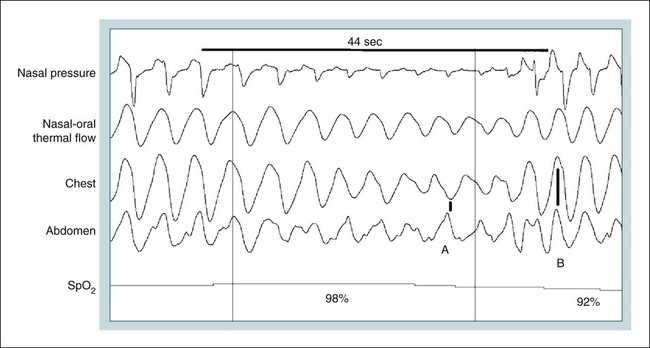
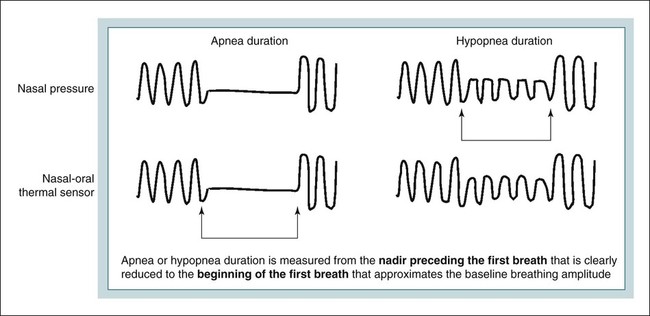
• An oronasal thermal sensor is recommended for apnea identification. The nasal pressure signal is recommended for hypopnea identification. An event with absent nasal pressure excursions but persistent oronasal sensor excursions >10% of baseline would not be scored as an apnea. • In adults, an event may be an RERA or a hypopnea based on which hypopnea definition is being used. • Hypoventilation in adults is defined as an increase in the PaCO2 of 10 mm Hg or greater from an awake supine value. • Hypoventilation in children is defined as a PCO2 greater than 50 mm Hg for 25% or more of the total sleep time by either PETCO2 monitoring or TcPCO2 monitoring. • Obstructive apneas and hypopnea in children are defined based on two missed breaths rather than an absolute time duration. • Respiratory rules for children are used for patients younger than 18 years. Adult respiratory scoring rules may be used for children aged 13 years or older. • In children, central apneas have absent inspiratory effort throughout the entire duration of the event and one of the following is met: 1. The event lasts 20 seconds or longer. 2. The event lasts 2 breaths (or the duration of 2 breaths as determined by the baseline breathing pattern) AND is associated with an arousal, an awakening, or a 3% or greater desaturation. To understand the origins of the current respiratory event definitions, a historical perspective is helpful. The apnea-hypopnea index (AHI) is the number of apneas and hypopneas per hour of sleep. This metric is often used to make the diagnosis of sleep apnea and to grade the severity. Definitions of apnea have been relatively standard (typically absent or nearly absent airflow for ≥10 sec), but varying definitions of hypopnea (reductions in airflow) have resulted in a “floating metric.”1 Early studies of patients with obstructive sleep apnea (OSA) focused on obstructive apnea,2 hence, the name of the syndrome. However, it soon became obvious that reductions in airflow (hypopnea) also had clinical significance. The importance of hypopnea, defined as a reduction in airflow associated with a 4% or greater desaturation, was emphasized by Block and coworkers.3 Gould and colleagues4 noted that some patients fit the clinical picture of OSA but the majority of their respiratory events were hypopneas rather than apneas. They defined hypopnea as a 50% reduction in respiratory inductance plethysmography (RIP) belt deflections lasting greater than 10 seconds and proposed the term the “sleep hypopnea syndrome.” Others have used the term the “obstructive sleep apnea hypopnea syndrome.” A landmark paper on the incidence of obstructive sleep apnea (Wisconsin cohort study) defined hypopnea as a discernible reduction in the amplitude of calibrated RIP plus an arterial oxygen desaturation of 4% or more.5 The Sleep Heart Health Study,6 a large multicenter population-based investigation, defined hypopneas as a decrease in airflow or thoracoabdominal excursion of at least 30% of baseline for 10 seconds or more accompanied by a 4% or more decrease in oxygen saturation.5 Airflow was monitored with an oronasal thermal sensor and respiratory effort with RIP belts. Using this definition of hypopnea, the study found associations between an increase in the AHI and cardiovascular morbidity. The widespread use of nasal pressure (NP) monitoring allowed recognition of more subtle and more frequent changes in airflow during sleep than was possible with thermal devices.7 It was also recognized that reductions in airflow from obstructive events not associated with desaturations could be associated with consequences such as arousal from sleep and sleep fragmentation (upper airway resistance syndrome).8 Therefore, definitions of hypopnea based on flow and arousal were proposed. In order to standardize definitions of respiratory events, a consensus statement was published in 1992 (“Chicago criteria”).9 Criteria for an obstructive apnea/hypopnea event (OAHE) was presented with no differentiation between obstructive apnea and hypopnea because “both events have similar pathophysiology.” An OAHE was defined as a 50% or greater reduction in airflow from baseline lasting 10 seconds or longer using a valid measure of breathing OR any discernible reduction in airflow using a valid measure of breathing during sleep when associated with either an arousal or a 3% or greater arterial oxygen desaturation. Valid measures of breathing included a pneumotachograph, NP, RIPsum (or simultaneous reduction in both chest and abdominal RIP band signals). A 3% rather than a 4% desaturation was recommended based on reanalysis of Wisconsin cohort data showing similar associations with important outcomes using either 3% or 4% desaturations. A respiratory effort–related arousal (RERA) was defined as an event lasting 10 seconds or longer with a pattern of progressively more negative esophageal pressure terminated by a sudden change in pressure to a less negative pressure and arousal. The choice of the definition of apnea and hypopnea can make a significant difference in the AHI and, therefore, a significant difference in the incidence of OSA.10–12 Ideal definitions of AHI would identify a population with symptoms and with an increased risk of adverse outcomes (if untreated). As previously noted, AHI values based on hypopnea definitions requiring an associated desaturation in large population studies have shown that increases in AHI are associated with cardiovascular morbidity. Another consideration in choosing a definition of hypopnea is the desire to have a high interscorer reliability. Whitney and associates10 reviewed the results when three experienced scorers analyzed the sleep studies of 20 randomly selected patients using different definitions of hypopnea. The sleep studies had been performed using a thermal sensor for airflow. Hypopnea was defined as a reduction in the nasal-oral thermal flow signal or the chest and abdominal RIP excursions to 70% of baseline or lower for a duration of 10 seconds or longer. There was a very large range of resulting AHIs (Table 9–1). Using a definition of hypopnea based entirely on a reduction in flow magnitude, there was a reasonably high interscorer reliability (see Table 9–1). However, inclusion of a desaturation criteria in the hypopnea definition did significantly improve the interscorer reliability for identifying these events. One rationale for not including arousal in hypopnea definitions is that scoring of arousals has relatively low interscorer reliability (see Table 9–1). However, the reliability of scoring hypopneas with a definition using a combination of flow and either arousal or desaturation resulted in only slightly lower interscorer reliability than flow plus desaturation alone. Of note, the method used to define a reduction in flow (nasal-oral thermal sensor versus RIP or NP) and the patient population studied may affect the changes in the AHI produced by varying definitions of hypopnea. Tsai and coworkers12 defined AHI-A as a discernible reduction in thoracoabdominal deflection (RIP) of 10 seconds or longer associated with a 4% or greater arterial oxygen desaturation and AHI-B as a discernible reduction in thoracoabdominal deflection longer than 10 seconds plus either a 4% or greater desaturation OR an arousal. They found AHI-B was, on average, only about 2 events/hr greater than AHI-A. However, depending on the AHI cutoff criteria, AHI-B did diagnose more patients as having OSA. TABLE 9–1 Effects of Varying Hypopnea Definitions on Interscorer Reliability and Apnea-Hypopnea Index (Events by Three Scorers)* *Hypopnea is defined as a reduction in nasal-oral thermal flow or chest and abdominal RIP excursions to 70% of baseline for 10 seconds or longer. Adapted from Whitney CW. Gottleib DJ, Redline S, et al: Reliability of scoring respiratory disturbance indices and sleep staging. Sleep 1998;21:749–757. A clinical practice parameter published by the American Academy of Sleep Medicine (AASM) recommended a definition of hypopnea similar to the one used in the population-based studies (30% reduction in flow + ≥4% desaturation).13 The rationale for the choice was that large population-based studies had shown an increased risk of cardiovascular consequences associated with an increased AHI based on this hypopnea definition. The Centers for Medicaid and Medicare Services (CMS) subsequently adopted this practice parameter definition of hypopnea for establishing criteria for continuous positive airway pressure (CPAP) reimbursement (http://www.cmshhs.gov/mcd/viewdecisionmemoasp?id=204 2008). The recently published AASM scoring manual14 provides definitions of apnea, hypopnea, and RERAs. There are different respiratory scoring rules for adults and children. An accompanying review15 discussed the evidence for the new respiratory rules. In the following sections, the AASM scoring manual definitions for apnea, hypopnea, and RERA events are presented (Table 9–2). Although the new criteria are expected to standardize terminology, the hypopnea controversy will likely continue. A recent study by Ruehland and colleagues16 found that compared with a diagnosis of OSA based on Chicago criteria, using the AASM recommended definition of hypopnea would result in 40% of patients being classified as not having OSA. If the AASM alternative hypopnea definition was used, 25% of the patients diagnosed with OSA by the Chicago criteria would be classified as negative for OSA. TABLE 9–2 Score apnea when all of the following are met: • Oronasal thermal sensor (or alternative) drops by ≥90% of baseline. • At least 90% of events duration must meet apnea amplitude reduction criteria. *For adults, hypoventilation is based on the PaCO2. No other sensor was recommended for documentation of hypoventilation. It was stated that PETCO2 or TcPCO2 may be used as surrogate measures of PaCO2 if there is demonstration of reliability and validity. From Iber C, Ancoli-Israel S, Chesson A, Quan SF for the American Academy of Sleep Medicine: The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, 1st ed. Westchester, IL: American Academy of Sleep Medicine, 2007. The term respiratory disturbance index17 (RDI) is used by some sleep centers and publications. In many sleep centers, the terms RDI and AHI mean the same thing. However, the 2005 AASM practice parameters for indications for polysomnography (PSG) defined the RDI as equal to the AHI + RERA index. Here, the RERA index is the number of RERAs/hr of sleep. The 1992 Consensus statement of the AASM recommended making a diagnosis of OSA based on the number of apneas/hypopneas obstructive events + RERAs/hr of sleep and also presented severity criteria based on this metric.9 However, the term RDI was not specifically used. Of note, the term RDI was not defined in the AASM scoring manual. It is important to note the definition of RDI when reading sleep study reports or publications concerning sleep apnea. The sensors and methods for respiratory monitoring are discussed in detail in Chapter 8. The recommended sensor for apnea detection is a thermal flow sensor at the nose and mouth (oronasal thermal sensor). If the thermal signal is inadequate, the NP signal may be used. The recommended sensor for hypopnea detection is NP with or without a square root transformation. If the NP signal is inadequate, either the oronasal thermal signal or the RIP signal (calibrated or uncalibrated) may be used. Whether the RIP sum signal or both chest and abdomen RIP signals are to be used was not specified. The sensors recommended for detecting respiratory effort include esophageal manometry or RIP (calibrated or uncalibrated). An alternative sensor for detection of respiratory effort is diaphragmatic/intercostals EMG. The sensor for detection of arterial oxygen desaturation is pulse oximetry. It is recommended that oximeters use a maximal averaging time of 3 seconds at a heart rate of 80 bpm or greater. At lower heart rates, most oximeters choose the averaging time based on heart rate and average at least 3 pulses. The recommended sensor for detection of an RERA (see later) is esophageal manometry. Flattening in the NP signal or RIP are alternative sensors that may be used. Apnea Rule: Score an apnea when all of the following criteria are met: 1. There is a drop in the peak thermal sensor excursion by ≥90% of baseline. 2. The duration of the event lasts at least 10 seconds. 3. At least 90% of the event’s duration meets the amplitude reduction criteria for apnea. 1. Score a respiratory event as an OBSTRUCTIVE apnea if it meets apnea criteria and is associated with continued or increased inspiratory effort throughout the entire period of absent airflow. 2. Score a respiratory event as a CENTRAL apnea if it meets apnea criteria and is associated with absent inspiratory effort throughout the entire period of absent airflow. 3. Score a respiratory event as a MIXED apnea if it meets apnea criteria and is associated with absent inspiratory effort in the initial part of the event, followed by resumption of inspiratory effort in the second part of the event. Figure 9–1 presents examples of obstructive, central, and mixed apneas using esophageal pressure to detect respiratory effort. Figure 9–2 presents examples of the corresponding events using chest and abdominal RIP belts. The nasal-oral thermal sensor and not the NP signal is used to score apnea. Absent NP signal excursions do not meet criteria for scoring apnea if nasal-oral thermal sensor excursions are still present and do not meet criteria for scoring an apnea. In the event shown in Figure 9–3, NP excursions are absent for greater than 10 seconds. However, the event is not scored as an apnea because the thermal signal is not decreased by 90% of baseline. The combination of absent NP excursions and persistent nasal-oral thermal sensor excursion is likely due to oral breathing. Also note that the apnea criteria do NOT depend on the presence of either arterial oxygen saturation (SaO2) or arousal. The AASM scoring manual states that if the oronasal thermal signal is not functioning, one then uses the NP signal to score apnea. Although not specifically recommended by the AASM scoring manual, one could also use the RIPsum signal. Score a hypopnea if all of the following criteria are met: 1. The NP signal excursions (or those of the alternative hypopnea sensor) drop by ≥30% of baseline. 2. The duration of this drop occurs for a period of at least 10 seconds. 3. There is a 4% or greater desaturation from the pre-event baseline. 4. At least 90% of the event’s duration must meet the amplitude reduction of criteria. This recommended hypopnea definition is essentially the definition recommended by the 2001 AASM Clinical Practice Parameter13 and later accepted by CMS. As discussed previously, evidence for the use of this definition includes the fact that a similar definition was used in the Wisconsin Cohort Study and the Sleep Heart Health Study and that an increased AHI based on this hypopnea definition was associated with an increased risk of cardiovascular morbidity in those studies. In addition, as previously mentioned, definitions of hypopnea using changes in SaO2 tend to have high interscorer reliability. The respiratory event illustrated in Figure 9–4 meets the recommended criteria for a hypopnea because the NP signal excursions are essentially zero for over 10 seconds and the event is associated with an SaO2 of 4% or greater. Score a hypopnea if all of the following criteria are met: 1. The NP signal excursions (or those of the alternative hypopnea sensor) drop by ≥50% of baseline. 2. The duration of this drop occurs for a period of at least 10 seconds. 3. There is a ≥3% desaturation from the pre-event baseline or the event is associated with an arousal. 4. At least 90% of the event’s duration must meet the amplitude reduction of criteria for hypopnea. The alternative definition of hypopnea is similar to the 1999 AASM Task Force Consensus definition of an obstructive apnea/hypopnea event. The use of 3% rather than 4% is based on the fact that reanalysis of some of the large studies using a 3% desaturation–based instead of a 4% desaturation–based hypopnea definition found similar results.9 The definition recognizes that some reduction in airflow events are not associated with a drop in the SaO2 of 4% or greater but are associated with arousal. Frequent respiratory arousals in the absence of significant desaturation can result in fragmented sleep and daytime sleepiness. However, interscorer reliability of scoring hypopneas with a definition based on either desaturation or arousals is slightly lower than with the scoring of events associated only with desaturations (see Table 9–1). A Event duration (apnea or hypopnea) is measured from the nadir preceding the first breath that is clearly reduced to the beginning of the first breath that approximates the baseline breathing amplitude (Fig. 9–5). B When the baseline amplitude cannot be easily determined (underlying breathing variability is large), events can also be terminated when either there is a sustained increase in breathing amplitude or, in the case in which a desaturation has occurred, there is event-associated resaturation of at least 2%.
Monitoring Respiration—Event Definitions and Examples
Respiratory Events in Adults
History of Respiratory Event Definitions
MEAN EVENTS/HR
ICC
AHI #1 Hypopnea = 30% reduction in airflow
25.9
32.9
27.4
0.74
AHI #2 Hypopnea = 30% reduction in airflow + 3% desaturation
11.35
9.97
10.8
0.97
AHI #3 Hypopnea = 30% reduction in airflow + 4% desaturation
6.08
5.38
5.75
0.99
AHI #4 Hypopnea = 30% reduction in airflow + 3% desaturation OR arousal
14.11
14.58
14.06
0.95
AHI #5 Hypopnea = 30% reduction in airflow + 4% desaturation OR arousal
9.75
10.78
10.05
0.94
Arousal index
13.5
20.63
17.31
0.54
Apnea
Hypopnea recommended
Hypopnea alternative
RERA
Hypoventilation*
Recommended Respiratory Sensors in Adults14
Apnea Scoring Rules in Adults (AASM Scoring Manual)14
Apnea Types
Hypopnea Scoring Rules in Adults14
Hypopnea (Recommended)
Hypopnea (Alternative)
Event Duration Rules14
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Monitoring Respiration—Event Definitions and Examples






