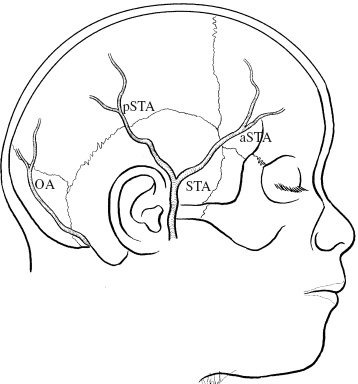
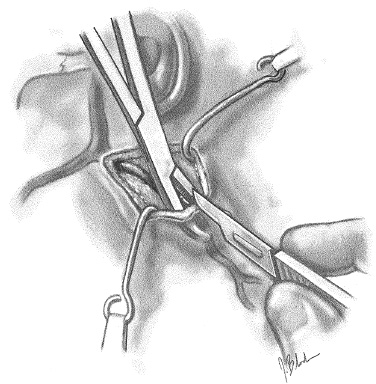
In 1979, we developed an operation called encephaloduro-arterio-synangiosis (EDAS) for the treatment of moyamoya disease in childhood. In moyamoya disease, intracranial and extracranial arteries easily form anastomoses spontaneously, and this tendency is increased by adding surgical interventions. EDAS is an operation that uses and favors these characteristics of the disease. By performing this operation, we could eliminate all the disadvantageous factors associated with surgical methods introduced before EDAS. The following are the characteristics of EDAS: FIGURE 21–1. Arteries available as donor arteries. STA, superficial temporal artery; aSTA, anterior (frontal) branch of the STA; pSTA, posterior (parietal) branch of the STA; OA, occipital artery. The goal of the treatment of moyamoya disease is to reach “a condition under which sufficient blood is supplied to the brain through the external carotid arterial system” before an oligemic state—unfavorable to the developing brain and manifested by repeated ischemic attacks—causes irreversible damage to the young brain. We believe this operation can be performed at any stage of the disease in patients who have had repeated ischemic attacks, except for those in which the brain has not yet stabilized after recent occurrence of transient ischemic attack (TIA), reversible ischemic neurologic deficit (RIND), or infarction. We recommend using the anterior and the posterior branch of the STA as the donor arteries on the dominant hemisphere in patients who have onset of the disease who are younger than 5 years of age or whose cerebral function deteriorates rapidly. Otherwise, what we consider to be the standard operation, using the bilateral posterior branches of the STA as donors, should be sufficient. The course of the donor artery is determined through palpation or with the help of a Doppler device (making reference to the course of the donor scalp artery as shown by the cerebral angiograms) and is marked on the scalp with marking ink. A shallow skin incision about 1 cm long is placed at the site immediately above and at the proximal side of the scalp artery, where the pulse can be palpated most strongly (Fig. 21–2). It is advisable to use a Feather no. 15 disposable operating knife here. Then the assistant inserts a curved hemostat into the layer between the skin and the artery (between the adipose tissue and the aponeurosis) and spreads this layer over the artery, taking care not to injure the artery, and elevates the skin upward. The operator then incises the elevated skin between the blades of the hemostat. The edges of the incised skin are separated by placing hooks applied with tension by using rubber bands. We use an EDAS frame (see Fig. 21–5.) Hemostasis for dermal bleeding can be obtained by only the tension of these hooks. FIGURE 21–2. Skin incision. The donor artery is exposed together with its attached galea for as far as possible (9 cm on average in our experience) within the range for which it can be traced safely. Two parallel incisions are placed in the galea 5 to 7 mm apart from and parallel to the scalp artery (Fig. 21–3) using a needle-shaped electric cautery. For these incisions we use a hard, nonconductive spatula with grooves, as shown in the figure. This spatula is inserted beneath the galea (above the fascia or periosteum), parallel to the donor artery, and incisions are made using a needle-tip electric cautery along the grooves of the spatula. With this method, the incision can be made quickly, producing no injuries to the adjoining tissue.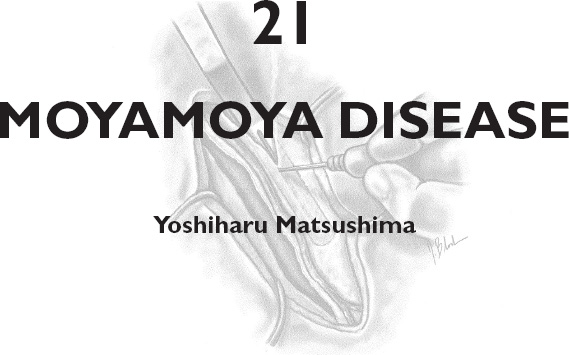
INDICATIONS AND TIMING OF OPERATION
INTRAOPERATIVE TECHNIQUES
Skin Incision
Dissection of the Galea and Preparation of the Pedicle with the Donor Artery
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


