Chapter 198 Nerve Transfers: Indications and Techniques
Traumatic brachial plexus injuries (BPIs) produce psychologically and functionally devastating handicaps afflicting, generally, a subset of young, healthy males in the prime of life. Seventy percent are caused by motor vehicle accidents, of which 70% are due to the use of two-wheelers.1 The disease burden is estimated to be about 2162 cases per annum in the United States; costs of treatment amount to about $34,733 per capita.2 It is prudent to mention at the outset that the management of traumatic BPI requires a complex multidisciplinary approach involving neurosurgeons, orthopedists, plastic/hand surgeons, neurologists, neuroradiologists, neurophysiologists, physiotherapists, and pain specialists.
Nerve Transfers (Neurotizations)
The use of and enthusiasm for nerve transfers have increased dramatically in the past two decades largely due to the creative contributions of innovators such as Drs. Christophe Oberlin and Susan Mackinnon. The introduction of a fascicular transfer by Oberlin et al. (1994)3 for upper trunk injuries catalyzed the transformation. This procedure introduced the concept of fascicular transfer by using functioning ulnar nerve fascicles supplying the flexor carpi ulnaris to be selectively transferred onto the nerve to biceps with excellent results.3–5
The new era of nerve transfer has created a major controversy in brachial plexus surgery now—the role of nerve grafts versus nerve transfers in postganglionic injuries. This issue remains largely unresolved. The advantages and disadvantages of performing nerve transfers over nerve grafts are listed in Tables 198-1 and 198-2. As can be seen, the advantages of performing nerve transfers may outweigh those of brachial plexus nerve grafting. In fact, in the event of patients sustaining panplexal nerve injuries secondary to multiple root avulsions, nerve transfers may be the only viable form of repair.
TABLE 198-1 Advantages of Performing Nerve Transfer versus Nerve Graft
| Nerve Transfer | Nerve Graft |
|---|---|
| A distal procedure performed close to the motor point of muscles. This decreases the time to reinnervation. The direct repair is at a single suture line. This improves reinnervation as well. | Performed at the site of injury, typically proximally, and thus more anatomical. These are also more physiologic and make relearning when muscle power returns easier. |
| Surgical dissection occurs in uninvolved pristine tissue. | These repairs make available more donor motor axons as nerve stumps are typically largest proximally. |
| Directed (selective) neurotization makes targeting motor recipient axons easier as it is closer to the motor end plate. | As the entire cut surface is coapted with the injured stump, sensory reinnervation is also a possibility. |
| Is the only procedure possible after nerve root avulsion. | Grafts enable entire motor groups to recover as opposed to single targeted muscles. |
| Can be performed with minimal technology. |
TABLE 198-2 Disadvantages of Performing Nerve Transfer versus Nerve Graft
| Nerve Transfer | Nerve Graft |
|---|---|
| Involves some loss of existing function, by definition. | Typically requires use of nerve grafts, e.g., non-degenerated sensory nerves like the sural. The harvest has cosmetic and functional sequelae. |
| Requires muscle re-education that can hamper autonomy because of co-contractions. | Has to be performed at the site of injury. Dissection is more difficult, especially in the presence of a concomitant vascular repair. |
| Number of available donor nerves is limited especially in patients with panplexal injuries. | Cannot be performed in patients with root avulsive injuries. |
| Number of available motor axons is necessarily limited. | Directed (motor donor to motor recipient) repair is seldom possible, especially when the loss of length is high. All proximal components of the brachial plexus are mixed sensorimotor. |
| Longer grafts should be vascularized as free grafts may fibrose secondary to ischemic injury. | |
| Grafts require axonal sprouts to cross two suture lines. This further delays repair. If the distal suture line scars densely, the entire repair may fail here. | |
| Grafts ideally require the use of intraoperative sensory and motor-evoked potentials to determine the viability of the donor nerve stump (especially proximal cervical nerves) even if it appears structurally intact. These have several technical and observer-dependent confounding factors. |
Indications
1. “Irreparable” nerves that are avulsed from the spinal cord.
Preganglionic injuries are not amenable to any other form of repair as the motor axon has been physically disconnected from the neuronal cell body across the intervertebral foramen. Reconnection via axonal regeneration is not physically possible. In such patients, motor end plate degeneration starts at the time of injury and may be irreversible after 12 to 18 months.6,7 To beat the biological clock, it is imperative to operate as soon as possible and transfer viable axons to as close to the motor end point as possible. This is the procedure of choice in this form of injury.
2. More rapid or reliable recovery of motor function.
Most experts have now begun to recognize that nerve transfers allow a faster and perhaps more reliable way of regaining function even in postganglionic injuries bucking the previous trend of using proximal nerve grafts (Table 198-3).
3. To power free-functioning muscle transfers (FFMT).
Free-functioning muscle transfer is a reliable way to reconstruct the damaged upper extremity by moving a functioning muscle with its nerve and blood supply to another location where it can subserve a new function. This can occur after a successful nerve repair and anastomosis of the artery and vein have been accomplished. This microsurgical technique therefore does not have a time window like typical nerve reconstruction. Most commonly, FFMTs have thereby been performed for delayed cases to provide elbow flexion (such as in neglected injuries or those with poor or incomplete recovery). FFMTs in this setting can augment motor function. The native anatomy of the transferred muscle/tendon unit (gracilis, for example) has important features which allow FFMTs to achieve more distal function, ordinarily unachievable with standard techniques of nerve reconstruction (e.g., recovery of prehension of the hand in patients with flail limbs). The nerve supply is relatively close to the muscle and the tendon is long (and can be prolonged). This technique then can also be incorporated into an armamentarium in combination with other nerve techniques in the early setting.
TABLE 198-3 Commonly and Uncommonly Performed Nerve Donors/Transfers
| Recipient Nerve | Common Donor Nerves | Uncommon Donor Nerves |
|---|---|---|
| Suprascapular | Spinal accessory C5 nerve C6 nerve | C4 nerve C7 nerve/middle trunk Phrenic nerve Contralateral C7 Dorsal scapular |
| Axillary | Triceps branch of radial Medial pectoral Motor intercostals | Thoracodorsal Contralateral C7 |
| MCN, biceps, or brachialis branch | Ulnar nerve fascicle Median nerve fascicle Motor intercostal Medial pectoral | Thoracodorsal Spinal accessory Phrenic Contralateral C7 Hemi-hypoglossal |
| Median | Sensory intercostals Contralateral C7 Ulnar nerve fascicle Brachialis branch of MCN | Supinator/ECRB branch of radial |
| Radial | Motor intercostals Proximal branches of radial | Contralateral C7 Dorsal scapular nerve Median nerve branches |
| Ulnar nerve | Brachialis branch of MCN Anterior interosseous | Contralateral C7 |
ECRB, extensor carpi radialis brevis; MCN, musculocutaneous.
Contraindications
The only absolute contraindications for a nerve transfer are the absence of a donor nerve and the presence of a fibrosed atrophic recipient nerve with no viable fascicles seen under magnification on sequential cut sections at the motor point. Relative contraindications would include the availability of a poor quality donor as seen with direct electrical stimulation at surgery, the presence of a stimulatable motor nerve recipient at surgery, or a short segment rupture/neuroma that can easily be repaired end-to-end without the use of a graft.
Principles
1. Accurate documentation of pre-existing muscle power, vascular injury, and joint contractures
2. Clear, coherent, and exhaustive discussion of options and priorities with the patient
3. Fall-back planning and prior consent in case favored donors are poorly functioning
4. Elaboration of realistic goals prior to surgery, including risks related to possible donor morbidity (transient and permanent) and slow nature of recovery
5. Selection of the ideal donor nerve (Table 198-4)
6. Transection of recipient nerve as proximal as possible to determine adequacy before donor dissection
7. Donor nerve dissected distal to recipient to gain length
8. Selective neurotization based on knowledge of fascicular anatomy (Table 198-5)
9. Awareness of proximal and distal orientation of transected nerve segments
TABLE 198-4 Characteristics of Ideal Donor
| Pure | Motor or sensory. Example: Medial pectoral nerve (motor); sensory intercostal nerves. |
| Adjacent | Minimal donor dissection required to gain length. Example: Double fascicular transfer for elbow flexion. |
| Expendable | Unlikely to affect donor function. Example: Intercostal nerve transfer. |
| Uninjured | Donor fascicle muscle groups must have at least grade 4/5 MRC power. Example: Spinal accessory transfer is contraindicated when shoulder function is poor. |
| Remote | From zone of injury (dissection is easier). Example: Oberlin’s transfer in upper trunk injury. |
| Proximate | To motor point so reinnervation is faster and likely better. Example: Triceps to axillary nerve transfer. |
| Adequate | Diameter mismatch is prevented. Example: Three motor intercostals are used to neurotize the nerve to biceps. |
| Educatable | Same muscle compartment is ideal, as relearning and subsequent autonomy are better and faster as antagonistic co-contractions do not occur. |
MRC, Medical Research Council.
TABLE 198-5 Fascicular Anatomy of Major Nerves
| Nerve | Donor/Recipient | Fascicular Anatomy |
|---|---|---|
| CC7 | Donor | Posterior division has 2x motor axons. |
| Median (axilla) | Recipient | Lateral root is mainly sensory. |
| Median (arm) | Donor | FCR/FDS fascicle is medial. |
| Median (arm) | Recipient | Posterior fascicle (AIN). Anterior fascicle (PT, FCR). Middle fascicle (FDS, thenar, sensory). |
| Median (forearm) | Donor | Terminal AIN branch to PQ. |
| Nerve to biceps | Recipient | Lateral in musculocutaneous nerve. |
| Nerve to brachialis | Donor/recipient | Lateral to LABC. |
| Suprascapular | Recipient | Lateral within upper trunk. |
| Ulnar (arm) | Donor | FCU fascicle is posteromedial. |
AIN, anterior interosseous nerve; CC7, contralateral C7; FCR, flexor carpi radialis; FCU, flexor carpi ulnaris; FDS, flexor digitorum superficialis; LABC, lateral antebrachial cutaneous nerve; PQ, pronator quadratus; PT, pronator teres.
Common Targets
The common recipient nerves for transfers are the suprascapular, axillary, and musculocutaneous nerves. A list of donors is provided in Table 198-3.
Surgical Anatomy
The brachial plexus is formed by the ventral rami of the fifth to eighth cervical and the first thoracic nerve roots. It is essential to remember that the nerves emerge between the scalenus anterior and medius (interscalene triangle) to form trunks in the supraclavicular fossa. The divisions of the brachial plexus are retroclavicular while the cords are infraclavicular and named as such in relation to the axillary artery.
Supraclavicular Exploration
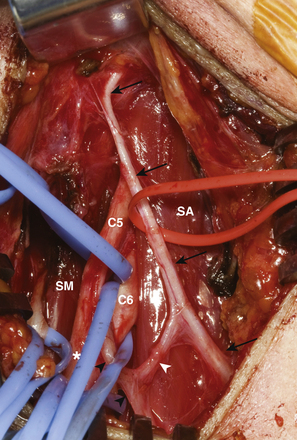
The key muscles for the supraclavicular exploration of the brachial plexus are the omohyoid (deep to which lies the fat pad covering the plexus) and the scalenus anterior (deep to which lie the nerves). The latter is often difficult to identify especially when there is extensive scarring. They are then identified indirectly as the structures that lie beneath the phrenic nerve. The phrenic nerve may be identified visually as the only neural structure (other than the nerve to subclavius) that passes from lateral to medial in the root of the neck (Fig. 198-1). If scarring is extensive, blind neural stimulation using 0.1–2 mA of current may provoke capnographic changes if not frank diaphragmatic contraction that may guide the surgeon to the approximate location of this key structure before sharp dissection is commenced.8 The phrenic nerve can then be traced back to the C5 nerve via its contribution to the former. From here, the C5 nerve can then be traced to the upper trunk. Proximal and distal dissection allows identification of C6 and the divisions of the upper trunk. The suprascapular nerve is the key target in this exploration and can be found superior, lateral, and posterior to the upper trunk. Its direction confirms its identity. It parallels the omohyoid and runs posteriorly obliquely to the scapular notch. In the event of a complete rupture of the C5 and C6 nerves, the distal components of the plexus can be found near, behind, or even below the clavicle.
Care has to be taken, during dissection, not to injure the lymphatic duct on the right and the chyle carrying thoracic duct on the left side. These elements are at risk during medial dissection such as with exposure of the lower trunk elements.
Infraclavicular Exploration
It is important to realize that the musculocutaneous nerve provides its first branch to the coracobrachialis muscle and then penetrates this muscle. This must not be mistaken for the nerve to the biceps which is given off its lateral aspect in the mid-arm (typically 12 cm distal to the acromion). The nerve to the brachialis is given off further distally (approximately 17 cm distal to the acromion) and typically lies lateral to the terminal branch, the lateral antebrachial cutaneous nerve.9 The former is a pure motor branch, while the latter is a sensory nerve. The authors verify the nature of both these terminal divisions by tracing the brachialis branch until it arborizes on the muscle surface. A variation that has to be considered is the low take-off of the musculocutaneous nerve from the median nerve. This is important to consider especially when the median nerve is being considered as a donor for a simultaneous nerve transfer.
General Principles: Surgical Technique
Positioning and Anesthesia
Patients are operated on under general anesthesia. Strict instructions are issued to ensure that no neuromuscular blocking agents are used. The patient is typically placed in the supine position with the head slightly extended and turned to the opposite side. An interscapular towel roll can also be used to make the supraclavicular fossa more prominent. Occasionally, the patient is bumped up to provide access if a posterior approach is anticipated. The arm is placed, initially, in an adducted and depressed position to enhance the exposure. However, it should be draped in such a manner as to ensure that it can be freely abducted or crossed over the chest, so as to facilitate further surgery. The hands and fingers should be kept exposed for visual inspection of evoked movements. As a substantial part of the total body surface area has to be kept exposed, it is vital to ensure that patients do not slip into hypothermia. The appropriate use of blankets and warming units is encouraged. As nerve transfers may well be done in combination with nerve grafting, wide prepping of the neck, chest, arm, and both legs is always done for various exposures and harvest of nerve graft(s).
Technique of Nerve Coaption
First we prepare all of the donor and recipient nerves or fascicles and clip them with redundancy to green backgrounds, once transected, to ensure high visibility. Then we perform all of the microsurgery of the various nerves. We trim back on the recipient so that its length is as short as possible so as to minimize reinnervation time to the end organ. A repair with tension is avoided. The repair is tested in the maximum anticipated range of joint movements in all directions. Diameter mismatches are avoided wherever possible and selective neurotization is practiced when it is not. Donor and recipient nerve fascicles are further skeletonized and soft tissue is denuded at the coapting ends to prevent scar formation. The fascicular ends are finally sectioned using an ultrafine diamond knife. Coaption is then carried out using interrupted, nylon, monofilament 9-0 sutures passed through the epineurium of adjacent fascicles. An operating microscope with twin mobile opposable eyepieces is used so that two surgeons can operate simultaneously. Frequent heparinized saline flushes ensure adequate visibility at the time of coaption. Typically, two diametrically opposite sutures are used with three throws each. The initial knot is tensioned gradually so as to just appose the cut sections of the participating fascicles without buckling them. Knots are initially cut long so as to rotate the line of coaption to look for any unevenness. If the suture line is uneven or buckled, more sutures or else release of existing sutures and redo may be preferred as this is the most vital part of the operation. Once the suture line is observed to be satisfactory, we place a bivalved nerve tube of an appropriate diameter to protect the repair. This is then cemented in with the use of tissue adhesive.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree