Schematic drawing of the bulbus.
Papilla
The papilla (discus nervi optici) is the origin of the ON and has a diameter of 1–1.5 mm. The papilla can be slightly excavated in normal subjects. The artery and vena centralis retina pass the papilla. Elevated intracranial pressure can lead to a swelling of the papilla (papilledema) due to high liquor pressure, reduced venous flow or inflammatory processes.
Optic nerve
The length of the intraorbital part of the ON is about 2.8 cm (lamina cribrosa-canalis opticus). The “optic nerve,” an extracranial part of the brain, is sheathed by the dura, arachnoidea and pia sheath. There is a liquor communication to the subarachnoidal space of the brain. About 1.2–2 cm distal of the globe the retinal vein and artery usually penetrate the nerve sheet. The diameter of the ON sheath is about 5–7 mm and could differ between right and left eye in normal subjects.
Intraorbital vessels
The ophthalmic artery (OA; arteria [a.] ophthalmica) is the first branch of the a. carotis interna (ICA) and branches in several arteries – central retinal artery (CRA), a. lacrimalis, a. supraorbitalis, a. ethmoidalis superior, a. ethmoidalis anterior, rami musculares, aa. ciliares posteriores breves – and finishes in the a. supratrochlearis and a. dorsalis nasi (Figure 25.2). The first part of the OA is located within the inferolateral area of the ON in about 90% of people and has an external diameter of 1.7 mm; 73% of the cases cross the ON superiorly, and 27% inferiorly. The first branch of the intraorbital part of the OA is the CRA in 26–47% and medial posterior ciliary artery in 26% of eyes. The CRA enters the ON 7.5 ± 2.2 mm (min.–max. 5.3–12.5 mm) behind the ocular bulb. The posterior ciliary arteries run forward, divide into multiple branches and penetrate the sclera close to the ON medially, laterally or superiorly. The longitudinal capillaries run between the ON and the CRA anterioposteriorly, while the transverse capillaries surround the ON [8].
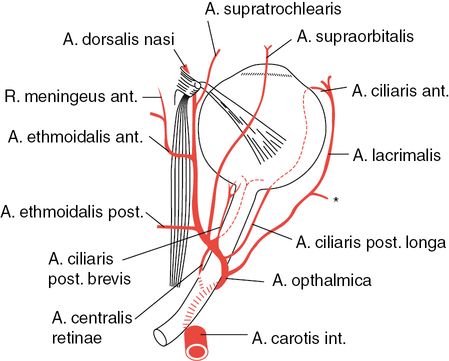
Schematic drawing of the intraorbital arteries.
Imaging tips
Probe selection
Standard neurovascular ultrasound machines equipped with linear-array transducers emitting 6–12 MHz (up to 15 MHz) are sufficient.
Safety aspects
The output of the machine needs to be adjusted to the requirements of orbital sonography according to the ALARA principle (“as low as reasonable achievable”). The main biological effects would be cavitation and temperature increase. Current guidelines released by the US Food and Drug Administration limit the acoustic output to temporal average intensities <50 mW/ cm2 and a mechanical index (MI) of <0.23 [9]. We recommend the examination time to last less than a minute for each eye. In order to prevent cavitation effects, we strongly recommend a presetting of the ultrasound machine using a button “orbital ultrasound” with a predefined limitation of the MI <0.23, TI <0.2, ISPTA-value <17 mW/cm2. In special situations (e.g., for improving the color mode intensity), one can increase the power beyond this limit for a short time. The color mode should be adapted to lower velocities.
Steps of investigation
The patient should be informed about the procedure, the risks and the goal of the examination before insonation.
Place the patient in a supine relaxed position, with both of their eyes closed during the whole examination. Ultrasound gel may irritate the eyes. There is no clear recommendation about removing contact lenses before examination (we do not).
The probe should be held in one hand and the heel of the hand should be placed on the skull of the patient to avoid high and uncontrolled pressure on the eyeball by the probe. Set the probe on the lateral upper closed eyelid in an oropharyngeal direction (Figure 25.3).
Due to Bell’s phenomenon, which is an upward and outward movement of the eye, the ON is curved. Some subjects could “look straight” even with closed eyes, which helps to better insonate the ON.
Move the probe to get a full screen of the bulbus and the proximal ON (Figure 25.4). Freeze and store the image digitally. During manual image processing, elevate the probe from the eye to reduce insonation time.

Examination of the left eye of a patient. Note, to avoid pressure on the bulb due to the transducer, the hand should be kept on the skull.
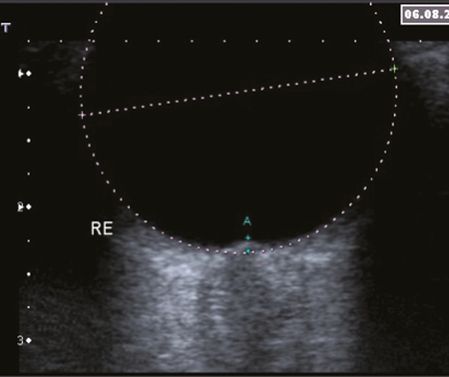
Right eye of a patient in the B-mode (6–9-MHz linear probe, MI <0.2). In the postprocessing, the bulbus (hypoechogenic) is marked by a circle which allow definition of a papilla position. The distance (A) could be used as the prominence or excavation of the papilla. Note the ON present as a hypoechogenic structure especially at the border.
Examination of the papilla
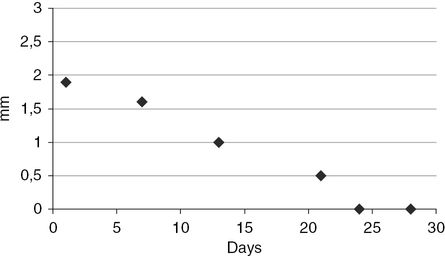
The papilla is quickly displayed (within seconds) if the bulbus is scanned in B-mode imaging. The origin of the ON could serve as a landmark. After optimizing the image, the plane with the maximum disc elevation or excavation is selected and frozen for further measurements. We recommend overlaying the bulbus with a circle (see Figure 25.4). This allows measurement of the distance from the circle to the papilla prominence. This method is suitable for intrasubject follow-up measurements. It is not easy to convert the distance given in millimeters to the optic values of dioptric units. Prominence of the papilla is easy to document in B-mode imaging (Figure 25.5). The method is optimal to control the therapeutic effects on intracranial pressure by measurement of the prominence of the papilledema (Figure 25.6).
Documentation: probe (linear MHz, MI), bulbus from both eyes, maximum raising of the papilla in mm. Description: the papilla excavation was x mm on the left eye and y mm on the right eye (normal value <0.5 mm).
Interpretation: papilla prominence is probably an indicator for ICP measurement and management. A reliable cut-off value to predict an ICP >20 cmH2O seems to be 5.7–6.0 mm with a sensitivity of 87–95% and a specificity of 79–100% [10,11]. It could also be an indicator for inflammation or ON compartment syndrome [4].
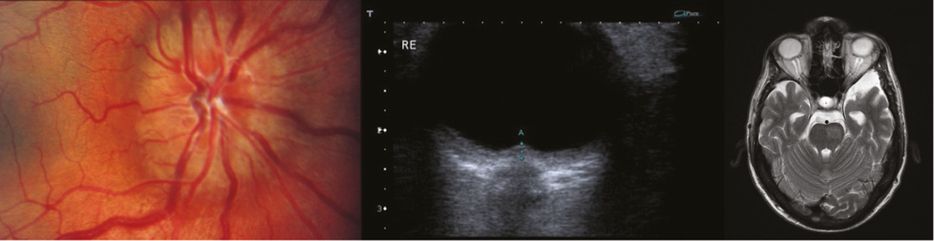
Patient with papilledema (left side: fundoscopy, kindly provided by U. Löw) and the B-mode scan (center) reveal prominence of the papilla of about 1.8 mm (A) (linear probe 6–9 MHz, MI <0.2). MRI scan (right side) of the patient revealed the swelling of the optic nerve on both sides.
Optic nerve
The ON is easily to detect as a hypoechogenic structure near the distal pole of the globe and serves as a landmark. Similar to the intima–media thickness, the ultrasound B-mode images map the ON sheet, that is, the ON and their sheets (Figure 25.7).
For standard measurements of the ON diameter, the point of length calculation is about 5 mm behind the papilla. Normal values for ON are 4–5 mm [10,11].
Documentation: probe (MHz, MI), images showing the bulbus and the ON should be documented for each eye separately and the following result should be described: ON for the right side x mm and left side y mm (normal value 4–5 mm).
Interpretation: several studies prove close association of ultrasound and MRI scanning of the ON diameter with good inter-rater and -observer reliability [12,13]. Raised intracranial pressure in patients with severe head injury, intracranial bleeding or idiopathic intracranial hypertension often display ON enlargement. Patients with demyelinating diseases are reported to have significantly smaller ONs and increased echogenicity [14].
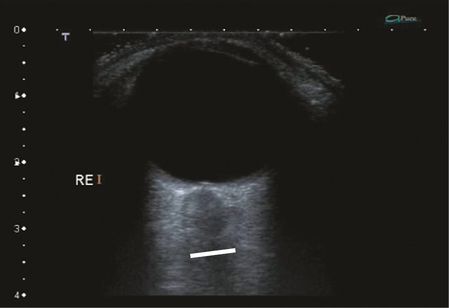
B-mode scanning of a patient with swelling of the ON but without papilla prominence. The image reveals a hypodense area behind the papilla which may be an indicator of increased liquor volume or inflammation reaction. Distance marker: 6 mm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree