Neurovascular Ultrasound
Tatjana Rundek
INTRODUCTION
Neurovascular ultrasound includes two major ultrasound imaging technologies: extracranial ultrasound (duplex ultrasound or Color Doppler) and transcranial ultrasound (transcranial Doppler). Together, these techniques provide a real-time, noninvasive, comprehensive, and affordable evaluation of the major brain-supplying arteries. Besides, these imaging technologies are repeatable and portable and therefore can be performed at bedside, emergency rooms, or at any other patient care settings. Extracranial Doppler and transcranial Doppler have become an integral part of the evaluation of patients with cerebrovascular disease or in asymptomatic individuals at an increased risk of vascular disease. These technologies are also an integral part of primary and comprehensive stroke centers. The most established clinical situations for the use of neurovascular ultrasound include the early detection and characterization of extracranial and intracranial atherosclerosis and occlusive disease; the evaluation of cerebral hemodynamic consequences of proximal arterial occlusive disease; monitoring of response to treatment of acute or chronic occlusive atherosclerotic disease; the time course and reversibility of cerebral vasospasm after subarachnoid hemorrhage; the detection of cerebral emboli in patients with cardiac, aortic, and carotid disease; and selection of sickle cell patients for blood transfusion as an effective imaging technology in primary stroke prevention. Neurovascular ultrasound is often used to complement other neuroimaging technologies such as magnetic resonance angiography (MRA) and computed tomography angiography (CTA). All of these neuroimaging techniques provide concordant results when performed in accredited laboratories. If discrepancies arise, conventional two-dimensional angiography may be indicated, mainly if an immediate interventional revascularization procedure is considered.
EXTRACRANIAL ULTRASOUND (DUPLEX ULTRASOUND OR COLOR DOPPLER)
Extracranial ultrasound is the noninvasive method of screening the extracranial carotid and vertebral arteries for an atherosclerotic disease with the lowest risk and cost. It provides real-time imaging of anatomy, physiology (hemodynamics), and pathophysiology of the extracranial circulation. Extracranial ultrasound is used in the risk stratification of patients with symptomatic or latent cerebrovascular disease as well as in asymptomatic patients to detect the presence of carotid stenosis and to evaluate other carotid artery phenotypes, including carotid plaque size, plaque echomorphology, intima-media thickness (IMT), and carotid stiffness.
Imaging modes of extracranial ultrasound include the brightness or B mode, where ultrasound echoes are displayed in various levels of gray; color or C mode, where the Doppler signal of blood flow velocities is displayed in color; Doppler or D mode, where shift in echoes is obtained from the moving blood particles and displayed as a Doppler spectrum of blood flow velocities; power mode, where the Doppler signal of blood flow is displayed independent of the angle of insonation and is therefore magnified; and motion or M mode, where motion of interfaces is recorded along the depth axis. An ultrasound system that combines the B and D modes is called duplex ultrasound, and if B, C, and D modes are combined, it is called “triplex” or Color Doppler. All modern ultrasound systems are now equipped with all of these imaging modes.
CAROTID ULTRASOUND CRITERIA FOR DETECTION OF CAROTID STENOSIS
Traditionally, carotid stenosis is usually defined as stenosis greater than 50% by carotid ultrasound criteria. The most important ultrasound measures in assessing carotid stenosis are peak systolic (PS) velocity, end-diastolic (ED) velocity, and velocity ratios. These are applied in prestenotic, stenotic, and poststenotic regions. The degree of stenosis is also assessed visually from gray-scale ultrasound images and crosschecked with Color Doppler imaging, which can guide Doppler velocity determination in order to select the most critical part of stenosis for Doppler velocity examination. The examples of carotid ultrasound criteria for the degree of carotid stenosis are widely available. The Society of Radiologists in Ultrasound has published multidisciplinary consensus on diagnostic criteria to grade the internal carotid artery (ICA) stenosis using Duplex ultrasound [Level 1]1 (Table 23.1). These criteria can be used as a template for new vascular laboratories as well as to validate individual laboratory criteria for the estimation of carotid stenosis (Fig. 23.1). Because of Doppler velocity measurement variability and specific patient populations, there are discrepant criteria for Doppler parameters of carotid stenosis. Each carotid ultrasound laboratory must, therefore, develop and validate its own criteria to grade carotid stenosis. These parameters must be validated with other imaging modalities and/or surgical findings and an ongoing quality control program must be implemented.
ASSESSMENT OF CAROTID ARTERY AFTER CAROTID ENDARTERECTOMY AND STENTING
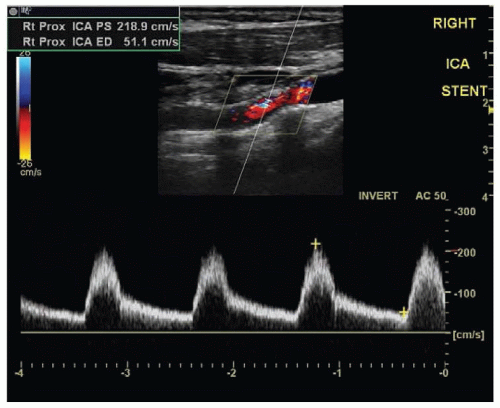
Carotid imaging shows changes in the carotid artery wall after successful carotid surgery or stenting. Special attention needs to be paid to the evaluation of the arterial wall changes at the edges of carotid reconstruction where incomplete plaque removal and residual stenosis can be detected. In addition, Doppler velocities may show values above normal through the reconstructed part of the artery likely due to flow remodeling or increased stiffness in the stented segments. If PS velocities at maximal narrowing in the reconstructed artery is greater than 150 cm/s and the PS ratio between stenotic and prestenotic (or prestented) segment is greater than 2, then significant restenosis likely occurred (Fig. 23.2).
TABLE 23.1 The Society of Radiologists in Ultrasound Multidisciplinary Consensus Criteria for Carotid Stenosis | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||
SENSITIVITY AND SPECIFICITY OF DUPLEX ULTRASOUND IN DETECTING CAROTID STENOSIS
Extracranial ultrasound is accurate and reliable in detecting carotid stenosis. The positive predictive value (PPV) of carotid ultrasound as compared to conventional angiography is 82% to 97%. In a large meta-analysis of 17 studies comparing carotid ultrasound with carotid angiography, carotid ultrasound had a pooled sensitivity of 86% (95% CI, 84% to 89%) and a pooled specificity of 87% (95% CI, 84% to 90%) for carotid stenosis [Level 1].2 For diagnosis of occlusion, carotid ultrasound had a sensitivity of 96% (95% CI, 94% to 100%). Although there can be considerable variation in the accuracy of duplex scanning among laboratories, accreditation programs such as Intersocietal Accreditation Commission (IAC) set standards for performance and accuracy of vascular testing.
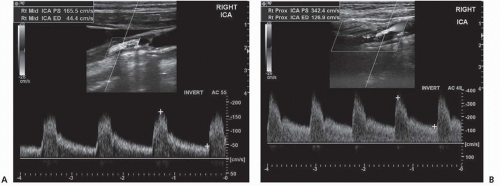 FIGURE 23.1 Two Color Doppler carotid artery studies, each showing different degree of the extracranial internal carotid stenosis. The studies show B mode (brightness mode) ultrasound image (gray scale) of the internal carotid artery (ICA) with corresponding atherosclerotic plaque, C mode (color mode) with color-coded blood flow velocity in the chosen volume sample (the selected box in the image), and D mode (Doppler mode) with the blood flow waveforms representing the velocity profile calculated from the Doppler shift (waveforms shown with velocity in cm/s in each picture from the chosen volume sample (represented by the diagonal line within the color-selected box). The peak systolic (PS) and end-diastolic (ED) velocities are marked with the yellow calipers in both pictures and used for the assessment of the degree of carotid stenosis. Two examples of varying degrees of ICA stenosis are presented: (A) ICA stenosis of 40% to 60%, with PS velocity of 165.5 cm/s and ED velocity of 44.4 cm/s (or 50% to 70% stenosis using the Society of Radiologists in Ultrasound Multidisciplinary Consensus Criteria1); and (B) with ICA stenosis of 60% to 80% (or >70% using the Society of Radiologists in Ultrasound consensus), with PS velocity of 342.4 cm/s and ED velocity of 126.9 cm/s and moderate turbulent blood flow. |
CAROTID ULTRASOUND OF CAROTID PLAQUE SIZE, MORPHOLOGY, AND CAROTID INTIMA-MEDIA THICKNESS
Carotid ultrasound provides information on plaque size (regardless of the degree of stenosis) and plaque echomorphology.
The presence of small nonstenotic carotid plaque on ultrasound is an independent predictor of future stroke and other cardiovascular disease independent of the degree of stenosis, although it is related to the degree of carotid stenosis. Detection of plaque ulceration by ultrasound imaging is limited. However, plaque surface irregularity is easy to detect on ultrasound and was shown to be associated with an increased risk of stroke. Ultrasound may help characterize plaque using a qualitative scoring system (echolucent or echodense; homogenous or heterogeneous plaque) as well as by the quantitative, computer-assisted echodensity parameters, such as the gray-scale median (GSM) index, recently shown to be clinically relevant in the prediction of stroke. Echolucent carotid plaque (soft) has been associated with an increased risk of first-ever stroke or myocardial infarction in asymptomatic individuals. Echodense carotid plaque (calcified) is in general considered to be of a good prognostic feature based on the lower rates of stroke, but recent studies have shown opposite results with an increased risk of stroke. Similar observation was reported for coronary calcium score. This presumably paradoxical effect of plaque calcification may be explained by the fact that echodense plaque is not a cause of stroke but rather a marker of presence of an “active” plaque in other vascular beds, which then can explain its association with increased vascular risk.
The presence of small nonstenotic carotid plaque on ultrasound is an independent predictor of future stroke and other cardiovascular disease independent of the degree of stenosis, although it is related to the degree of carotid stenosis. Detection of plaque ulceration by ultrasound imaging is limited. However, plaque surface irregularity is easy to detect on ultrasound and was shown to be associated with an increased risk of stroke. Ultrasound may help characterize plaque using a qualitative scoring system (echolucent or echodense; homogenous or heterogeneous plaque) as well as by the quantitative, computer-assisted echodensity parameters, such as the gray-scale median (GSM) index, recently shown to be clinically relevant in the prediction of stroke. Echolucent carotid plaque (soft) has been associated with an increased risk of first-ever stroke or myocardial infarction in asymptomatic individuals. Echodense carotid plaque (calcified) is in general considered to be of a good prognostic feature based on the lower rates of stroke, but recent studies have shown opposite results with an increased risk of stroke. Similar observation was reported for coronary calcium score. This presumably paradoxical effect of plaque calcification may be explained by the fact that echodense plaque is not a cause of stroke but rather a marker of presence of an “active” plaque in other vascular beds, which then can explain its association with increased vascular risk.
Carotid IMT is a measure of subclinical atherosclerosis shown to be associated with an increased risk of stroke and other cardiovascular disease. It has been used extensively as an outcome measure in numerous clinical trials testing the effect of lipid, blood pressure, and glucose-lowering medications. It has been associated with traditional vascular risk factors across different age groups, including in children and young adults. The American Society of Echocardiography and Society for Vascular Medicine have supported the use of carotid IMT in vascular risk stratification in moderate-risk individuals and outlined the recommendations for the IMT protocols [Level 1].3
DUPLEX ULTRASOUND OF THE VERTEBRAL ARTERIES
The ultrasound evaluation of the vertebral arteries (VAs) is similar to that of the carotid arteries. Examination of the VA is, however, limited by its anatomy because VA, unlike the carotid, cannot be traced continuously when it passes within the transverse processes of cervical vertebrae. Therefore, ultrasound examination of the extracranial VA is reliable only at the origin, intervertebral segments, and at the atlas-loop portion. Color Doppler and Power Doppler are particularly useful in assessing the caliber of VAs. Use of other diagnostic technologies (MRA, CTA, and even conventional angiography) is often recommended in symptomatic patients with suspected VA stenosis on Duplex ultrasound.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree