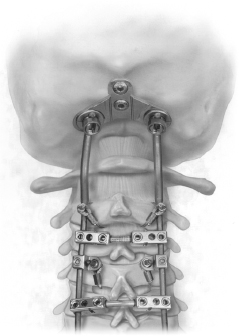
26 Occipitocervical Fusion I. Key Points – Maintaining occipitocervical (OC) alignment, decompressing neural elements, and achieving a strong arthrodesis are the main goals of this procedure. This is accomplished by judicious use of fluoroscopy/image guidance and meticulous technique in decorticating and placing the graft material. – Traction is not applied in cases of occipitocervical dislocation or significant ligamentous injury on magnetic resonance imaging (MRI). – As part of preoperative planning, make sure to review the depth of the midline suboccipital keel, thickness of the paramedian cranium, and course of the vertebral artery. – Prior to locking in the construct, verify that a neutral occipitocervical relationship has been achieved. II. Indications – Occipitocervical instability due to trauma, infections, rheumatoid arthritis, tumors, iatrogenic injury (after transoral odontoidectomy), congenital anomalies, cranial settling with brainstem or cord compression1 III. Technique – For most of these patients fiberoptic intubation is performed, and then baseline somatosensory evoked potentials (SSEPs) and motor evoked potentials (MEPs) are obtained with the patient still supine. – Maintaining cervical alignment, rotate the patient to the prone position onto chest rolls or a Jackson frame. – The head is secured with a Mayfield cranial fixation system (Schaerer Mayfield, Randolph, MA) or in modest traction with tongs when not contraindicated (OC dislocation). – Cervical alignment is maintained and checked with fluoroscopy to ensure a neutral OC relationship. – The suboccipital area is shaved and cleansed. If autograft is required, the hip harvest site is incorporated in the prepped area. – A midline incision is extended from the inion to the lowest level to be incorporated in the construct. – Subperiosteal dissection with Bovie electrocautery (Bovie Medical Corporation, Clearwater, FL) is performed to expose the suboccipital bone. Special care is taken to leave a cuff of fascia near the inion for subsequent closure. This ensures that the occipital plate will be fully covered by muscle, reducing the chances of hardware eroding through the skin. – Subperiosteal dissection is also used to expose the dorsal elements of the cervical spine. When exposing the arch of C1, blunt dissection with a Penfield 1 is recommended to avoid injury to the vertebral artery. – Any decompression required (suboccipital or cervical) is now performed, with the bone saved for autograft. – Occipital fixation can be performed using a variety of methods: occipital wiring, occipital in/out buttons, occipital screw fixation (occipital plate) (Fig. 26.1), or occipital condyle screw fixation. The current evidence supports the superiority of cranial screw fixation over wire and cable constructs with respect to both clinical outcomes and fusion rates. – First place the suboccipital plate in position and use one of the plate apertures to mark the midline keel with a marking pen. The plate is removed and a hand-held power drill is used to make a bicortical hole. To avoid injury to the suboccipital neural structures, drill in a progressive fashion—first to a depth of 8 mm, then slowly increasing the depth in 2 mm increments until bicortical penetration is felt, usually around 10 to 14 mm. The hole is tapped (this is mandatory; the occipital keel is only cortical bone) and then the plate is repositioned over this hole and secured with an appropriate-length screw with a 4.5 mm diameter. The other midline holes can now be drilled with the plate in position. – Some plates provide the option of paramedian holes for screw placement. Keep in mind that the paramedian bone in the suboccipital region is not as thick as the midline keel. – The cervical instrumentation can now be placed and incorporated to the suboccipital plate using rods bent to the appropriate shape. – The plate should be placed high in the suboccipital bone (closer to the inion than to the foramen magnum) to leave a small area of bone caudal to the plate for fusion surface. – An alternative to plate systems is the occipital condyle screw fixation.2 It is particularly useful in situations where a suboccipital decompression is required. With this technique a 3.5 mm × 20 to 22 effective length and 10 to 12 mm lag shank screw (30 to 34 mm) is placed in the center of the condyle, inferior to the hypoglossal canal. Although different techniques for its placement have been described, in general the screw has a medial trajectory (10 to 25 degrees) from an entry point about 5 mm lateral to the foramen magnum on the condyle itself. Image guidance and free-running electromyography (EMG) monitoring of the hypoglossal nerve are highly recommended with this technique. Fig. 26.1 Occipital plate and rod system. Illustration of the Summit occipital plating and rod system (DePuy Spine, Raynham, MA). Note that the occipital anchor plate is extended to the cervical spine via rods anchored by sublaminar wires that pass through custom cable connectors (reprinted with permission from DePuy Acromed; SCSCT pg. 434, Fig. 26-14). IV. Complications – In contemporary series, complication rates (minor and major) range from 12 to 30%.3,4 • Wound infection, cerebrospinal fluid (CSF) leak, intracranial injury (sub-/epidural hematoma), spinal cord injury (instrumentation into spinal canal), vascular injury (hardware into vertebral artery) • Hardware failure (loosening, pullout, breakage) • Nonunion requiring re-operation • Fixation of patient’s neck in exaggerated flexion or extension V. Postoperative Care – Upright x-rays with cervical collar – Subfascial drain – Prophylactic antibiotics for 24 hours – Prompt mobilization with collar VI. Outcomes – Fusion rates of 94 to 97% with screw-rod constructs and more than 85% neurologic improvement have been achieved in patients with myelopathy.1,4 – Screw-rod constructs have a much lower pseudarthrosis rate compared with wiring techniques (6 vs 27%) and result in a higher rate of neurologic improvement (86 vs 40%).5 – Early biomechanical studies suggest that condyle screw fixation is biomechanically equivalent to suboccipital plate systems in terms of providing craniocervical stability.2 VII. Surgical Pearls – Cervical traction is not applied in cases of occipitocervical dislocation. – As part of the preoperative planning, make sure to review the depth of the midline suboccipital keel, thickness of paramedian cranium, and course of the vertebral artery. – Prior to locking in the construct, verify that a neutral occipitocervical relationship has been achieved.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







