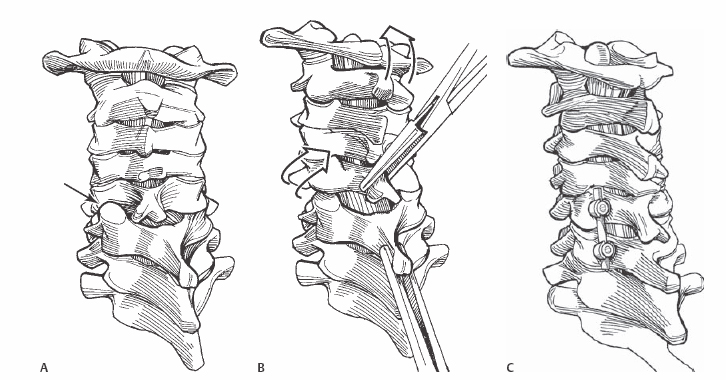
5 Moe R. Lim, Sameer Mathur, and Alexander R. Vaccaro Open posterior reduction of unilateral or bilateral facet dislocations or fracture/dislocations. The key principle for achieving reduction is the gentle re-creation of the injury mechanism followed by manipulation of the affected segments into normal alignment. Avoidance of neurologic injury with the reduction maneuver. After a failed attempt at closed reduction, a cervical spine MRI is mandatory to search for a disk herniation. A significant disk herniation may be dragged into the canal and cause spinal cord compression during open reduction under general anesthesia. In the presence of a disk herniation, an anterior diskectomy is required prior to open posterior reduction. Neurophysiologic spinal cord monitoring during the reduction maneuver is extremely helpful. If an alert is detected, the reduction maneuver can readily be reversed, potentially avoiding neurologic injury. Multimodality monitoring is preferred with motor evoked potentials, somatosensory evoked potentials, and spontaneous electromyogram (EMG) recordings. For anesthesia, awake fiberoptic intubation avoids excessive cervical extension and allows a neurologic exam after intubation. Neurophysiologic baselines are recorded after the administration of general anesthesia, prone positioning, shoulder taping, and other closed cervical manipulation. The patient is placed in traction with Gardner-Wells tongs on a Stryker frame to allow for the preservation of cervical stability while turning the patient prone. The reduction should be achievable with only gentle manipulation. Greater amounts of force may cause a spinous process fracture or neurologic injury. If difficulty in reduction is encountered, additional muscle relaxation from anesthesia may be helpful. If additional relaxation does not allow safe reduction, the superior articular facet(s) of the caudal vertebra can be trimmed with a burr. This decreases the barrier to posterior translation of the inferior facet of the cephalad level. The amount of bone resected, however, should be minimized to allow native bony stability following the reduction. A nerve hook placed along the medial edge of the inferior cephalad facet can also provide addition leverage. If significant neurophysiologic signal changes are encountered during the reduction maneuver, the procedure should be halted. Once other potential causes of the signal changes (such as hypotension) are ruled out, the patient should be carefully turned supine and a diskectomy performed. Because reduction should afford an indirect decompression of the spinal cord, neurophysiologic changes with attempted reduction likely indicate anterior cord compression by a herniated disk. Traumatic dural lacerations may also occur in facet dislocations with a concomitant lamina fracture. When encountered, a watertight repair should be performed. If repair is not possible, a lumbar drain can be used to divert cerebrospinal fluid (CSF) flow. After prone positioning and establishment of neurophysiology baseline recordings, a standard subperiosteal dissection of the posterior cervical spine is performed. Care should be taken to avoid violating the facet capsules and interspinous ligaments of levels not involved in the intended fusion. The dislocated level can often be detected by a step-off in the spinous processes or the associated soft tissue injuries. Once the dislocated levels are identified, the lateral masses are exposed completely. The dislocation can be reduced by grasping the involved cephalad and caudal spinous process with a tenaculum at the spinolaminar junction. The neurophysiologist should be warned of the possibility of an acute signal change. If any significant neurophysiologic changes are detected, the procedure should be halted. Axial caudal traction is applied to the caudal tenaculum. A gentle distraction and kyphotic moment is applied to the cephalad tenaculum to re-create the injury mechanism. A rotational force may also be additionally required for unilateral facet dislocations. The maneuver is applied until the inferior articular processes of the cephalad vertebra are freed from underneath the superior articular processes of the caudal vertebra. Once the inferior facets of the cephalad vertebra clear and become posterior to the superior facets of the caudal vertebra, the difficult portion of the reduction is complete. To achieve anatomic alignment, posterior compression is applied using spinous process wiring or lateral mass screws (Fig. 5.1, Fig. 5.2, and Fig. 5.3).
Open Reduction of Unilateral and Bilateral Facet Dislocations
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








