46 Pedicle Subtraction Osteotomy/ Smith Petersen Osteotomy
I. Key Points
– For correction of mainly symptomatic fixed sagittal imbalance (pedicle subtraction osteotomy [PSO]) and nonfixed sagittal imbalance (Smith-Petersen osteotomy [SPO])1
– An asymmetric PSO can also be used for correction of coronal imbalance.
– Can aid in the correction of coronal balance via posterior column release (SPO) or three-column release (PSO)
– Can be performed on the thoracic or lumbar spine
II. Indications
– Uncompensated spinal kyphoscoliosis (thoracic and/or lumbar) with or without progression
– Correction of fixed kyphosis requiring more than 30 degrees of correction (PSO) at one spinal segment
– Correction of nonfixed deformity requiring 5 to 10 degrees of correction (SPO) per spinal segment
III. Technique
Pedicle Subtraction Osteotomy
– 1. Position on Jackson frame with extended chest bolster.
– 2. Neurophysiologic monitoring should be used (transcranial motor evoked potentials, somatosensory evoked potentials, electromyography) to minimize neurologic injury during correction
– 3. Place two to three levels of bilateral pedicle screws cephalad and caudal to the target vertebral segment (i.e., commonly L2 or L3 in the lumbar spine).
– 4. Remove transverse process and rib head (if in thoracic spine).
– 5. For 360 degree extrapedicular vertebral body exposure, dissect soft tissues and vascular structures from vertebral body with placement of malleable retractors to maintain separation.2
– 6. Perform Gill laminectomy of the target vertebral body and partial laminectomies of the adjacent segments (Fig. 46.1A).
– 7. Decancellate and resect pedicle while contralateral temporary rod is in place.
– 8. Resect (chisel or drill) a posterior wedge out of vertebral body (Fig. 46.1B).3
– 9. Repeat steps 5 and 6 on the contralateral side.2
– 10. Resect remaining posterior vertebral body cortex; impact bone into cavity previously created during wedge resection of vertebral body with angled bone tamp or down-going curette.2
– 11. Use fluoroscopy to confirm adequate resection in addition to visual inspection.3
– 12. Compress across pedicle screws to close down osteotomy (Fig. 46.1B).
– 13. Evaluate neurophysiologic monitoring and/or wakeup test to ensure absence of neurologic compromise.
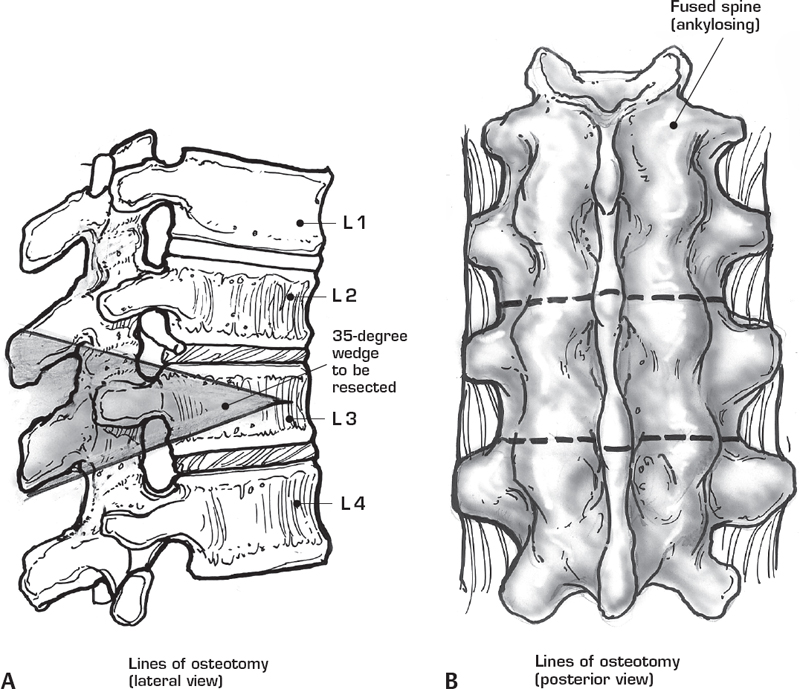
Fig. 46.1 (A, B) Pedicle subtraction osteotomy. (From Haher R, Merola A, Surgical Technique for the Spine, Thieme; pg. 234, Fig. 50-3A,C.)
Smith-Petersen Osteotomy
– 1. Position on Jackson frame with extended chest bolster.
– 2. Consider use of multimodal neurophysiologic monitoring to minimize neurologic complications during deformity correction.
– 3. Place pedicle screw instrumentation across targeted segments.
– 4. Remove interspinous ligaments with rongeur.
– 5. Spinous processes are removed at each targeted segment in a 45 degree angle in addition to removal of the upper and lower lamina edges.
– 6. Bilateral facetectomies are performed with osteotomes and/ or a high-speed drill4 (Fig. 46.2A).
– 7. Remove ligamentum flavum.
– 8. Compress across the screw heads to close the osteotomy4(Fig. 46.2B).
– 9. The patient may be placed in extension to assist in closure of the osteotomy.4
IV. Complications
– Neurologic injury due to iatrogenic spinal stenosis upon closure of the osteotomy
– Spinal subluxation during osteotomy
– Durotomy
– Hypotension due to excessive blood loss during osteotomy; avoid hypotension especially during correction maneuvers as spinal cord ischemia may result
– Epidural hematoma
– Vascular injury
– Pseudarthrosis
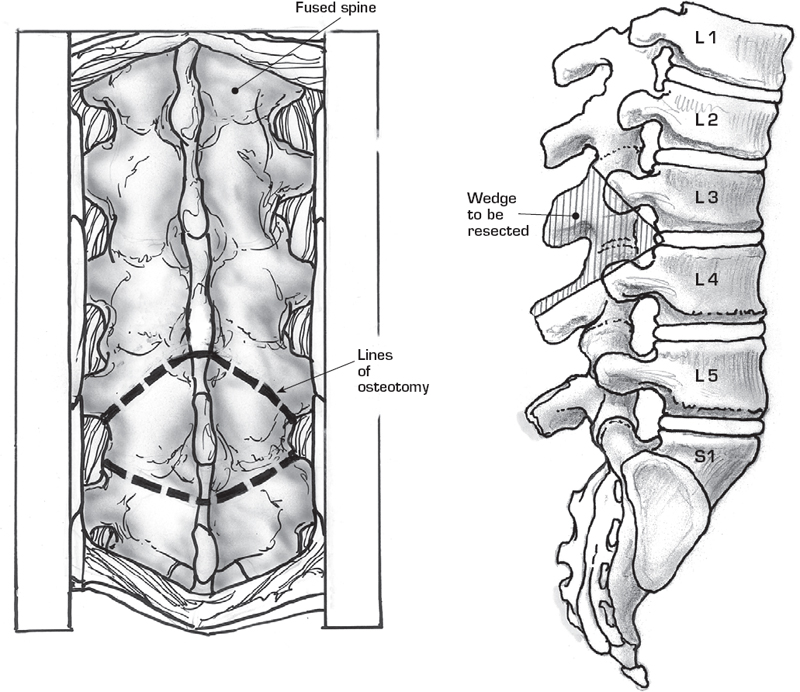
Fig. 46.2 (A, B) Smith-Petersen osteotomy. (From Haher R, Merola A, Surgical Technique for the Spine, Thieme; pg. 228, Fig. 49-1A,B.)
V. Postoperative Care
– Immediate neurologic evalution upon wakeup
– Admission to neurologic intensive care for close monitoring
– Maintenance of blood pressure
– Consider postoperative computed tomography (CT) scan to evaluate adequacy of bone resection and juxtaposition of osteotomy margins.
VI. Outcomes
– With PSO, average curve improvements are 61 degrees in scoliosis cases, 56 degrees in global kyphosis cases, and 51 degrees in angular kyphosis cases.4
– Clinical and radiographic outcomes are superior with PSO in the lumbar spine rather than in the thoracic. The lower the PSO is performed, the less angulation is required for sagittal balance correction.1
– In properly selected patients, sagittal balance can be restored with PSO or multiple SPO safely.
VII. Surgical Pearls
– Ensure that bone resection is adequate and wide enough laterally in both PSO and SPO to prevent interference upon osteotomy closure or compression of neurologic structures.
– Use thrombin powder or bioabsorbable bone wax to minimize bleeding during PSO without compromising fusion rates. Aprotinin is also an option, although controversy exists over possible associated complications.
– Do not resect the anterior vertebral wall entirely during PSO, as it will serve as a hinge during pedicle screw compression and osteotomy closure and prevent vertebral segment subluxation.
– Posterior laminectomy resection should be complete and include any epidural scar removal to assess dural sac adequately after osteotomy closure and ensure there is no spinal canal compression.
– During SPO closure, place patient in extension to lengthen the anterior spinal column and facilitate osteotomy closure and to minimize strain on the pedicle screw construct.
Common Clinical Questions
1. How many degrees of correction can be achieved with PSO as opposed to SPO?
2. What is the main advantage of a PSO/SPO procedure?
3. In regard to the anterior and middle columns, what is the main difference between PSO and SPO?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







