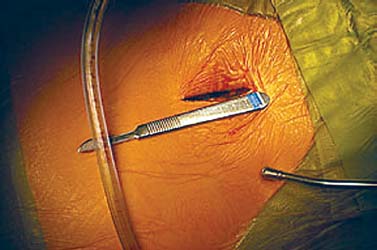
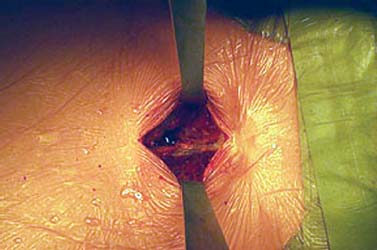
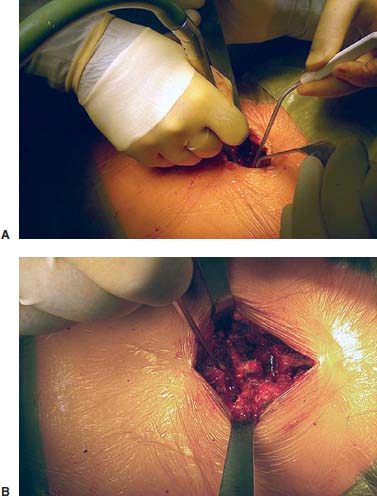
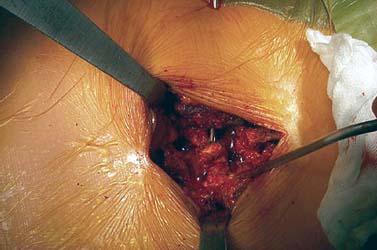
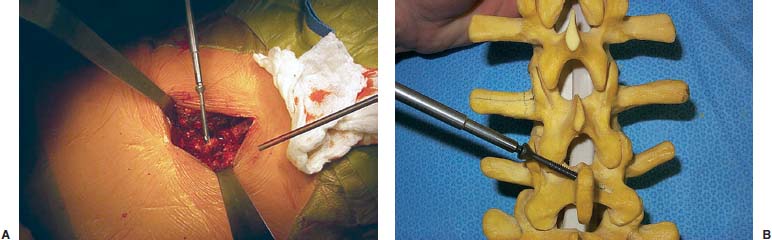
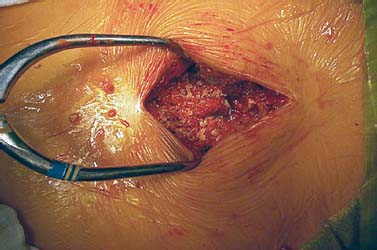
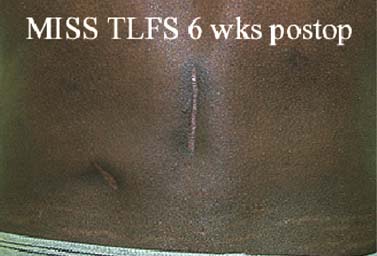
Translaminar facet screws (TLFSs), invented by Magerl for posterior stabilization, were first described by Montesano et al in 1988.1 In 1998, Rathonyi et al2 reported their findings from a biomechanical study that comprised an intact human cadaver spine versus TLFS alone, versus Bagby and Kuslich (BAK) cages alone, versus TLFS + BAK cages at both one and two levels. They noted: “The combination of the excellent stabilizing effect of an anterior cage in axial compression, flexion, and lateral bending, with the stabilizing effect of TLFS fixation in extension and axial rotation seem optimal from a biomechanical perspective.” In another biomechanical study in 1998, Deguchi et al3 compared TLFSs with pedicle screws in a human cadaver model. They described TLFS fixation as having “similar biomechanical performance to pedicle screw fixation.” Multiple investigators have reported excellent clinical results with a high rate of fusion using TLFS in a circumferential fusion model.4–12 TLFS fixation involves placing screws through the base of the spinous process, through the lamina, and into the facet joint in a criss-cross fashion. This is instrumental in completing the tension band, which is the goal of a circumferential instrumented environment. TLFSs are inherently less invasive than transpedicular screws, and implantation through a minimally invasive approach improves upon this concept. The importance of a minimally invasive approach to TLFS fixation cannot be overstated. The use of TLFS in lieu of transpedicular fixation is ineffective if taking down of the paraspinous muscles occurs, as with a traditional open midline approach for transpedicular fixation. If the paraspinous muscles are sacrificed with the approach, a poor biomechanical environment for healing is created, both for the fusion mass and for the return of normal function of the low back (W. Rauschning, personal communication). The introduction of TLFS has reduced the use of pedicle screws by 70% in the senior author’s (JMG) practice. In an environment of managed care and escalating surgical costs, TLFSs are, on average, 75% less expensive per level compared with pedicle screw systems currently on the market. The senior author currently uses TLFSs approved for use in the spine by the U.S. Food and Drug Administration (Discovery; DePuy AcroMed, Raynham, MA). Prior to the FDA approval of this device, 4.5 mm cancellous bone screws were used as an off-label device. Indications The following are indications for percutaneous translaminar facet screw fixation: FIGURE 25–1 (A) The Discovery Translaminar Facet Screw Set (DePuy AcroMed, Raynham, MA), FDA-approved for use in the lumbar spine. (B) A close-up view of a titanium translaminar facet screw, which includes a hollow core. Contraindications Contraindications for the procedure include: Surgical Procedures Surgical Equipment FIGURE 25–2 The patient is placed in the prone position on a Jackson table. Preoperative fluoroscopy is used to identify the appropriate level for the approach. Operating Room Setup A standard setup for posterior lumbar surgery is used, with the spine surgeon standing on the left or right side of the patient, depending on the pathology, and with one surgical technician and one surgical assistant. Patient Positioning The patient is placed in the prone position on a Jackson table. Following general anesthesia, the patient is draped and prepped in the standard fashion, and preoperative antibiotics are given. Fluoroscopy is used to find the landmarks of the appropriate lumbar level (Fig. 25–2). The skin is marked, identifying the level(s) to be addressed. Surgical Technique Great care is taken to limit the midline incision to 2.5 to 5.0 cm (Fig. 25–3). The incision should be made as small as possible without dissecting or denervating the paraspinous muscles. Posterior retractors are then placed at the edge of the incision laterally on each side (Fig. 25–4). A laminoplasty-type decompression must be performed. The laminar arch and at least 50% of the facet joints must also be left intact (Fig. 25–5). Following decompression, percutaneous incisions are made to the left and right, lateral and cranial to the midline incision. The surgeon stands on the left side of the patient. A 3.2 mm drill is placed through the incision (Fig. 25–6) to the base of the spinous process. A hole is drilled through the base of the spinous process, across the lamina, and to the contralateral facet joint, from left to right (Fig. 25–7). This is then repeated from right to left, with the surgeon standing on the right side of the patient. Once this is completed, the drill bit is changed to a screwdriver bit, and the appropriate-length screws are selected. The screws can be placed either through the lateral percutaneous incisions or through the midline incision, with power, depending on the anatomy and surgeon’s preference (Fig. 25–8). Following screw placement (Fig. 25–9), bone graft is placed in the midline (Fig. 25–10), not in the lateral gutters, which are not exposed with this approach. FIGURE 25–3 A 2.5 to 5.0 cm midline incision is made. The size of the incision does not change for a two-level procedure. FIGURE 25–4 Posterior retractors are placed bilaterally at the lateral edges of the incision. FIGURE 25–5 (A) Standard instruments (e.g., a Midas Rex drill) can be used through this minimally invasive incision. A laminoplasty-type decompression technique is necessary for this approach. (B) The laminar arch must be kept intact, and there cannot be more than 50% removal of the facet joints. FIGURE 25–6 Small percutaneous incisions are placed above and lateral to the primary incision. The drill is placed through this incision. FIGURE 25–7 The drill is shown penetrating the base of the spinous process and across the lamina. FIGURE 25–8 (A) The screw can be placed either through the percutaneous lateral incisions or directly through the midline incision. (B) Sawbones model view of implantation of the screw from left to right. FIGURE 25–9 (A) Perioperative anteroposterior view of a completed one-level construct. (B) Sawbones model anteroposterior view of a completed one-level construct. (C) Sawbones model lateral view of a completed one-level construct. Postoperative Care Patients who undergo either circumferential minimally invasive instrumented fusion or only minimally invasive translaminar fixation are discharged from the hospital 1 to 3 days postoperatively. The posterior incision heals completely in 6 weeks (Fig. 25–11). Patients are placed in a Neoprene lumbar corset for at least 4 weeks postop. They begin aquatic physical therapy at 10 to 14 days postop and advance to weight training, treadmill, and range-of-motion therapy as tolerated. Return to work depends largely on the patient’s motivation and occupational circumstances (Fig. 25–12). FIGURE 25–11 Healed incisions at 6 weeks following surgery. The smaller incision in the lower left quadrant is from the minimally invasive bone graft harvest of the posterior iliac crest. FIGURE 25–12 Anteroposterior (A) and lateral (B) radiographs of a 50-year-old male patient at 29 months postop with notable fusion. The patient presented with internal disk disruption and degenerative disk disease at L4–L5 and L5–S1. Femoral rings were implanted anteriorly via a gasless endoscopic approach. The patient had a 70% reduction in pain and returned to work at 5 months following surgery. Complications and Avoidance Nerve Root Irritation Caused by the Screw Care must be taken to place the screws subforaminally to avoid irritation of the nerve root. If a patient develops a radiculopathy postoperatively, a CT scan should be obtained to discern the presence or absence of nerve root impingement. If nerve root impingement or irritation is evident, percutaneous removal of the screw is advised. Immediate postoperative CT scans are helpful in assessing any nerve root irritation issues if the patient awakens in the recovery room with burning radiculopathy. Inadequate Decompression The laminoplasty-type decompression may be difficult to accomplish in some patients. If the decompression cannot be performed in this manner, a standard laminectomy or laminotomy should be performed with transpedicular fixation. These cases are rare. Malposition of the Screw Perioperative imaging should be used to verify alignment and placement of the screws. If the placement of a screw is suboptimal, the screw should be removed and reimplanted in the proper position. Translaminar facet screw fixation using a minimally invasive approach can be done in place of transpedicular fixation for an instrumented circumferential lumbar fusion at one or two levels. TLFSs are inherently less invasive than transpedicular screws, and they are less expensive per level compared with pedicle screw systems. Other indications for use of TLFS include stabilization following laminoplasty-type decompression at one or two levels and as adjunctive fixation at the middle levels of a transpedicular fixation construct for the treatment of fracture. REFERENCES
25

Percutaneous Translaminar Facet Screw Fixation






< div class='tao-gold-member'>
Percutaneous Translaminar Facet Screw Fixation
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








