52 Posterior and Transforaminal Lumbar Interbody Fusion (PLIF/TLIF) (Open)
I. Key Points
– Arthrodesis across one or more vertebral disc spaces is indicated in conditions that produce spinal instability.
– Bilateral posterior lumbar interbody fusion (PLIF) may be performed at L5-S1 with less potential for neural injury due to the enlarged capacity of the neural canal at this level.
– A primary advantage of the transforaminal lumbar interbody fusion (TLIF) procedure over PLIF is the reduction in nerve root retraction, and thus in neural complications.
II. Indications
– Spondylolisthesis grade I or II
– Reoperation for pseudarthrosis
– Degenerative disc disease causing discogenic low back pain
– Recurrent disc herniation with mechanical back pain, or recurrent radiculopathy
– Lumbar deformity with coronal or sagittal plane imbalance
– Neural foraminal stenosis from disc space collapse
III. Technique
Transforaminal Lumbar Interbody Fusion
– Exposure of the disc space
• Expose the vertebral spinous process and lamina of the levels above and below the operative disc space using lateral x-ray to confirm the anatomic level. In the case of a L4-L5 TLIF, the medial facet joint (inferior articular process) of the L4/L5 interspace on the primary symptomatic side is removed.
• This is performed with a high-speed drill or osteotome to create a sagittal cut in the lamina and a transverse cut through the pars interarticularis directly over the exiting nerve root at the inferior aspect of the pedicle of the index neural foramen.
• The joint capsule and ligamentum flavum can be detached with monopolar electrocautery. A Leksell rongeur is used to remove the medial facet, which is morselized for fusion autograft. The superior (or lateral) facet of the caudal level is then removed with a Kerrison rongeur until the superior aspect of the next pedicle is encountered. Care must be taken to avoid injury to the exiting nerve root within the foramen at this level.
• The shoulder of the traversing nerve root is visualized exiting the thecal sac at the level of the disc space. The medial and superior borders of the caudal pedicle limit the amount of the superior facet that can be removed. A high-speed drill can be used to shave bony osteophytes to optimize the trajectory into the disc space and minimize nerve root retraction during interbody graft placement.
– Discectomy
• The discectomy is performed by incising the annulus with a scalpel and then using curettes and pituitary rongeurs to remove the nucleus pulposus and cartilaginous end plates, thus exposing the bony surface of the vertebral end plates for fusion.
• Preservation of the bony end plates will serve to prevent graft subsidence into the cancellous portion of the vertebral body.
– Interbody grafting
• An interbody graft of the appropriate size is packed with autograft or other fusion substrate1 and carefully impacted into the disc space.1 A nerve retractor is placed against the traversing nerve root shoulder to protect it during graft placement.
• The interbody graft should not protrude beyond the dorsal aspect of the adjacent vertebrae.
– Pedicle screw placement
• The pedicle screw entry point is indicated by the mamillary process: the junction of the transverse process, superior facet, and pars interarticularis. The lateral to medial trajectory varies generally from 5 to 20 degrees from L1 to L5 (i.e., 5 degrees at L1 and increasing at 5 degree increments per caudal level).
• The rostral to caudal trajectory should parallel the pedicle as directed by palpation with a Woodson-Adson or similar instrument if a decompression has been performed, or alternatively, using intraoperative fluorscopy or image guidance.
• Once the pedicle screws have been placed, a lordotic rod is inserted and the cap screws are tightened with compression across the screw heads. This restores lordosis and compresses the interbody graft to prevent graft migration and facilitate fusion.
– Closure
• A multilayer closure is performed using absorbable sutures in the lumbodorsal fascia and subdermis. Staples or nylon suture is used to close the skin.
• If a surgical drain has been left in the wound, it is secured to the skin with suture and the wound is covered with an appropriate dressing.
Posterior Lumbar Interbody Fusion
– The PLIF procedure is similar to TLIF with respect to exposure, discectomy, and closure.
– The key difference is that the approach to the disc space is more medial and a portion of the facet remains, necessitating neural element retraction for discectomy and interbody graft placement (Fig. 52.1).2
– Laminectomy is routinely performed with a high-speed drill and rongeurs, following which the ligamentum flavum is resected to expose the thecal sac. Bilateral foraminotomies are routinely performed with a Kerrison rongeur to ensure adequate nerve root decompression, but the distal aspects of the roots themselves are not typically exposed as in the TLIF procedure.
– Once visualization has been accomplished, a dural retractor is used to medialize the neural elements and expose the underlying disc space.
– The discectomy, graft placement, and pedicle screw construct techniques are similar to those for the TLIF technique. Careful attention must be paid during intervertebral work to limit medial retraction of the neural elements. 3
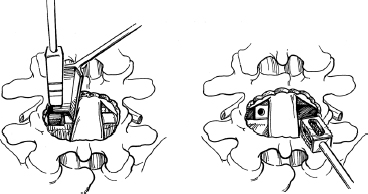
Fig. 52.1 An implant filled with cancellous bone graft is inserted into the rectangular channel. Note the teeth of the cage that engage the vertebral bone. (From Fessler R, Sekhar L, Atlas of Neurosurgical Techniques, Thieme; pg. 686, Fig. 95-3B.)
IV. Complications
– Dural tear (5 to 14%) can occur at any stage of the procedure, but most commonly occurs during the thecal sac and nerve root exposure.4
– Nerve root injury secondary to retraction has been reported in up to 13% of cases, with resultant radiculopathy, typically transient.
– Vascular injury during the discectomy, typically from breach of the anterior longitudinal ligament, requires packing of the disc space, emergency closure, and vascular consult for laparotomy and/or interventional repair of the injured vessel.
– Infection (1 to 5%), typically with skin flora
V. Postoperative Care
– Mobilize early; consider deep vein thrombosis (DVT) prophylaxis if patient is not ambulating on post-op day 1.
– Pain management with patient-controlled administration of narcotics augmented with muscle relaxants, and transition early to oral medications
– Discontinue wound drain based on output (e.g., less than 100 ml in 24 hours).
VI. Outcomes
– Clinical success rate is typically 75% for relief of mechanical back pain and radiculopathy.
– Fusion rates around 90% have been reported in multiple series.5
VII. Surgical Pearls
– Strict dissection along the periosteum minimizes blood loss.
– PLIF procedures may be more suited to the L5 to S1 disc space.
– Nerve root retraction can be reduced or eliminated with the more lateral to medial trajectory of the TLIF procedure.
– The introduction of pedicle screw and rod constructs has reduced the incidence of pseudarthrosis from TLIF and PLIF procedures.
Common Clinical Questions
1. A patient with known tethered cord would be better suited for which lumbar interbody fusion procedure?
2. The pars interarticularis is transected completely in which lumbar interbody fusion procedure?
3. The lateral to medial trajectory is greatest for pedicle screws inserted at which lumbar level?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







