Cardiac right-to-left shunt (atrial septal defect) is demonstrated using color Doppler transesophageal echocardiography.
Focused questions
How is a cTCD study for RLS detection usually performed?
Which cTCD findings indicate the presence of a RLS, shunt size and site?
Is RLS detection by cTCD useful in conditions not related to cardiac RLS and in diseases other than stroke?
Is there a clinical consequence of RLS detection by cTCD in stroke patients?
Imaging tips
TCD requires technical expertise and accurate interpretation of the test results. The results may vary considerably depending on methodological factors; therefore, in order to minimize variability, a standardized approach for RLS detection by cTCD was established by international Consensus Meetings [15,16,17]. Recommendations are available also from publications summarizing the impact and technique of cTCD for the diagnosis of PFO [18,19,20].
Identification criteria of contrast-induced microembolic signals (MES): the basic principle for the detection of an RLS by cTCD is that intravenously injected gas bubbles are detected within the Doppler frequency spectrum of the insonated intracranial artery. Under physiological conditions these gas bubbles are normally stopped and trapped in the lung and they dissolve. In the presence of a cardiac or pulmonary RLS, gaseous emboli pass from the right into the left atrium, and from there into the systemic circulation including the brain. These MES are detectable by cTCD and lead to the diagnosis of RLS. International standards for the identification criteria of emboli by TCD have been established [16,17]. MES appear within the Doppler spectrum as unidirectional, high-intensity signals of short duration and characteristic sound (Table 16.1). It is recommended to decrease the gain amplitude and sample volume to detect the MES more accurately.
| a. Transient, short duration, usually lasting <300 ms (<0.01–0.03 s) |
| b. Intensity increase within the Doppler frequency spectrum. Doppler amplitude is at least 3 decibels higher than the backround blood flow. Intensity increase is focused around 1 frequency |
| c. Unidirectional within the Doppler velocity spectrum |
| d. Characteristic acoustic output (clicking, chirping or whistle sound) |
The detection of microemboli is based on the measurement of the backscatter from the emboli. The backscatter of the ultrasound from gaseous emboli is usually higher than the backscatter from solid emboli of similar size [17] with a typical bidirectional appearance of the signal (Figure 16.2).
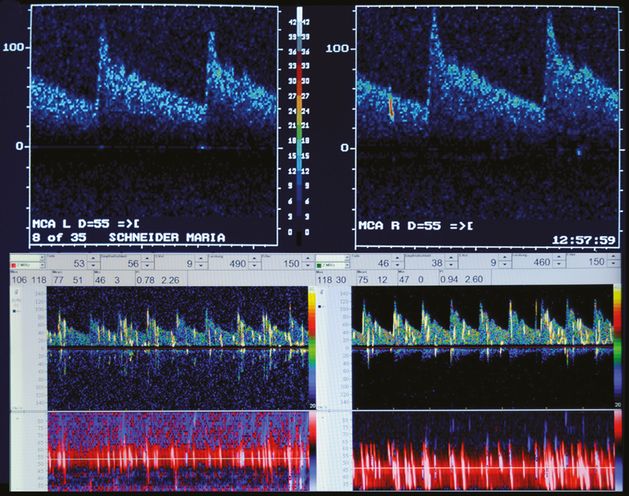
Simultaneous bilateral TCD monitoring of the middle cerebral arteries. Upper images: spontaneous solid emboli originating from a severe ipsilateral internal carotid stenosis. Lower images: typical bilateral and bidirectional appearance of gaseous emboli after contrast injection in a patient with patent foramen ovale.
Microbubble (Mb) signal duration was found to be higher than measured for solid emboli [21]. However, at present no reliable conclusion as to the composition and the size of an embolus can be drawn from the echo of the embolus and there is agreement that no current system of automatic embolus detection has the required sensitivity and specificity for clinical use [17].
Choice of contrast agent: the diagnosis of RLS using cTCD is based on the application of air-containing echo contrast agents (CAs). Two CAs were used routinely. Publications focused mainly on agitated saline solution or D-galactose Mb solution (Echovist®); only few authors utilized other media such as oxypolygelatine. The 2000 Consensus Meeting recommendation indicated the use of a saline/air mixture, since it was not subject to local approval rules and it had proved effective in numerous studies; the usage of Echovist® in countries where it was available, had to be considered according to local regulations [15]. However, in the meantime, Echovist® has been out of the market in most countries because it is no longer commercially available. Several reports exist about allergic reactions to gelatine-based plasma expanders; also, a severe anaphylactic reaction to Gelofusine®, as part of a transthoracic echo study to determine if there was a PFO, has been described [22].
Ultrasound system: although embolic signals are detectable by using duplex ultrasound, a higher sensitivity is achieved by performing the RLS detection with Doppler sonography. Bilateral recordings (simultaneous bilateral TCD monitoring) increase the sensitivity when compared with unilateral insonations [11,23].
Steps of investigation
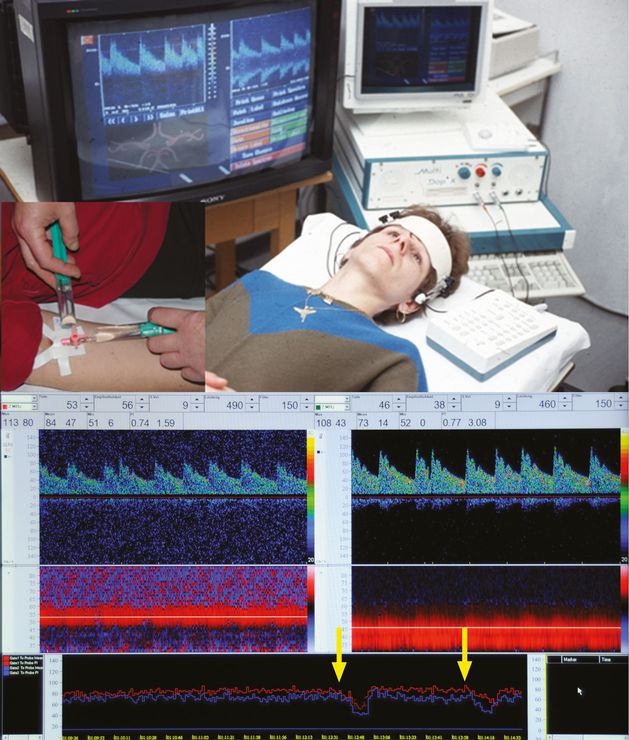
The patient is in a supine position with one arm placed horizontally.
An 18-gauge needle – preferred over a 20-gauge needle to increase the sensitivity [24] – is inserted into the (right) cubital vein.
At least one (better both) middle cerebral artery (MCA) is insonated. A 2-MHz TCD probe is placed over the temporal bone window and held in position manually (unilateral TCD monitoring). In case of bilateral monitoring, the two probes are fixed by a head frame (simultaneous bilateral TCD monitoring). The MCA is monitored usually at a depth of 5–6 cm.
In case of insufficient acoustic bone window, transforaminal insonation of the basilar artery or insonation of the extracranial internal carotid artery represent alternative approaches.
After adjusting the probe and verifying the quality of the Doppler signal, data storage is recommended for off-line analysis.
An initial recording of at least 20 minutes for the detection of spontaneous emboli originating from a carotid stenosis or due to atrial fibrillation is recommended. Simultaneous bilateral TCD monitoring helps to localize the source of the embolization.
The CA is prepared. For the agitated saline/air mixture, a syringe with 9 ml of saline (physiologic solution) and a syringe with 1 ml of air are used. Both syringes are connected with the patient using a three-way stopcock which is in turn connected to an intravenous line by means of a short flexible line. The air/saline mixture is exchanged vigorously between the syringes at least ten times. The injection has to be performed as a bolus and immediately after CA preparation. Commercially traded contrast agents should be prepared according to the manufacturer´s instructions.
Valsalva maneuver (VM): in case of a negative test result (no detection of MES at the MCA level), the test should be repeated performing a VM. Before contrast application, the patient should be trained in order to perform an effective VM. The VM is defined as an inhalation, followed by an exhalation against the closed glottis, ensuring an increase of the thoracic pressure and right atrium pressure. The pressure gradient between the right and left atrium allows right-to-left shunting through the PFO. Correct performance of the VM can be controlled by observing the decrease of the MCA peak flow velocity (TCD envelope): the VM is considered effective when there is a peak systolic velocity reduction of >25% in the MCA.
The patient should start the VM on the examiner’s command 5 seconds after injection of the CA, and the duration of the VM should be at least 5–10 seconds (Figure 16.3).
Evaluation of test results
Diagnosis of a RLS by cTCD
The diagnosis of a RLS by cTCD is established if at least one contrast-induced MES is observed on the TCD trace after contrast injection (Figure 16.4).
Positive testing without VM performance ensures a permanent RLS. Latent or functional shunting is assumed if the contrast study is positive only during Valsalva straining (Figure 16.5).
The number of embolic signals and the time interval between the beginning of contrast injection start and the appearance of the first MES in the MCA has to be documented.
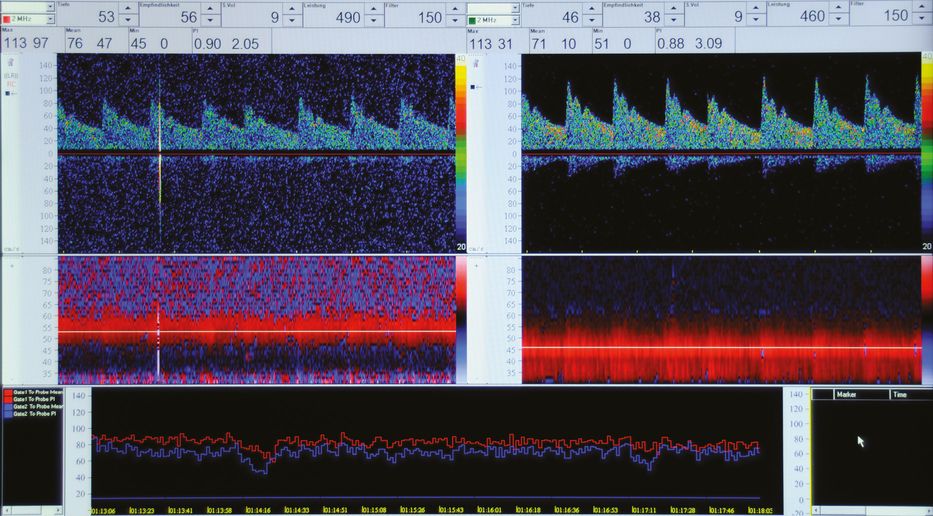
Single microembolic signal observed on the TCD trace after contrast application in a patient with pulmonary RLS.
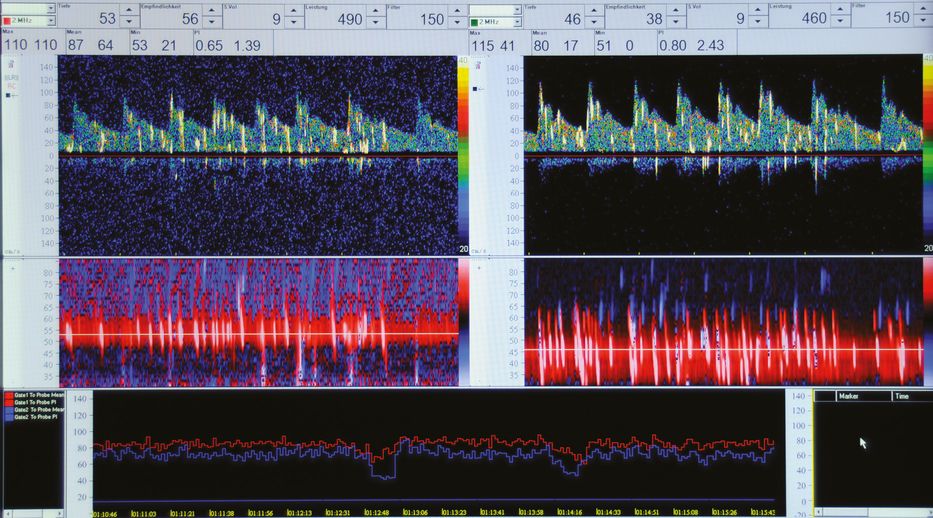
Multiple microembolic signals on the TCD trace after contrast injection indicate massive shunting in a patient with patent foramen ovale.
Estimation of the shunt size and shunt localization
Estimation of the size and grade of the RLS is achieved by assessing the amount of contrast shunted [20,25] (Table 16.2 and Figure 16.6).
| Unilateral TCD monitoring | Bilateral TCD monitoring | |
|---|---|---|
| Cat 1 shunt negative | No microbubbles | No microbubbles |
| Cat 2 low-grade | 1–10 | 1–20 |
| Cat 3 medium-grade | >10 | >20 |
| Cat 4 high-grade | Shower | Shower |
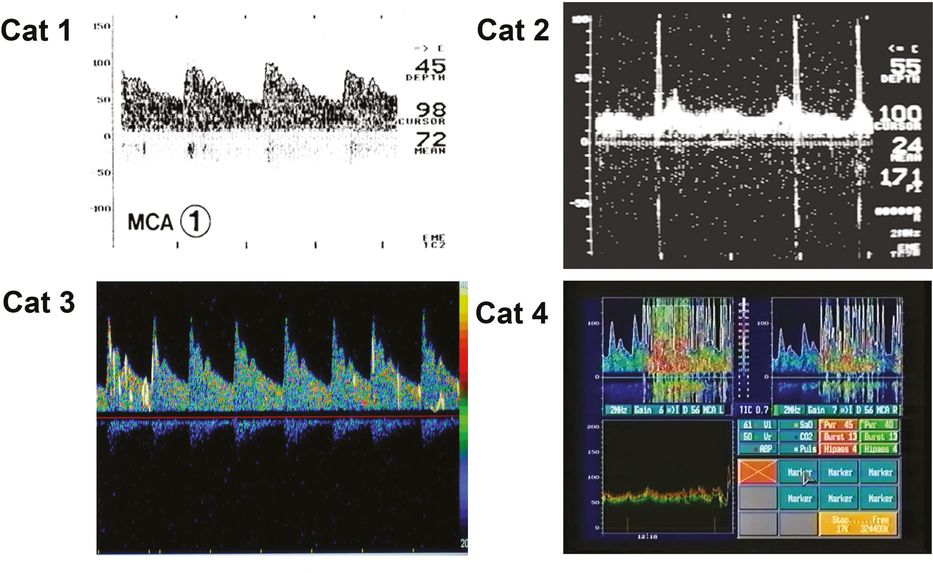
Quantification and categorization of right-to-left shunts by contrast TCD monitoring.
cTCD allows an estimation of the shunt size by quantification and categorization of the contrast shunted and is comparable to cTEE [10,26–30]. However, the clinical significance of cTCD shunt sizing still remains unclear. Several authors consider a large PFO and a high degree of RLS to be associated with a higher risk of stroke [26,31–35] – particularly of cryptogenic stroke [27] – and with a significant stroke recurrence rate [36]. In contrast, results from a prospective multicenter study showed that a massive RLS as defined by cTCD was not an independent risk factor for recurrent stroke [28].
Following the hypothesis that contrast passing through a pulmonary shunt appears later and is smaller than contrast shunted via a cardiac RLS, several authors sought to define a “cut-off time-interval” and MES-count limit capable of discriminating between the two types of RLS. According to some reports, an intracardiac communication rather than a pRLS is suggested if MES appear early, within 6–10 cardiac cycles or 4–40 seconds, after contrast application [37–41]. A minimum amount of MES suggestive of a clinically relevant RLS is not yet established [15]. However, the fact that a single embolic event was found by TCD in patients with PFO is in concordance with previous reports in which the threshold for a positive TCD examination was set at one MES [41,42]. In summary, although the delayed appearance of only a small amount of contrast is more suggestive of shunting at the pulmonary level, definitive differentiation by cTCD is not feasible.
Value of contrast transcranial Doppler RLS detection in other diseases than stroke
The impact of cTCD in RLS detection has been studied in numerous conditions not related to cardiac RLS and in diseases other than stroke, considered to be associated with paradoxical embolism; the grade of evidence from these studies is low to moderate. A significant association was reported between the degree of RLS quantified by cTCD and the number of magnetic resonance imaging infarctions in asymptomatic sport divers [43]; also, a higher risk of decompression sickness was observed in divers with RLS [44]. There is evidence of an increased prevalence of PFO in patients with migraine with aura supported by cTCD studies [45,46]; cTCD demonstrated that PFO was significantly more prevalent in children suffering from migraine with aura than in those suffering from migraine without aura [47]. High counts of cTCD-detected MES associated with RLS have been also observed during orthopedic surgery [48]. Finally, cTCD has been described to be a useful tool in detection of residual shunting after transcatheter closure of a PFO [49].
Clinical usage of contrast transcranial Doppler RLS detection in stroke patients
TCD cannot replace echocardiography. TEE is required in all cryptogenic stroke patients, particularly in those of younger age, to confirm the site of the shunt (cardiac or extracardiac) and to assess PFO size, presence of ASA, left atrial thrombus, other cardiac abnormalities or severe atherosclerosis of the aortic arch. However, TEE depends on the patient’s cooperation and ability to swallow the ultrasound probe. TCD may serve as an alternative method if TEE is not applicable or available. It serves as an ideal, noninvasive bedside screening method for the detection and sizing of RLS and can be useful during the acute phase of routine ischemic stroke workup in order to identify the pathogenic mechanisms of stroke and to make timely decisions to perform TEE.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree