6 Sacral-Iliac Spine
I. Key Points
– The sacrum is the structural link that distributes load from the lumbar spine to the pelvis through the sacroiliac joints (and vice versa).
– The bulbocavernosus reflex involves the S2 to S4 sacral nerves, and its absence or presence has prognostic significance in spinal cord trauma.
– Because of the location of the lumbosacral plexus in relation to the sacrum, sacral fractures have a high incidence of neurologic injury (up to 25%).1
II. Bony Anatomy
– The normal adult spine consists of five fused sacral vertebrae that form the wedge-shaped sacrum and four fused coccygeal vertebrae that form the coccyx (the skeletal remnants of a tail).
– The sacrum has four paired sacral foramina, a sacral canal, a sacral promontory (anterior projection of the S1 body), and a sacral hiatus (clinically useful for caudal epidural anesthesia)2(Figs. 6.1 and 6.2).
– The sacroiliac (SI) spine has many palpable bony landmarks, including the sacral cornu and the iliac crest. The posterior superior iliac spine may be difficult to palpate but is readily identifiable by the permanent skin dimples above the buttocks.3
• An imaginary line connecting the dimples passes through the S2 spinous process and the middle of the SI joint in the anterior-posterior plane.
• An imaginary line connecting the highest points of the iliac crest passes through the L4/L5 intervertebral disc space.
– The sacrum has multiple points of articulation:
• The S1 body articulates with the L5 body via the L5/S1 disc to form the lumbosacral angle, which varies from 130 to 160 degrees.3
• The inferior facet of L5 articulates with the superior facet of S1 and acts as a buttress to resist anterior translation.3
• The apex of the sacrum articulates with the coccyx.
• The lateral aspects of the sacrum articulate with the two coxal (innominate) bones to form the SI joint (a true synovial diarthrodial gliding joint with limited motion). Only the anterior 25% is synovial in nature (the rest is ligamentous attachment).1
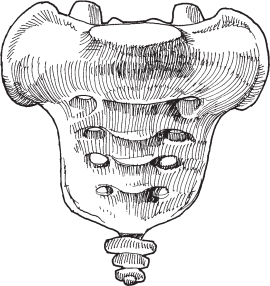
Fig. 6.1 Anterior view of the bony sacrum.

Fig. 6.2 Posterior view of bony sacrum/pelvis with the ligamentous attachments to the pelvis.
III. Neural Anatomy
– Ventral and dorsal branches of the sacral nerves exit the four pairs of anterior and posterior sacral foramina, respectively; the anterior foramina are larger in caliber than their posterior counterparts.2
• Dermatomes are supplied by sacral nerves (Fig. 6.3).
– The sacral canal contains the nerve roots of the cauda equina.
– The pelvic splanchnic nerves are composed of parasympathetic fibers derived from S2 to S4 and supply autonomic innervation to various abdominal and pelvic viscera.
– The lumbosacral plexus is composed of the ventral rami from T12 to S3 and lies posterior to the psoas muscle.
– Following are major nerves that arise from this plexus3:
• Sciatic nerve: composed of the ventral rami from L4 to S3, it has an anterior preaxial tibial division and a postaxial peroneal division; most commonly it exits the pelvis via the greater sciatic foramen inferior to the piriformis muscle.
• Pudendal nerve: composed of the anterior divisions of the ventral rami of S2 to S4, it supplies the perineum and external genitalia.
• Superior gluteal nerve: composed of the posterior divisions of the ventral rami of L4 to S1, it supplies the gluteus medius, gluteus minimus, and tensor fascia lata.
• Inferior gluteal nerve: composed of the posterior divisions of the ventral rami of L5 to S2, it courses with the inferior gluteal artery to supply the gluteus maximus.
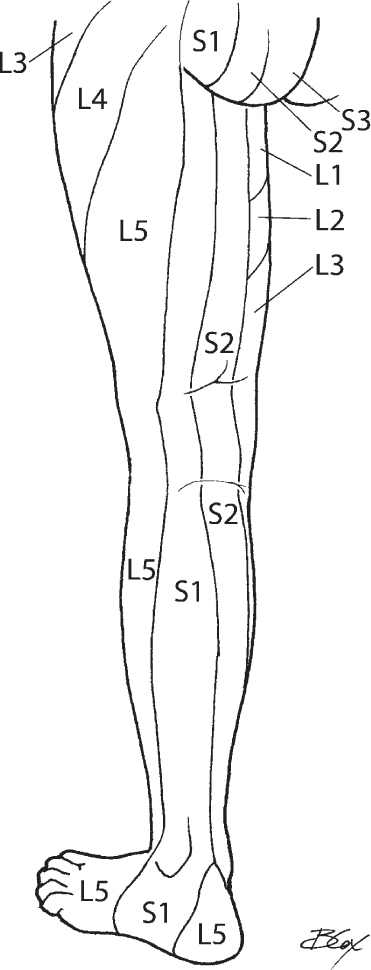
Fig. 6.3 Dermatomal map of sacral nerve roots.
IV. Vascular Anatomy
– The abdominal aorta begins at the aortic hiatus in the diaphragm at the level of T12 and bifurcates into the common iliac arteries at the level of L4.3
– The common iliac veins unite at the level of L5 to form the inferior vena cava.3
– The common iliac artery bifurcates anterior to the SI joint to form the internal iliac artery and descends posteriorly into the greater sciatic foramen to supply the pelvis, buttocks, medial thigh, and perineum.
• The internal iliac vein sits between the SI joint and the internal iliac artery.
– The median sacral artery and vein form an unpaired vessel that originates from the posterior aspect of the abdominal aorta to supply the lower lumbar vertebrae, sacrum, and coccyx.3
– The lateral sacral arteries are paired and branch from the internal iliac artery and course through the anterior sacral foramina to supply the spinal meninges.3
V. Ligamentous and Muscular Anatomy
– The iliolumbar ligament attaches the transverse process of L5 with the ilium.2
• Unstable vertical shear fractures can avulse off the L5 transverse process.
– The anterior SI, posterior SI, and interosseous ligaments suspend the sacrum between the ilia.3
• The posterior SI and interosseous ligaments are thicker and limit motion.
– The sacrotuberous ligament attaches the sacrum to the ischial tuberosity; the sacrospinous ligament attaches the sacrum to the ischial spine.
• These ligaments function to limit upward movement of the caudal portion of the sacrum and delineate the greater and lesser sciatic foramina.
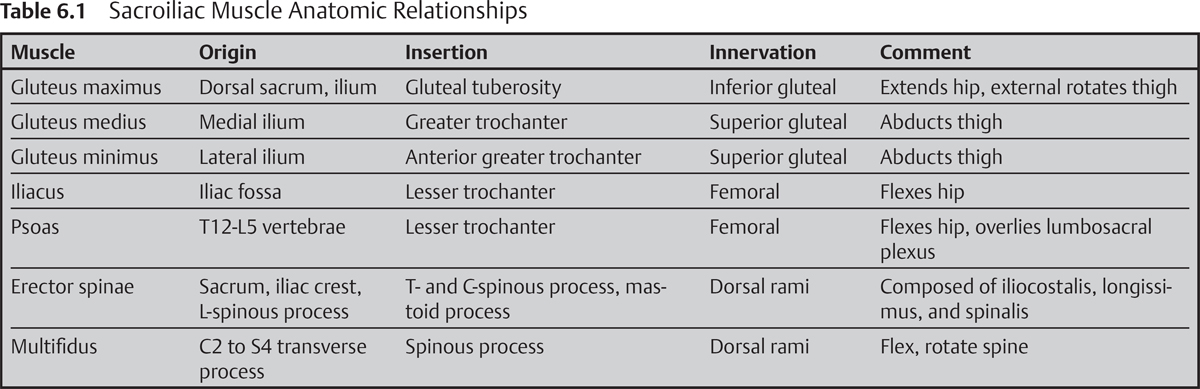
– See Table 6.1 for major muscles of the sacroiliac spine.
VI. Surgical Pearls
– Transitional vertebrae can lead to incorrect surgical localization.2
– Aggressive exposure of sacral ala for posterolateral fusion can endanger the L5 nerve root.1
– A low L5-S1 disc may not be accessible via an anterior approach due to pubic symphysis obstruction.2
– Anterior dissection of the superior hypogastric sympathetic plexus can result in retrograde ejaculation in males, with rates ranging from 0.42 to 5.9%.4
1. Of the listed nerves, which is the most susceptible to injury during an anterior approach to the SI joint?
A. S1 nerve root
B. Femoral
C. Ilioinguinal
D. L5 nerve root
E. Genitofemoral
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







