Fig. 46.1
Sinonasal adenocarcinoma. Coronal MRI shows an invasive mass (arrow) arising from the left middle turbinate, with extension to the ethmoid sinus, maxillary sinus, and floor of the orbit (Adapted with permission from Villar et al. [6])
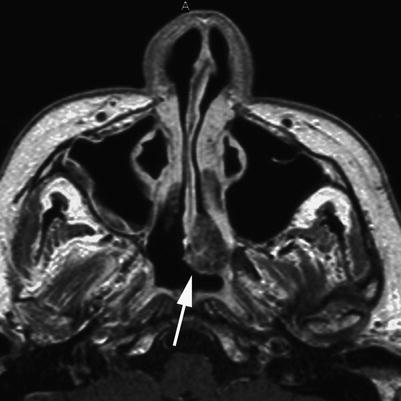
Fig. 46.2
Sinonasal adenocarcinoma. Axial MR image shows a left, intranasal low-grade adenocarcinoma (arrow) (Adapted with permission from Orvidas et al. [7])
46.3 Histopathology
ITAC, which bears a close resemblance to colon adenocarcinoma, is commonly located in the ethmoid sinus (Fig. 46.3). ITAC tumors demonstrate immunoreactivity for CK7, CK20, CDX2, and MUC [2].
Low-grade non-ITAC tumors may vary from tubular and simple glandular tumors to papillary or cystic types. Higher-grade non-ITAC neoplasms are characterized by necrosis, cellular pleomorphism, and a high mitotic rate [2].
Adenoid cystic carcinoma is often characterized by basaloid cells with small, hyperchromatic nuclei, and scant cytoplasm arranged into three subtypes: cribriform, tubular, and solid. Perineural invasion is seen in up to 70 % of these tumors. They classically have a “Swiss cheese” or sieve-like pattern. Immunoreactivity for c-kit is often positive [10, 11].
Fig. 46.3
Adenocarcinomas of the nasal and paranasal cavities are divided into two main categories: intestinal-type adenocarcinoma (ITAC) and non-ITAC. (a) In this example of a low-grade, non-ITAC sinonasal carcinoma, the tumor cells are arranged in lobules and show a moderate degree of pleomorphism and mitotic activity. (b) A tumor from the sphenoethmoidal recess shows moderately differentiated ITAC
46.4 Clinical and Surgical Management
Maximal safe tumor resection followed by adjuvant radiation and possibly chemotherapy is the mainstay of treatment.
Endoscopic endonasal resection is now widely and effectively used to treat this and other sinonasal malignancies [1].
Sinonasal adenoid cystic carcinomas have a notoriously high recurrence rate, over 90 % [4].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








