Examining a Smear
Optimal examination of an intraoperative smear entails observing at every level. Radiology, gross examination, and how the tissue physically separates are all relevant. The data that establish the final diagnosis should “fit” or be consistent at all levels. A dural-based, uniformly enhancing mass that is firm and gritty when you crush and smear it should not look like a glioma. The more raw information you have, the more accurate your diagnosis will be. Do not be persuaded by the interpretations of others; look at the scans and tissue yourself.
Examination of the smear itself is also a multilevel process. After it is stained, hold it up to the light. What does it look like? Is it pink or blue, lumpy or smooth? Does the slide have no tissue or a big clump at one end? These are all keys to the underlying nature of the lesion. Under the microscope at an intermediate magnification, the lesion’s matrix becomes clear: glial, liquid, epithelial, or cohesive. Finally, at high power, the cells reveal their identity. Their cytoplasm generally indicates the cell type, whereas their nuclei tell whether the process is reactive or neoplastic, benign or malignant.
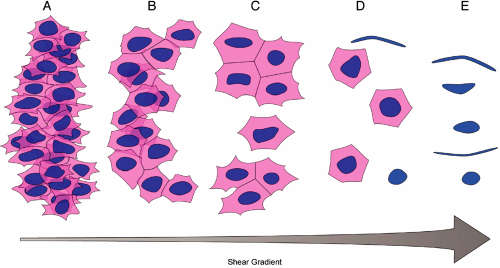
The most informative areas of a smear are at the borders of smaller tissue fragments, where the physical forces pull the cells to their limits, before they are stripped of their cytoplasm or sheared from their neighboring cells (Figure 3-1). Every tissue and every tumor has a threshold at which its cells rip apart to individual entities. It is just before this limit is reached that the smear is most informative. At this point, the shearing forces just balance the tissue’s intrinsic intercellular connections. Observing how they break gives the most biological information. Each sample will have a different threshold. You can get a sense of this limit when you observe and feel the smear as you perform it.
Smears prepared from lesional tissue generally fall into one of several classes of patterns. Cells in the lesion may be discohesive, thus smearing almost like a liquid. The lesion may have abundant glial fibers binding it together. Frequently, biopsies from tumors have an epithelial character, in which cells show a clear affinity for each other and have sharp cell borders. Some tumors grow in or elaborate dense connective tissue or a reticulin-rich background. Because of their dense extracellular matrices, their cells bind tightly together and smear poorly. Finally, the brain biopsies may be either normal brain or completely necrotic. All of these patterns are important to recognize.
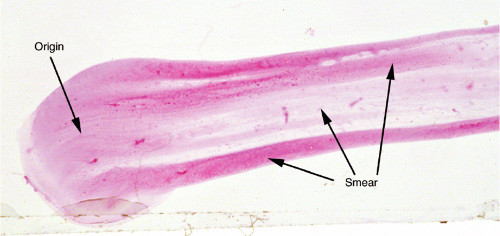
Normal Brain
Brain biopsies, especially stereotactic biopsies or large resections, frequently include normal brain. This tissue is important to recognize: in a stereotactic biopsy, misidentifying normal brain as “diagnostic” (i.e., you think it is pathologic) means the procedure will eventually have to be repeated. The key to normal brain is that it gives a smooth, pink smear (Figure 3-2). Placing the slide on a white piece of paper can almost make the diagnosis. Under the microscope, normal brain has sparse cellularity, minimal cellular clustering, and an occasional capillary.
Biopsies of gray matter come from cerebral cortex or from needle biopsies of deep nuclei (thalamus and basal ganglia). When normal, these areas produce smooth, relatively pink smears. They are hypocellular, which distinguishes them from tumors and inflammatory disorders. A few delicate capillaries often stretch around the smear, whereas larger vessels are dragged off to the end of the slide. Neurons and their synapses make up the essence of gray matter. The multitude of axons synapsing on dendrites gives gray matter or “neuropil” its fine granularity. Smearing neuropil breaks these lipid-enclosed
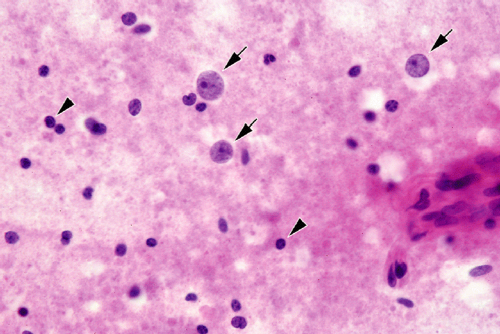
structures into fine droplets of lipids and proteins, which give gray matter its background of subtle, delicate fluffiness (see the background in Figure 3-3).
structures into fine droplets of lipids and proteins, which give gray matter its background of subtle, delicate fluffiness (see the background in Figure 3-3).
Because they arise from gray matter, neurons are present. However, usually you will not know the biopsy is of gray matter; instead you will see odd cells with large nuclei having a prominent nucleolus (Figure 3-3). Such nuclei flag gray matter. Several factors are important in distinguishing these cells from similar but nasty invaders. The nuclear envelopes of neurons should be smooth, not convoluted or irregular. They should have fine, not coarse or clumped, chromatin. If their delicate cytoplasm has not been sheared
off, you may see pyramidal shapes, Nissl substance, or lipofuscin. Finally, identifiable large neurons only make up a small percentage of cells in gray matter; most of the other inhabitants are small and nondescript. Do not mistake neurons for metastatic carcinoma or melanoma. These cells are nasty in appearance, have coarse chromatin, irregular nuclear borders, and, importantly, make up most of the cells in the region.
off, you may see pyramidal shapes, Nissl substance, or lipofuscin. Finally, identifiable large neurons only make up a small percentage of cells in gray matter; most of the other inhabitants are small and nondescript. Do not mistake neurons for metastatic carcinoma or melanoma. These cells are nasty in appearance, have coarse chromatin, irregular nuclear borders, and, importantly, make up most of the cells in the region.
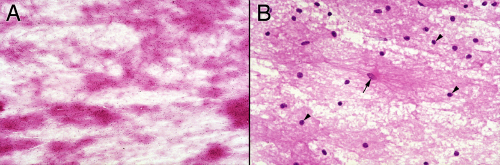
Normal white matter lacks the neurons and neuropil of gray matter. It contains two main populations of cells that can be difficult to distinguish: oligodendrocytes and astrocytes. “Normal” white matter is rare in biopsies because it will show some gliosis near lesions; also, in adults, it suffers the slings and arrows of aging (Figure 3-4). Like gray matter, nonlesional white matter is hypocellular and produces a relatively smooth smear. Typically, two types of nuclei are present: a dense, small, round, blue nucleus and a larger, slightly round nucleus with more open chromatin. The former are presumably oligodendrocytes or perhaps a rare lymphocyte, whereas the latter are most likely astrocytes. Unless you see some defining cytoplasm, you cannot reliably distinguish these nuclei. Rather, you identify a cell by the company it keeps, by its context in the surrounding tissue. It is this heterogeneity of small, white matter cells that distinguishes it from the larger, more uniform nuclei of neoplasia.
A major site of confusion in both smears and frozen sections is the cerebellum. Cerebellar cortex has a few, very large Purkinje neurons lying on top of a sea of small blue granular neurons (Figure 3-5A). A biopsy of cerebellum near a lesion will look like a small round blue cell tumor, such as a medulloblastoma, small cell carcinoma, or a lymphoma. Such biopsies will be blue and densely cellular. Two problems can occur: mistakenly calling a lesion a tumor when it is only normal cerebellum or indicating diagnostic tissue is present when the biopsy was only near the lesion. Distinguishing normal cerebellum from a small, round, blue cell tumor can be tricky. However, normal cerebellum smears evenly, like all other brain, and the confounding internal granular neurons are oppressively monotonous at high power. In a smear, identifying cerebellar cortex requires recognizing the monotony of its granular neurons (e.g., small nuclear diameter




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree