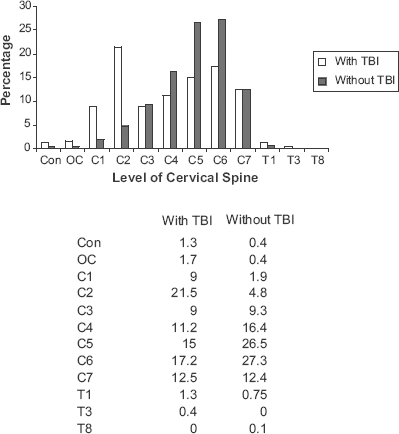
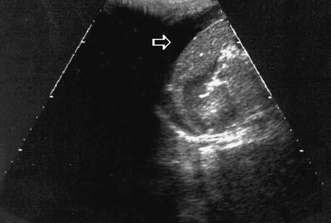
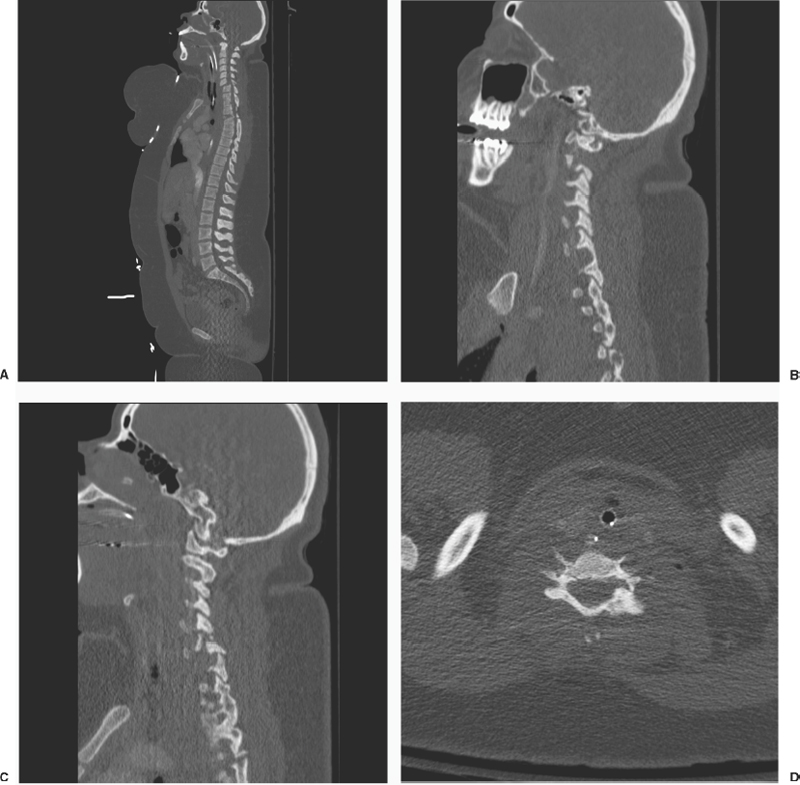
15 Special Considerations in the Evaluation of Patients with Combined Head and Spinal Injuries and Multiple System Trauma Bizhan Aarabi, Christopher J. Neal, and Allan Philp From 2% to 6% of patients admitted to a trauma center with altered state of consciousness, including traumatic brain injury (TBI), may have associated cervical spine injury.1,2–8 In a retrospective study by Chiu et al, 143 of 2605 patients (5.5%) admitted to a level I trauma center with a Glasgow Coma Scale (GCS) score less than 15 had cervical spine injury. Among this group of patients 129 had fractures and 14 pure ligamentous damage.9 In another study by Cooper et al, the incidence of thoracic, lumbar, and sacral injury for 4142 patients arriving at a level I trauma center was 4.4%. In this study patients with a GCS score of 13 to 14 had significantly less chance of complaining from back pain or tenderness as compared with patients with a GCS score of 15.10 Without vigilance, high index of suspicion, and appropriate and timely imaging studies, these fracture subluxations could be easily missed adding to further loss of function. Note that missed diagnosis is usually due to lack of adequate studies not visualizing appropriate areas of the spine or wrong interpretation of the existing imaging studies by less familiar providers. Describing 32,117 trauma patients, Davis et al discovered 34 cases of missed cervical spine injuries in symptomatic patients. Twenty-three of these symptomatic patients either did not have radiographs or had inadequate radiographs. Eight patients had imaging studies that were misread by the treating provider. Only one case was truly missed with adequate films with an undetectable fracture. The reasons for missing two fractures were not mentioned.11–13 With today’s powerful imaging technology, it is unusual to miss spinal injuries.14–20 Careful attention to demographics and mechanism of injury is crucial in pinpointing high-risk patients. Hanson et al estimated an incidence of cervical spine injury in patients without risk factors to be only 0.2%.21 Risk factors in a series of 3684 patients with injury included high-speed motor vehicle accidents (>35 miles/hour), death at the scene, fall from at least a 10-foot height, severe head injury, neurological deficit referable to the spinal cord, and multiple long bone and pelvic fractures. Reporting on 215 patients with gunshot wounds to the head, Kaups and Davis did not find a single case of indirect cervical spine injury.22 Patton et al reported the results of imaging studies of 102 patients with TBI due to assault. These authors did not find any injuries to the cervical spine using different imaging technologies, including three views, computed tomography (CT), and magnetic resonance imaging (MRI).23 Patients with TBI are at greater risk of upper cervical spine injury.24,25 The distribution of osseous or ligamentous injuries in patients with and without TBI admitted to the R Adams Cowley Shock Trauma Center from 2000 to 2005 is depicted in Figure 15-1. Clearly, patients with TBI have two peaks, with C2 at the greatest risk for fracture subluxations. Although not as sensitive as imaging studies, any of the following clinical findings in a trauma victim with depressed level of consciousness due to TBI or drugs should raise one’s index of suspicion for the presence of spinal cord injury26: The principles that govern initial injury management are the same regardless of patient specifics. These principles have been enumerated in the American College of Surgeons Advanced Trauma Life Support Course (ATLS).27,28 In the primary survey, immediately life-threatening injuries are identified and treated. Patients with neurological injury, be it TBI or spinal cord injury, can present some special challenges. Patients with TBI have a depressed level of consciousness; therefore, a history is unobtainable. More importantly, patients with brain injury are unable to voice specific complaints. Patients with spinal cord injuries, particularly if located in the cervical spine, may also be unable to fully describe their complaints if injuries are located below the level of their spinal injury. Figure 15-1 Percentage involvement of C1-T1 vertebrae in patients with cervical spine injury and neurological deficit admitted to R Adams Cowley Shock Trauma Center from 2000 to 2005. Patients with traumatic brain injury (TBI) had a higher tendency of C1-C2 involvement compared with patients without TBI. Airway control is the highest priority following injury. Patients who present with any signs or symptoms of airway compromise should be promptly intubated. Patients with TBI are at great risk for developing either or both hypoxia and hypercarbia from their depressed mental status.29,30 Patients with TBI are also at high risk for aspiration. Therefore, any patients with significant obtundation should be intubated at the time of presentation. Patients with cervical spine injury should also be evaluated for early airway control, particularly if the spinal cord level is above the fifth cervical vertebra.31 Ninety-five percent of patients with high spinal cord injury require intubation within the first 24 hours of hospitalization. Breathing, the second-highest priority, requires identification of immediately life-threatening thoracic injuries. Patients with TBI or spinal cord injury are certainly at risk for developing any of the common life-threatening thoracic injuries such as tension pneumothorax, massive hemothorax, cardiac tamponade, open pneumothorax, or a flail chest. Following airway control, a rapid search should be made for these conditions and they should be treated if present. Assessing the adequacy of circulation and treating hemorrhage are the next highest priorities. A rapid search of hemorrhage should identify the location of bleeding. In addition to external bleeding, there are four body cavities into which a patient can lose significant amounts of blood: the abdomen, thorax, muscle compartments, pelvis, and outside the torso. The combination of physical exam and initial radiographic studies should suffice. Hemorrhage control and rapid resuscitation are particularly important in patients with TBI because hypotension has been shown to markedly worsen outcome by producing secondary brain injury.29,30 Patients with cervical spinal cord injury may be hypotensive from neurogenic shock, hemorrhagic shock, or a combination of both. Because patients with brain injuries or spinal cord injuries may not be able to describe symptoms of all injuries, physical exam becomes very important in identifying areas of injury. Particular attention must be paid to outward signs of injury such as a seat belt sign or areas of contusions or lacerations. Extremity bleeding or edema should prompt a search for underlying injury. The torso should be examined for differences in breath sound and for subcutaneous air. Extremity pulses must be evaluated, with an eye toward inconsistencies and imbalances. Careful and thorough physical examination remains essential. However, a greater dependence on diagnostic imaging is necessary in patients with neurological injury. Patients with neurological injury are often multiply injured.32 Evaluation and treatment must proceed simultaneously. A full evaluation may not be possible until the patient is stabilized. Even urgent studies such as head CT may have to be deferred until after a laparotomy or thoracotomy is performed for hemorrhage control. These patients are among the most dynamic patients. Decision making must be fluid and will often require input from various services to obtain optimal patient care. A few basic radiographs may be considered an extension of the secondary survey. Many large institutions now deviate slightly from the ATLS guidelines and perform only a supine chest film, an anteroposterior (AP) pelvis film, and a focused abdominal sonogram for trauma (FAST) for this exam (Fig. 15-2).33 The goal acutely is to efficiently localize potentially life-threatening conditions. On the chest film, these include smaller pneumo- or hemothoraces (larger collections or tension conditions should be appreciated on auscultation), which are demonstrated by a pleural line, “deep sulcus” sign, or increased opacity of a hemithorax, respectively. Other injuries, including diaphragmatic rupture, pneumomediastinum, or pneumopericardium, may also be suggested by a simple chest x-ray. The pelvic film serves to show fractures of the pelvic ring, acetabulae, or proximal femurs, as well as femoral head dislocations. Pelvic fractures in particular should raise the suspicion for both a hemodynamically threatening source of hemorrhage and the potential of commonly associated bladder and urethral injuries. Figure 15-2 Focused abdominal sonogram for trauma, showing fluid between the liver and kidney (arrow). This patient presented following a motor vehicle collision and required embolization for hepatic hemorrhage control. The FAST is performed to characterize primarily the pericardium and peritoneum. A modest amount of training allows even nonsurgical practitioners to detect significant hemopericardium and hemoperitoneum, using a series of four standard views of the heart, left and right upper quadrants, and pelvis (see Fig. 15-2). This exam is dependable, rapid, painless, and easily repeated at intervals if necessary. It is less sensitive for intraparenchymal solid organ injury in the absence of hemoperitoneum, but these injuries less commonly require surgical or angiographic intervention. Unfortunately, sonography is also significantly limited in its ability to demonstrate hollow viscus injury or retroperitoneal structures. CT scanning, discussed subsequently, more completely defines these areas.34,35 We recently acquired a Statscan Critical Imaging System (Lodox Systems (Pty), Ltd., Benmore, South Africa). The Statscan is a low-dose digital radiograph that scans the entire body in ~13 seconds. We routinely scan the patient in both AP and lateral projections. The oblique projections can be obtained if desired. The images are reformatted and available for review within our digital radiographic system36 (Fig. 15-3). There are some obvious advantages with the Statscan in patients who are obtunded. Long-bone fractures can be identified regardless of lack of symptomatology. The mid- and lower thoracic spine as well as the lumbar spine can be imaged quite nicely. The quality of the images of the cervical spine is normally not clear enough to clear the spine down to the level of T1. In addition, because it is an AP projection, the mediastinum is virtually never cleared. We routinely use screening CT to evaluate these areas as well as the abdomen. Figure 15-3 Lodox total body imaging in a patient with multiple contusions and complaints of pain after a fall but ultimately without fractures. CT scan is now routinely used to image the bony structures of the neck as well as the soft tissue and vascular structures. High-resolution CT can diagnose a laryngeal and tracheal injury, or panendoscopy may be employed to study the aerodigestive tract. Hemorrhage, edema, or air adjacent to the esophagus strongly suggests esophageal injury.32 The incidence of blunt cerebrovascular injuries is an evolving area, and the ready access to high-resolution CT and CT angiography (CTA) suggests the incidence may be in the 1% to 3% range, with a mortality of 10% to 40%. These are manyfold higher than data a decade ago would suggest.37,38 In our center, therefore, patients undergoing a contrasted initial trauma CT receive neck imaging and a formal CTA if this is suggestive of injury. An alternative employed at some facilities is magnetic resonance angiography (MRA)39; however, this is somewhat more time consuming, not as readily accessible, and thus not as frequently employed in the acute setting. A significant amount of intrathoracic pathology may be clarified by CT scanning with intravenous (IV) contrast. This allows excellent imaging of the mediastinal structures, particularly the great vessels, as well as the trachea and lungs. It may also suggest esophageal injury (air in the posterior mediastinum), although it is less sensitive for hollow viscus injuries. Conditions not as visible on plain films, such as pulmonary contusions and lacerations, smaller pneumo- or hemothoraces, or foreign bodies, are much more easily seen on CT imaging. A particularly concerning injury, traumatic aortic disruption, is also well seen on contrast chest CT. Many institutions employ multichannel scanners that can produce reconstructed images providing information as detailed as a conventional angiogram, and in these locations CTA has replaced angiography for aortic injury diagnosis and planning of subsequent management40,41 (Fig. 15-4). Although the speed and ease of obtaining a FAST exam and a plain pelvis film make them very useful in acutely evaluating traumatic abdominal and pelvic injuries, they lack the sensitivity and specificity of CT scanning for intraparenchymal solid organ damage (liver and spleen), hollow viscus trauma (stomach, small bowel, and colon), and extraperitoneal structures (kidney, pancreas, bony pelvis, etc.). Again, multichannel scanners with carefully formulated protocols allow imaging of the chest, abdomen, and pelvis as a contiguous unit with great success and a single-contrast bolus. This provides information about contrast extravasation, grading solid organ injuries, and quantifying hemoperitoneum. Reconstructions may also be performed for acetabular and pelvic fractures or complex vascular injuries. In turn, this allows appropriate decision making regarding nonoperative, angiographic, or operative management of these injuries.42,43 Figure 15-4 Chest computed tomography with active bleeding in the left thorax (arrow) following a motorcycle accident. The patient continued to bleed after evacuation with a chest tube and went to thoracotomy for control of intercostal and lung hemorrhage. A weakness of CT scanning continues to be the diagnosis of hollow viscus and diaphragmatic injuries. Although the sensitivity for bowel injury increases if signs other than frank intraperitoneal air or contrast leak are utilized (bowel wall thickening or discontinuity, free fluid in the absence of solid organ injury, mesenteric thickening/hematoma), it still remains less than 90% in most series and considerably worse in some. If suspicions are significant, deep peritoneal lavage, laparoscopy, or laparotomy is indicated.44,45 Similarly, even the highest-resolution CT or MRI has up to a 25% false-negative rate for diaphragmatic injuries. If suspected, laparoscopy or laparotomy is a consideration for further evaluation.46,47 In stable patients, this can be pursued in a controlled fashion after more-threatening conditions have been addressed. The genitourinary system may also require evaluation, particularly in the setting of pelvic fractures. CT imaging accurately diagnoses renal contusions and lacerations, and simultaneous CT intravenous pyelogram (IVP) is typically adequate for ureteral injury screening. CT cystogram is also possible, although the protocols are not available at every institution48 (Fig. 15-5). In those instances, a simple three-view bedside cryptogram (scout film, view with 300 mL of contrast instilled into the bladder, and postdrainage film)28 is usually adequate to elucidate intra- and extraperitoneal bladder rupture. If questions exist regarding urethral integrity, a similar bedside urethrogram may be obtained by instilling contrast into the urethral meatus with an angiocath and using AP and oblique plain films to demonstrate extravasation. Figure 15-5 Computed tomographic cystogram with extraperitoneal bladder rupture (arrow) in a patient with a pelvic fracture and hematuria. This was managed with Foley catheter drainage for 10 days and then repeat cystogram. Physical exam should demonstrate most long-bone injuries, even in obtunded patients. More subtle fractures, however, may be difficult to discern. Accordingly, any areas with deformity, pain on exam, or stigmata of trauma (contusion, abrasion, or swelling) should be imaged in at least two views with plain films. Any known injury should also include films of the joints and regions above and below the fracture. A screening Statscan (see Fig. 15-3) will provide total body AP and lateral views of the torso as well as information about long bones and some smaller bony structures. The Statscan may miss distal fractures in the extremities. Finally, any fracture or dislocation should prompt a careful neurovascular exam. Diminution of pulses on exam or asymmetric pulses should prompt further workup with angiogram or CTA given the high association of vascular injury requiring repair. CT requires the administration of intravenous contrast, which raises several potential concerns. The occurrence of true IV contrast allergies is relatively uncommon. Intravenous steroids (100 mg methylprednisolone), IV diphenhydramine chloride, and an IV histamine-2 (H2) blocker are typically adequate to prevent reactions other than anaphylaxis. An alternative such as MRI/MRA might be considered. A longer course of premedication with multiple steroid doses if time permits can be used for prophylaxis.49 The second concern with IV contrast is renal injury. This also appears to be less frequent than initially believed, and several recent studies have supported its use even in renal insufficiency. As with most cases, the maintenance of renal perfusion with adequate hydration and blood flow is essential to preventing an injury.50,51 Pregnancy is another condition worthy of particular consideration. Because the fetal mortality is markedly increased by maternal shock, the trauma workup should not be delayed, and necessary radiographic studies should be performed. All women of greater than 20 weeks’ gestation should have fetal monitoring, and all greater than 12 weeks a Kleihauer-Betke analysis. Exposure of less than 5 rads has no clear association with increased fetal anomalies or fetal demise and so is safe at all stages. (Fetal dosing is roughly 30% of maternal exposure if unshielded.) Thus, if essential studies are selected most trauma workup can be safely obtained. The fetus must be shielded during x-ray imaging outside the pelvis, and ultrasound used in place of other studies if available. MRI is also not associated with known adverse fetal effects, but until more information is available it is not recommended during the first trimester.52 The initial evaluation of blunt trauma remains challenging due to the breadth of potential injuries and involved structures. This is particularly true in the population involving central nervous system (CNS) injuries in whom physical exam is less reliable, and thus thoughtful diagnostic imaging is essential. An initial survey with chest x-ray, pelvis film, and FAST identifies most immediately life-threatening extra-CNS injuries. CT scanning with IV contrast and including images of the neck, thorax, abdomen, and pelvis identifies the vast majority of other critical conditions. At our institution, a large tertiary care center, patients undergo an initial evaluation with plain films and ultrasonography as noted, followed by a “trauma protocol” scan, which includes a noncontrasted head CT and contrasted neck, chest, and abdomen/pelvis utilizing a single-contrast bolus. More specific evaluation with formal CTA is undertaken to further characterize lesions if necessary. Major extremity injuries should be detected initially on physical exam, with plain films targeted for fractures or a screening Statscan exam, and consideration of CTA or formal angiography for vascular abnormalities. In 2002, based on the available scientific evidence, “Guidelines for the Management of Acute Cervical Spine and Spinal Cord Injuries”53 offered recommendations for two management questions: (1) the most sensitive, specific, and safe protocol to rule out stable and unstable cervical spine bony and ligamentous injuries in symptomatic patients, including patients with altered mental status and TBI; and (2) the most reliable and secure manner to discontinue cervical spine immobilization in symptomatic patients (including TBI patients) when static radiographic studies are nonrevealing. A three-view cervical spine series (AP, lateral, and odontoid views) is recommended for radiographic evaluation of the cervical spine in patients who are symptomatic after traumatic injury. This should be supplemented with CT to further define areas that are suspicious or not well visualized on the plain x-rays. Cervical spine immobilization in obtunded patients with normal cervical spine x-rays (including supplemental CT as necessary) may be discontinued (1) after dynamic flexion/extension studies performed under fluoroscopy guidance, or (2) after a normal MRI study is obtained within 48 hours of injury, or (3) at the discretion of the treating physician. Research supporting the standards for radiographic evaluation of a patient with altered mental status following TBI remains robust. It has been firmly established that a complete three-view cervical spine series is very informative in discovering cervical spine injuries following blunt trauma. The negative predictive value for a complete three-view cervical spine series has been recorded to be from 85% to 98%.14,15,54–57 The sensitivity, however, remains low, from 62.5% to 84%.14,15,20 In a retrospective review of 775 motor vehicle crash victims by MacDonald et al, 55% had a GCS <15. Lateral radiographic visualization of the complete cervical spine had a sensitivity of 83% and a specificity of 97%.20 In a prospective study by Berne et al, 58 patients with blunt trauma and multiple organ injury had a mean GCS score of 8.9. Twenty of these patients (30%) had cervical spine injuries (12 stable and eight unstable). Plain radiography missed eight injuries (including three unstable injuries), and its sensitivity was 60% and negative predictive value 85%.15 Plain radiography had a specificity of 100% and a positive predictive value of 100%. Ajani et al, in a class I study, evaluated cervical spine injuries in 100 critically ill patients. They used static and functional radiographs, CT, MRI, and clinical follow-ups. Complete radiography missed one of six unstable fractures, a sensitivity of 84%.14 Evaluation of not well-visualized and questionable areas by CT increases sensitivity significantly.14–16,20,54,58,59 In Berne et al’s study, CT missed two injuries, both clinically insignificant. In this study the negative predictive value for CT was 95% for all injuries and 100% for unstable spine fractures.15 CT is specifically valuable for craniocervical and cervicothoracic junctions.18,58,60 In 100 patients with blunt injury and poor visualization of the C7-T1 region, Tehranzadeh et al found three stable fractures of C6 and C7 vertebrae using supplemental CT for definitive evaluation.59 Evaluating the cost-effectiveness of CT, Tan et al studied 360 patients with poor visualization of the C7-T1 region on plain radiography and discovered 11 missed fractures.58 The applicability of MRI in the acute settings of emergency departments (EDs) and intensive care units (ICUs) to rule out osseoligamentous spine injuries is not well defined. When done within 48 hours of injury and negative, MRI is helpful, but many of the more than 30% soft-tissue findings seen on T2-weighted images may be clinically insignificant.61,62 In Benzel et al’s study, only one of 62 patients with discoligamentous injuries in a series of 174 patients with blunt trauma and without clinical or radiographic evidence of disruption of spinal integrity needed surgical fusion.61 D’Alise et al studied 121 high-risk, intubated, obtunded/comatose patients with nonrevealing cervical spine radiographs. These investigators discovered 31 patients (25.6%) with disk, ligamentous, or bony cervical spine injuries. Eight of these 31 patients needed surgical intervention. Ninety of 121 patients were considered to have no cervical spine injuries and were thus cleared. MRI is not particularly helpful in cervical spine fractures. Klein et al studied 32 patients with 75 known fractures. The sensitivity of MRI to detect posterior and anterior spinal fractures was 11.5% and 36.7%, respectively. Negative predictive value in this group of patients was 46% and 64%, respectively.63 Immobilization of the cervical spine, in light of normal radiographs and supplemental CT, is allowed only after dynamic flexion/extension radiographs of the cervical spine or a normal-looking MRI within the first 48 hours after trauma.53 In 372 patients with blunt trauma and normal cervical spine radiographic studies, Brady et al discovered five new abnormalities, none of which needed surgical management and some of which could have been false-positive.65 In a class I study of 100 obtunded patients, Ajani et al. discovered one unstable cervical spine injury with dynamic flexion/extension fluoroscopy in a patient with a normal three-view series and CT of the cervical spine.14 Davis et al reported on questionably unstable subluxations using dynamic fluoroscopy in 116 obtunded patients with normal three-view series and CT scan.17 Bolinger et al were less impressed by the quality of images of bedside fluoroscopic flexion and extension views in 56 consecutive comatose head-injured patients.64 These authors discovered one new unstable type 2 odontoid fracture. A combination of normal three-views of cervical spine and dynamic flexion/extension radiographs improve the negative predictive value of cervical spine radiographic studies for significant osteoligamentous injuries up to 99%.14,17,19,65 The negative predictive value of MRI within the first 48 hours is very high; however, MRI of the cervical spine is weak in revealing posterior arch fractures, and positive soft-tissue findings are less interpretable.61–63,66
Demographics and Mechanism of Injury
Evaluation of the Multisystem Trauma Patient, Including Traumatic Brain Injury
Initial Imaging for Blunt Trauma

Evaluating Organ Systems
Soft Tissues and the Neck
Thoracic Injuries
Abdominal and Pelvic Injuries


Extremity Injuries
Special Considerations
Summary
Radiographic Assessment of the Spine in Traumatic Brain Injury Patients
Standards
Options
Deviations from the Guidelines
Special Considerations in the Evaluation of Patients with Combined Head and Spinal Injuries and Multiple System Trauma
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








