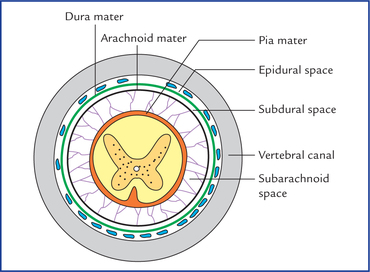
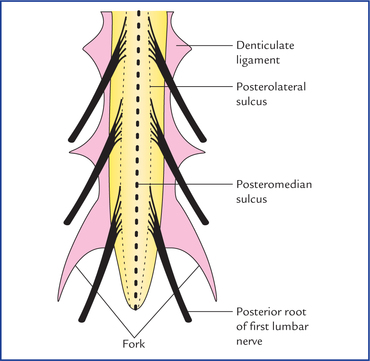
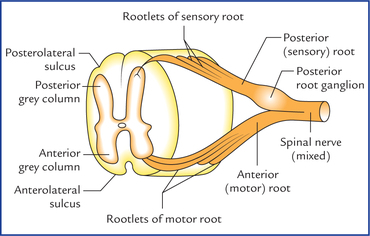
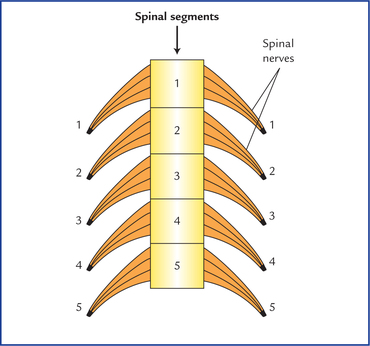
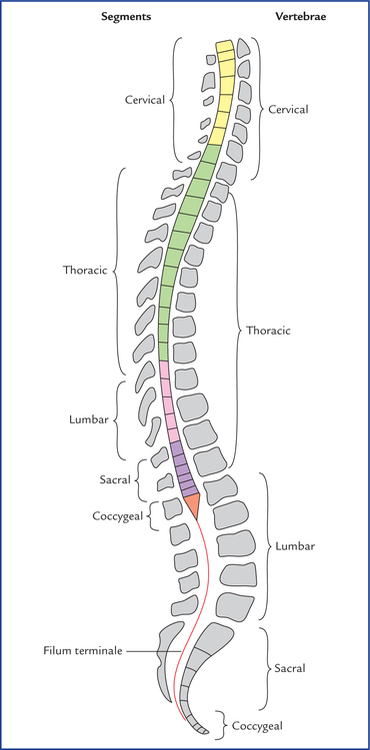
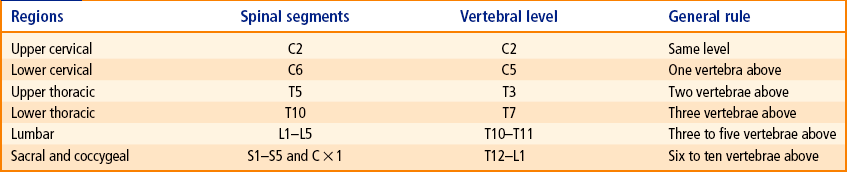
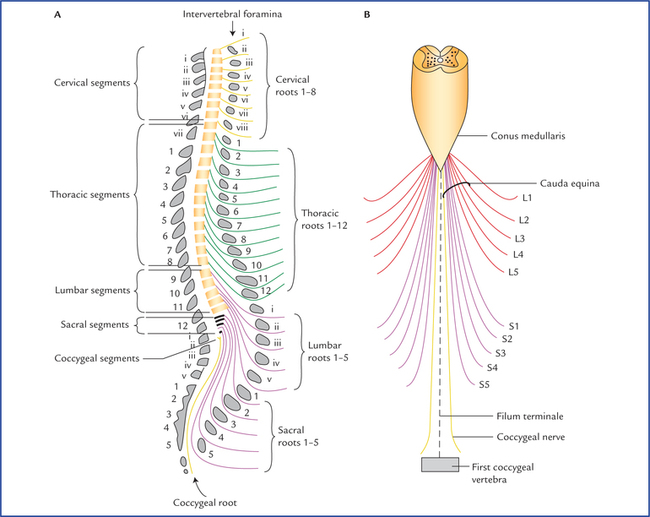
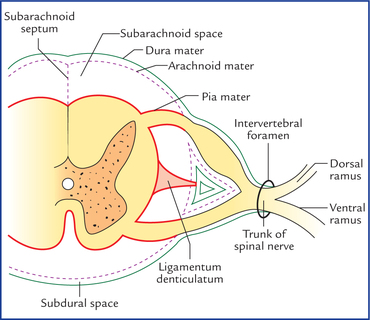
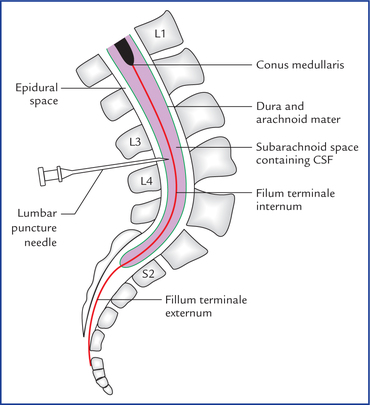
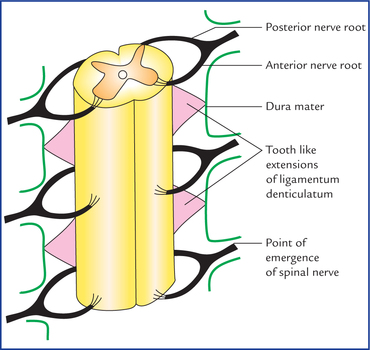
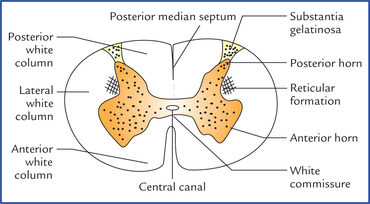
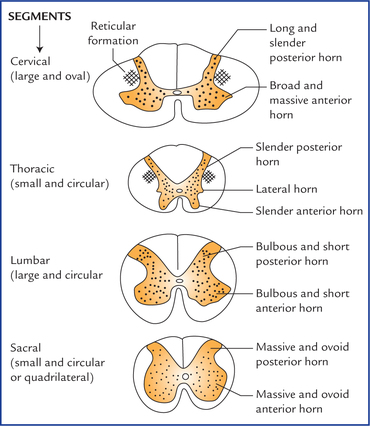
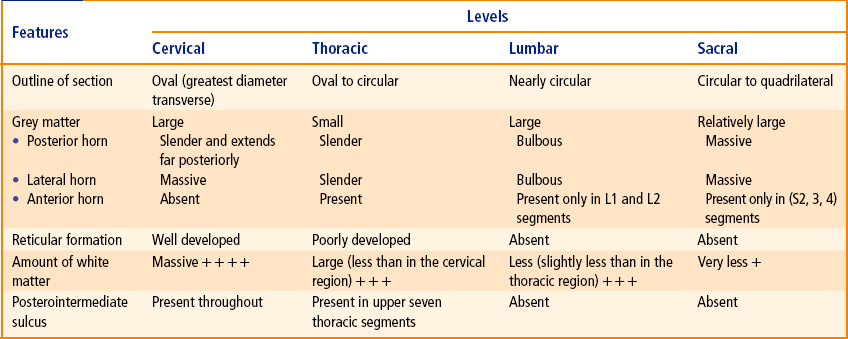
7 The spinal cord is the lower elongated part of the central nervous system (CNS). It is cylindrical in shape, slightly flattened anteroposteriorly and occupies the upper two-third of the vertebral canal. The spinal cord is surrounded by three protective membranes called spinal meninges. From outside inwards these are: dura mater, arachnoid mater, and pia mater (Figs 7.1 and 7.2). Fig. 7.2 Schematic transverse section of spinal cord showing meninges and formation of meningeal sheaths onto the spinal nerve roots. The spinal dura extends from foramen magnum to the lower border of second sacral vertebra (S2). The space between dura and arachnoid mater termed subdural space. It contains capillary layer of fluid. The spinal dura differs from cranial dura. The differences between the two are enumerated in Table 7.1. Table 7.1 Differences between spinal and cranial dura The subarachnoid space between the pia mater and the arachnoid mater is filled with cerebrospinal fluid (CSF). Above it is continuous with subarachnoid space around the brain. Distal to the termination of spinal cord, the sub-arachnoid space around the filum terminale, becomes roomy, forming a pool of CSF called lumbar cistern. The lumbar puncture is done at this site to take out the CSF (Fig. 7.3). Fig. 7.3 Sagittal section through lumbosacral region showing conus medullaris, filum terminale (internum and externum), lower end of subarachnoid space and site of lumbar puncture. The central canal of spinal cord extends into the upper part of the filum terminale for about 5 mm. The filum terminale consists of two parts: (a) filum terminale internum, and (b) filum terminale externum. The filum terminale internum is about 15 cm in length and lies within the dural sac. The filum terminale externum is about 5 cm in length and lies outside the dural sac, i. e. below the level of second sacral vertebra (Fig. 7.3). These are two transparent ribbon-like thickened bands of pia mater (one on each side) extending laterally between posterior and anterior nerve roots from pia mater covering the cord. The lateral margin of each band presents 21 tooth-like processes which pierce the arachnoid, to be attached to the inner surface of the dura mater between the points of emergence of the spinal nerves (Fig. 7.4). Fig. 7.4 Anterior view of part of spinal cord, showing position of ligamenta denticulata and their attachments to the dura mater. The ligamenta denticulata help to anchor the spinal cord in the middle of subarachnoid space. The external features of the spinal cord are (Fig. 7.6): Fig. 7.6 External features of the spinal cord: (A) on anterior aspect, and (B) on posterior aspect. Also note the important levels (C1, L1, S2, etc.) in relation to the spinal cord. The anterior aspect of the spinal cord (Fig. 7.6A) presents anterior median fissure, and two anterolateral sulci while the posterior aspect (Fig. 7.6B) presents: posteromedian sul-cus, two posterolateral and two posterointermediate sulci. The surface of the cord is divided into two symmetrical halves by an anterior median fissure and a posterior median sulcus. Thirty-one pairs of spinal nerves emerge from the sides of the cord. Of these, 8 are cervical, 12 are thoracic, 5 are lumbar, 5 are sacral, and 1 is coccygeal. The cervical nerves leave the vertebral canal above the corresponding vertebrae with the exception of eighth, which emerges between seventh cervical and first thoracic vertebrae. The remainder spinal nerves emerge below the corresponding vertebrae. Each spinal nerve is attached to the cord by two roots, anterior motor root and posterior sensory root. The posterior root has a ganglion, the posterior root ganglion consisting of pseudounipolar cells. Each of the two roots is made up of number of rootlets that arise from the spinal cord over a certain length (Fig. 7.7). The rootlets of posterior root enter the dorsolateral aspect of the cord along the posterolateral sulcus whereas the rootlets of anterior root emerge from the anterolateral sulcus/anterolateral aspect of cord opposite to the anterior grey column. Like the vertebral column, the spinal cord is also segmented though the segments are not visible externally. The part of spinal cord to which a pair of spinal nerves (right and left) is attached is known as spinal segment (Fig. 7.8). The number of spinal segments corresponds to the number of vertebrae in thoracic, lumbar and sacral regions, but in cervical region, one segment is more than the number of vertebrae, whereas in coccygeal region there is only one segment for four coccygeal vertebrae. Thus, the spinal cord is made up of 31 spinal segments: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and one coccy-geal. Since, the length of spinal cord (45 cm) is smaller than the length of vertebral column (65 cm), the spinal segments are, short and crowded, especially in the lower part of the cord. Thus, the spinal and vertebral segments (spines) do not lie at the same level. The spinal segments as a rule always lie above their numerically corresponding vertebral spines. In the lower part of the spinal cord, they lie well above their corresponding vertebrae (Fig. 7.9). For example, the lumbar segments are related to the thoracic vertebrae. Approximate vertebral levels matched to spinal cord segments are presented in Table 7.2. The spinal cord is roughly cylindrical in shape with an average diameter of about 1.25 cm. However, opposite to the attachments of the nerve roots contributing to the formation of brachial and lumbosacral plexuses, the spinal cord presents definite fusiform swellings called cervical and lumbar enlargements respectively (Fig. 7.6A, B). The two enlargements are compared in Table 7.3. Table 7.3 Comparison between cervical and lumbar spinal enlargements Since the cord is shorter than the vertebral column, length and obliquity of spinal nerve roots increase progressively from above downwards, so that spinal nerves may emerge through their respective intervertebral foramina (Fig. 7.10A). As a result the nerve roots of lumbar, sacral and coccygeal nerves from the caudal part of the cord takes more or less a vertical course and form a bunch of nerve fibres around the filum terminale called cauda equina because of its fancied resemblance to the tail of a horse (cauda – tail; equina – horse). The cauda equina consists of the roots of the lower four pairs of lumbar, five pairs of sacral and one pair of coccygeal nerves (Fig. 7.10B). The cross-section of the spinal cord (Fig. 7.11) shows that it consists of an inner core of grey matter, and a peripheral zone of white matter. Fig. 7.11 Cross-section through the cervical segment of the spinal cord showing its internal structure. In cross-section of cord the grey matter is seen as H-shaped (or butterfly-shaped) fluted column, extending throughout the length of the spinal cord. It is divided into symmetrical right and left comma-shaped masses which are connected across the midline by a transverse grey commissure. The central canal of the cord passes through the centre of grey commissure. The canal is surrounded by substantia gelatinosa centralis. The lateral comma-shaped mass of grey matter is further divided by a transverse grey commissure into a narrow elongated posterior horn, and a broad anterior horn. In the thoracic region and upper two lumbar segments (T1 to L2), a triangular projection juts out from the side of lateral grey mass between the anterior and posterior horns, nearly opposite to the grey commissure. It is called lateral horn. The posterior horns are connected to the surface by a gelatinous substance called substantia gelatinosa. The amount of grey matter and shapes of its horns, and amount of white matter varies at different levels (Fig. 7.12). Fig. 7.12 Transverse sections of the spinal cord at different levels showing the arrangement of grey and white matters. The horns are thus largest in the regions—cervical and lumbar enlargements. 1. Progressively more and more ascending fibres are added to the cord from below upwards. 2. Number of descending fibres decreases in the cord from above downwards as some of them terminate in each spinal segment. Table 7.4 reveals the characteristic features of the spinal segments in different regions of the spinal cord. Table 7.4 Characteristic features of spinal segments as seen in transverse sections at various levels of the spinal cord Types of motor neurons in the anterior grey columns: 1. Alpha (α) neurons: They are large multipolar cells (25 µm or more in diameter) and supply the extrafusal skeletal muscle fibres. 2. Gamma (γ) neurons: They are small multipolar cells (15–25 µm in diameter) and supply the intrafusal muscle fibres of the neuromuscular spindles in skeletal muscles. • Sensory neurons: These are present in the posterior horn and involved in relay of sensory information to the different parts of the brain, forming ascending tracts; or to the other segments of spinal cord forming interseg-mental tracts. • Interneurons: These are small neurons present throughout the grey matter of the spinal cord. They connect different types of neurons, hence also called association neurons. These are either inhibitory or excitatory, and concerned with integration of segmental activities.
Spinal Cord
Spinal Meninges
Dura Mater
Spinal dura
Cranial dura
Single layered and consists of meningeal layer only
Double layered and consists of an inner meningeal layer and outer endosteal layer
Does not form folds
Forms folds, viz. falx cerebri, falx cerebelli, tentorium cerebelli and diaphragma sellae
Epidural space present
Epidural space absent
Pia Mater
Processes of the pia mater (also called special parts of the pia mater)
1 Filum terminale
4 Ligamenta denticulata
External Features of the Spinal Cord

Fissures and Sulci
Attachment of Spinal Nerves
Spinal segments
Enlargements
Cervical enlargement
Lumbar enlargement
Extent
From C5 to T1 spinal segments
From L2 to S3 spinal segments
Vertebral level
From C3 to T1 vertebrae
From T9 to L1 vertebrae
Widest circumference
About 38 mm at the level of C6 segment
About 35 mm at the level of S1 segment
Innervation
Muscles of upper limbs and their associated girdles
Muscles of the lower limbs and their associated girdles
Cauda Equina
Internal Structure of the Spinal Cord
Grey Matter
Structure of the grey matter
Neurons in the grey matter of the spinal cord
Functional classification
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree