24 Spondyloarthropathies
I. Key Points
– Spondyloarthropathies are subdivided into seronegative and seropositive arthropathies (positive vs. negative antinuclear antibody [ANA] or rheumatoid factor [RF]).
– A family of described disorders/syndromes with overlapping symptomology with varying human leukocyte antigen (HLA) associations, including ankylosing spondylitis (AS), psoriatic arthritis, enteropathic arthritis, Reiter syndrome, ossification of the posterior longitudinal ligament (OPLL), and rheumatoid arthritis (RA)
– RA with high incidence of C-spine involvement (>85%)1
– In RA, atlantoaxial subluxation (AAS) classified by anterior atlantodental interval (ADI) ≤3 mm (stable) and posterior atlantodental interval (PADI) ≤14 mm (increased risk of injury)
– OPLL: Asians, mostly asymptomatic, surgical approach controversial. Computed tomography (CT) for evaluation of posterior longitudinal ligament (PLL) calcification/ossification.
– Diffuse idiopathic skeletal hyperostosis (DISH): sacroiliac sparing, osteophytic change, associated with globus and dysphagia
II. Ankylosing Spondylitis Seronegative Arthropathy
– Background
• Also called Marie-Strümpell disease.1 Affects 0.1 to 0.2% of the population, with a male : female ratio of 3 : 1. Peak age of onset: teens to fourth decade of life.2
• A chronic systemic inflammatory disease (strongest correlation with HLA-B27). CD4, CD8, and cytokine (tumor necrosis factor [TNF]-α and -β) mediated.3–5
• AS specifically involves the sacroiliac joints and progresses to involve the entire spine. It may also variably involve peripheral joints, eyes, skin, and the cardiac and intestinal systems.
• Increased risk (up to 20%) if there is a first-degree relative with HLA-B27 and AS6
• Enthesitis: chronic inflammation at the insertion point of tendons that leads to ossification5
• Enthesopathy leads to osteoporosis of vertebral bodies and disc with sparing of nucleus pulposus (bridging osteophytes), producing the so-called bamboo spine.1
– Signs, symptoms, and physical exam1,5
• Initial nonradiating back pain and morning stiffness (>45 minutes) that improves with exercise/activity
• Stiffness of the gluteal and lumbosacral junction (sacroiliitis)
• Progression of symptoms to entire spinal axis
• Eventual decrease in range of motion (autofusion)
• Tendon/ligament involvement (plantar fasciitis/Achilles tendonitis)
• Differential diagnosis: rheumatoid arthritis (RF+), DISH (also called Forestier disease) (spares facet and sacroiliac [SI] joint, later age of onset than AS), psoriatic arthritis/Reiter syndrome (milder with asymmetric sacroiliitis)
• The Patrick or FABERE (flexion, abduction, external rotation, extension) test: flex hip, flex knee, and place the lateral malleolus on contralateral knee; then press the ipsilateral knee downward (by stressing the hip joint); will cause pain in bursitis, sacroiliitis, and other hip joint pathology
• Cauda equina syndrome: usually no obvious etiology or compression
• Unstable rotatory subluxation (occipitoatlantal or atlantoaxial joint)
• Myelopathy: due to bow stringing of cord
• Significant fractures with minimal trauma
– Workup
• Modified New York criteria (radiographic sacroiliitis and back pain >3 months, limited spine motion in sagittal/frontal planes, or limited chest expansion)
– Neuroimaging
• Plain x-rays (crucial for diagnosis): obtain x-rays of entire spine (bamboo spine) and pelvis (SI joint) (Fig. 24.1)
• Magnetic resonance imaging (MRI): for further evaluation of disc spaces and ligamentous changes
• Bone scan: increased uptake at SI joint
– Treatment
• Medical management with nonsteroidal antiinflammatory drugs (NSAIDs), sulfasalazine, TNF-α antagonists, and corticosteroids
• Stable fracture: treatment with rigid brace
• Surgical decompression for inpatients with unstable fractures and/or progressive neurologic deficit
• Special care needed with routine neck immobilization after trauma intraoperatively in patients with AS. These patients tend to have the neck fixed in flexed position. Forced inline fixation may be deleterious, so fix neck in natural position.
• If patient is placed in traction, special attention to degree of kyphosis is necessary. Traction must be in line with patient’s natural kyphosis and not directly horizontal.
• No consensus on treatment for cord injury in AS patients (halo vs internal fixation) without obvious compression
• Root/cord compression: laminectomy and fusion recommended
• Posterior approach should be strongly considered secondary to anterior bridging osteophytes and concerns with fixation of anterior plate for osteoporotic vertebral body.
• Consider posterior osteotomy and fusion for correction of severe kyphotic deformity
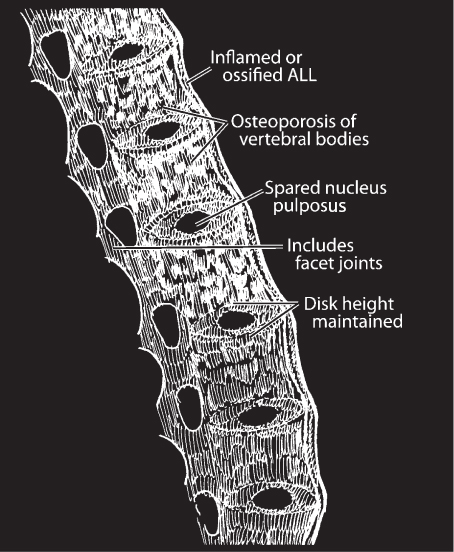
Fig. 24.1 “Bamboo spine” in ankylosing spondylitis.
III. Rheumatoid Arthritis
– Background
• Very high incidence of C-spine involvement (atlantoaxial subluxation [anterior > posterior], basilar impression, pannus granulation of odontoid)5,7
• 2 : 1 female : male ratio; peak incidence in fourth to fifth decade of life
• Serum RF+: 1 to 2% prevalence
• AAS: erosion at C1-C2 joint and at transverse ligament insertion
– Signs, symptoms, and physical exam
• Morning stiffness, symmetric multi-joint arthritis (particularly the proximal interphalangeal [PIP], metacarpophalangeal [MCP], and metatarsophalangeal [MTP]), rheumatoid nodule (extensor surface)
• Radiographic decalcification at joints (x-ray hand)
• Neck pain with possible C2 radiculopathy
• Headache, paresthesias, difficulty with ambulation, and signs of cervicomedullary junction compression (basilar impression)
– Workup
• ADI: ≤3 mm for evaluation of integrity of the transverse ligament; does not correlate with risk of injury8
• PADI: essentially the amount of space for the cord at C1-C2; does correlate with risk of injury if ≤14 mm5,8
• Look for basilar impression and cervicomedullary junction compression
– Neuroimaging
• Lateral C-spine x-ray: ADI (anterior aspect of odontoid to arch of C1) / PADI (posterior aspect of vertebral body to spinolaminar line)
• MRI for evaluation of degree of stenosis (pannus)
– Treatment
• Surgical treatment of asymptomatic AAS can be considered when ADI >6 to 10 mm.9
• AAS in RA will progress with time; therefore, treatment is recommended, especially if myelopathy exists.
• Rigid collar does not support C1-C2 and is therefore a poor option.
• Immobilization of the C1-C2 joint via halo or posterior fusion alone may reduce the size of pannus over time.
• May use halo traction to align the odontoid and return it to its neutral position (start with 5 lb).
– Surgical pearls5
• Anterior, posterior, or vertical subluxation: most cases will require 360 degrees of fusion.
• Rotational or lateral subluxation: posterior-only approach is adequate.
• Posterior fusion with or without laminectomy (C1): C1-C2 fusion, C2-occiput
• Anterior approach: odontoidectomy. For transoral approach the patient’s mouth must be able to open at least 25 mm.1 Patient is to remain in halo traction until fusion.
• RA with concomicant basilar impression should first be reduced and then fused.
• Transoral approach is associated with higher morbidity and usually reserved as a second option to posterior fusion.
IV. Diffuse Idiopathic Skeletal Hyperostosis
– Background
• Significant osteophyte formation in absence of significant degeneration. Distinct from degenerative disease, OPLL, and AS (Fig. 24.2).10
• Males in seventh decade of life
• SI joint spared11
• Osteophytes do not stabilize, and unfused they are unstable. Minor trauma can lead to significant injury.
– Signs, symptoms, and physical exam
• Morning stiffness (milder than with AS)
• Globus: sensation of lump in the throat, secondary to large anterior vertebral body osteophyte adjacent to esophagus
• Dysphagia with or without weight loss1
– Neuroimaging/workup/treatment
• Dysphagia: speech therapy consult to rule out primary esophageal pathology, diet modification, barium swallow (to localize obstruction). Progressive dysphagia with weight loss may benefit from surgical debulking.5
• CT scan superior to x-ray for evaluation of osteophytic structures
• Conservative treatment unless mass effect on esophagus or surrounding structures causes significant health risk (i.e., weight loss from dysphagia, pneumonia, and respiratory difficulty)
• Initially a change in diet to soft mechanical may be beneficial.
– Surgical pearls
• Anterior approach, drill down osteophyte. Special attention needed for protection of surrounding structures.
• No instrumentation needed. Debulking only. Do not violate disc space.7
• Initially, postop patients may have increased dysphagia. Risk of gastrostomy tube requirement.1
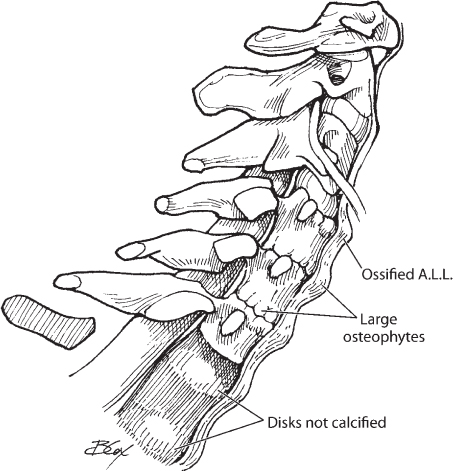
Fig. 24.2 Diffuse idiopathic skeletal hyperostosis in the cervical spine. Note the continuous osteophyte formation along the anterior border of the cervical spine.
V. Ossification of the Posterior Longitudinal Ligament
– Background
• Calcification with subsequent ossification of PLL. Can occur in any part of the spinal column and can extend into dura. Most commonly cervical (C3-C6).
• Classified as segmental when ossification skips area behind disc space and is present only behind each vertebral body. (Mixed type and focal form exist.)
• Increased incidence in Asian (Japanese) population (prevalence around 2%).5,12 Prevalence increases with age (average age at time of diagnosis is mid-50s).
– Signs, symptoms, and physical exam
• Most are asymptomatic but can progress to myelopathy over time.13
• Symptoms can range from subjective neck pain to severe myelopathy.
– Neuroimaging/workup
• Plain x-rays will miss the ossification. Therefore, CT is suggested when OPLL is suspected.
• MRI or CT with intrathecal contrast for evaluation of degree of stenosis
• MRI: ossified PLL is dark on T1 and T2.
• Consider glucose level check given the higher frequency of OPLL patients with diabetes mellitus (DM)
– Treatment
• Surgical treatment required to decompress the spinal cord. Patients with myelopathy can benefit from early decompression.
• Patients with mild subjective complaints can be treated conservatively.
– Surgical pearls
• Nasotracheal/fiberoptic intubation should be strongly considered to prevent hyperextension.
• Surgeon’s prerogative as to whether or not to leave a thin rim of ossified PLL attached to the dura during decompression. Note that the ossification usually extends into the dura and is inseparable.1
• Anterior approach (corpectomy) as opposed to posterior (laminectomy/laminotomy) decompression is controversial because of the significant risk associated with resecting all of the OPLL.14 Leaving a thin layer of bone that is adherent to the dura is recommended. Nerve root decompression is required.7
• Somatosensory evoked potential (SSEP) monitoring highly recommended.
Common Clinical Questions
1. A 65-year-old male comes to the hospital after a motor vehicle accident complaining of neck and back pain. Further questioning reveals that the patient has had a history of chronic neck ache with morning “back stiffness.” He also admits to having mild dysphagia with the sensation of a lump in his throat. Initial x-rays show significant vertebral osteophyte formation but are otherwise negative. Hip x-rays show normal hip and pelvic joints with no fractures. What is the patient’s most likely diagnosis?
A. OPLL
B. DISH
C. Ankylosing spondylitis
D. Acute cervical fracture
2. A 65-year-old Japanese male comes to your office complaining of not being able to keep objects in his hands and “dropping things.” Your exam is positive for bilateral Hoffman 3+ reflexes and 4/5 weakness of intrinsic hand muscles. Cervical spine MRI with central canal stenosis and cervical dynamic x-rays are normal. Careful analysis of MRI indicates a hypointense signal on T1 and T2 lining the posterior side of the vertebral body at C3-C5 with sparing of disc space. What is the most likely diagnosis?
A. Primary bone tumor
B. Metastatic disease
C. DISH
D. Segmental OPLL
3. True or false: An ADI >3 mm correlates with increased risk of cervical injury.
4. Dynamic imaging indicates C1-C2 instability. Which of the following is not a recommended treatment?
A. Cervical fusion secondary to ADI >10 mm
B. Rigid cervical collar with close follow-up
C. Halo fixation with subsequent close follow-up imaging in an effort to decrease pannus size
D. Cervical fusion and decompression secondary to symptoms of myelopathy
5. True or false: Enthesitis is a chronic inflammation at the insertion point of the tendons into the spine that can become ossified.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







