Fig. 26.1
Lordotic cage placed in the intervertebral disc space. Note that it spans the lateral endplate on both the right and left sides of the apophyseal ring, which is the region with the strongest endplate bone
26.7 Case Illustration
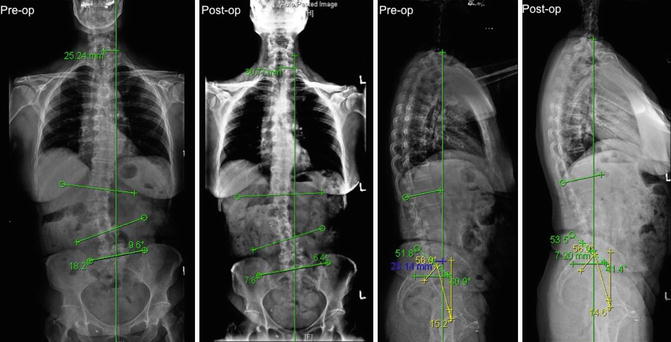
The patient is a 73-year-old female present with complaint of progressive chronic back pain over 10 years. She has failed conservative therapy that included physical therapy and pain management. She underwent left MIS lateral interbody fusion as stand-alone construct. Standing scoliosis films show:
Preop | Postop | |
|---|---|---|
Coronal Cobb angle | 18.2 | 7.8 |
SVA | 2.3 cm | 0.7 cm |
CSVL | 2.5 cm | 3.0 cm |
Sacral slope | 40.9° | 41.4° |
Pelvic incidence | 56° | 56° |
Pelvic tilt | 15.2° | 14.6° |
Lumbar lordosis | 51.8° | 53.5° |
Fractional curve | 9.6° | 6.4° |
Conclusions
The importance of understanding the differing risk characteristics of an aging population with spinal deformity cannot be overstated. Lateral stand-alone surgery for adult spinal deformity is a viable option in very selective patient population. Combined approaches for correction of spinal deformity provide the best chance for correction of spinopelvic alignment and neural decompression. However, certain patients may have unacceptable risk with combined or more invasive procedures. A patient’s comorbid medical condition can affect postoperative outcomes [27, 28]. In this select few of patients who have failed conservative therapies, spine practitioners may consider a stand-alone construct. The advantages of the MIS-LIF include minimization of muscle dissection/trauma, shorter operative time, relatively decreased blood loss, preservation of anterior/posterior longitudinal ligaments, maximization of interbody cage size, indirect foraminal decompression, and relatively earlier postoperative mobilization. MIS-LIF is a safe feasible alternative to traditional surgical approaches in a selected group of patients with adult spinal deformity.
References
1.
3.
4.
Pimenta L. Lateral endoscopic transpsoas retroperitoneal approach for lumbar spine surgery. VIII Brazilian spine meeting, Belo Horizonte, Minas Gerais, Brazil; 2001.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








