Figure 40.1. Stroke Code of The Madrid Stroke Network. Activation and distribution of stroke patients by the emergency coordination center.
- Infrastructure:
- Stroke Unit.
- Intensive Care Unit.
- Emergency Department.
- Stroke Database.
- Stroke Unit.
- Personnel:
- Neurologist physically present in the hospital every day and 7 days a week.
- Interventional neuroradiologist 24/7.
- Stroke Medical Coordinator.
- Stroke-trained neurologists.
- Stroke-trained nurses.
- Rehabilitation physician and physiotherapists.
- Stroke-expert neurosurgeons.
- Vascular surgeons with experience in carotid surgery.
- Diagnostic radiologists expert in stroke diagnosis.
- Intensivists.
- Social workers.
- Neurologist physically present in the hospital every day and 7 days a week.
- Diagnostic procedures:
- Extracranial and transcranial doppler sonography.
- Extracranial and transcranial duplex sonography.
- Brain diagnostic imaging: CT and MRI.
- Vascular neuroimaging: angio-CT, magnetic resonance angiography, transfemoral cerebral angiography.
- Functional neuroimaging.
- Echocardiography.
- Extracranial and transcranial doppler sonography.
- Invasive treatments:
- Revasculazation procedures: carotid surgery, angioplasty and stenting.
- Endovascular procedures: aneurysm and intracranial vascular malformations, intraarterial reperfusion and recanalization.
- Neurosurgical procedures: hemicraniectomy, surgical evacuation of brain hemorrhage, external drainage for hydrocephalus, surgical excition of aneurysms and intracranial vascular malformations.
- Cardiovascular surgery.
- Revasculazation procedures: carotid surgery, angioplasty and stenting.
- Programs:
- Established networks with extra- and intra-hospital stroke codes (Figures 40.1 and 40.2).
- Multidisciplinary work plans with participation of different specialists involved in stroke management: vascular surgeons, neurosurgeons, cardiologists, rehabilitation physicians, neuroradiologists.
- Diagnostic and therapeutic protocols.
- Education and research programs.
- Established networks with extra- and intra-hospital stroke codes (Figures 40.1 and 40.2).
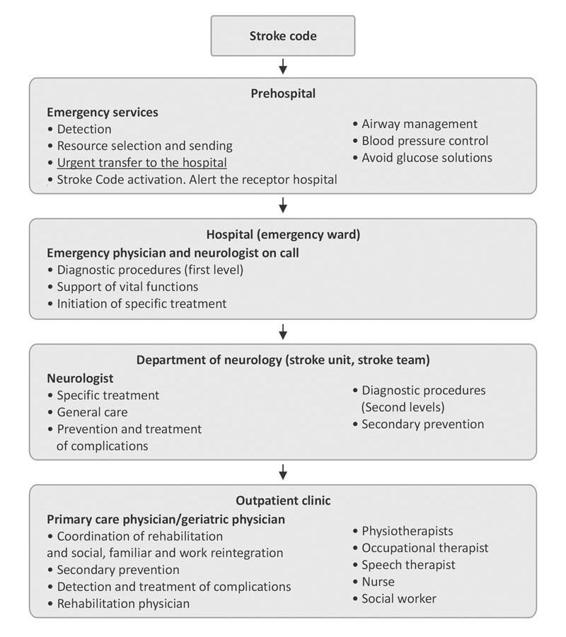
Figure 40.2. Integration of extra-and intra-hospital stroke code in a stroke care network. Priorities and tasks.
40.5.2 Stroke Unit Hospitals
They are provided by a stroke unit with all the diagnostic and therapeutic procedures needed for acute stroke care, with a neurologist physically present in the hospital every day and 7 days a week. Recommended organizational elements are:
- Infrastructure:
- Stroke Unit.
- Intensive Care Unit.
- Emergency Department.
- Stroke Database.
- Stroke Unit.
- Personnel:
- Stroke Medical Coordinator.
- Neurologist physically present in the hospital every day and 7 days a week.
- Stroke-trained nurses.
- Physiotherapists.
- Stroke Medical Coordinator.
- Diagnostic procedures:
- Brain CT scan 24/7.
- Emergency laboratory 24/7.
- Extracranial and transcranial sonography.
- Non-invasive multiparametric monitoring.
- Brain CT scan 24/7.
- Programs:
- Established networks with extra- and intra-hospital stroke codes.
- Multidisciplinary work plans with participation of different specialists involved in stroke management: vascular surgeons, neurosurgeons, cardiologists, rehabilitation physicians, neuroradiologists.
- Diagnostic and therapeutic protocols.
- Established networks with extra- and intra-hospital stroke codes.
40.5.3 Stroke Team Hospitals
In those hospitals where a stroke unit is not possible, mainly because of the scarce number of acute stroke patients admitted, stroke care is provided by stroke teams, defined as multidisciplinary teams specialized in stroke management. As they are not large enough, these hospitals do not generally have a neurologist physically present 24/7 nor the facilities for specific treatments like intravenous thrombolysis during the acute stroke phase. When necessary, patients are transferred to a hospital with a stroke unit or to a stroke center in order to complete the treatment. To ensure fluidity of patient referral systems and to allow early administration of drugs within a narrow therapeutic window, it is essential to develop inter-hospital coordination systems included in the stroke networks. These hospitals will have:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







