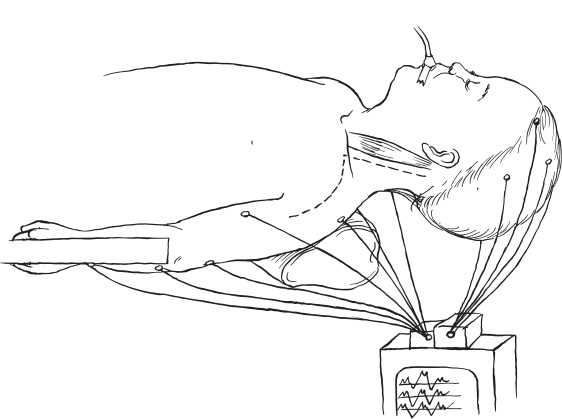
The role of pediatric neurosurgeons in the treatment of infants with birth-related brachial plexus injuries has increased steadily over the last 10 years. Previously, these children were referred to orthopedic and plastic surgeons, neurologists, and physical therapists. Symptomatology of birth-related brachial plexus injuries is usually first observed by the obstetrician, midwife, or infant’s family shortly after birth. Obstetric factors related to brachial plexus injury at birth include a multiparous mother, prolonged labor, high birthweight, and vertex delivery with shoulder dystocia. Brachial plexus injuries have been seen in premature births and cesarean sections. These injuries are more common with breech deliveries; this presentation is relatively rare compared with vertex presentations. Most children who present with birth-related brachial plexus injuries demonstrate classic Erb’s type upper plexus lesions of roots C-5 and C-6. The arm is clinically limp, the shoulder abducted with its upper part internally rotated, the elbow extended, and the forearm pronated with flexed wrist and fingers. Other levels of involvement can include C-7, which causes triceps paresis and some insufficiency of wrist and finger extension. A C-4 root lesion causes phrenic nerve palsy with accompanying respiratory problems. In contrast to radiculopathies, brachial plexus neuritis, and tumors among adults, the birth-related brachial plexus syndrome does not include pain. Patients with classic Klumpke’s syndrome, a variety of brachial plexus injury rarely seen today, present with flexion in the elbow and extended wrist without finger movement; this syndrome involves the C-8 and T-1 roots, often with avulsion. The presence of Horner’s syndrome is diagnostic of C-8 and T-1 level lesions. Dysfunction of the dorsal scapular (rhomboid muscle) nerve or the long thoracic (anterior serratus muscle) nerve indicates a root-level injury. A lesion of the suprascapular (supraspinatus and infraspinatus muscles) nerve indicates an upper-trunk lesion. Combined total plexus lesions from C-5 to T-1 constitute the remaining cases. The entire plexus is involved at birth in most infants, with the neurologic level definitely established at age 6 to 8 weeks. Upper-plexus injury may be present without lower-plexus involvement, but lower plexus injury usually is not seen without some degree of accompanying upper plexus damage. The ability to use the limb is the best indicator of function, and, when possible, the Mallet scheme is invaluable. A diagnostic workup in an infant or young child should include careful inspection of the injured extremity from a distance and observation of how the child uses it: Does he or she reach for objects? If so, how are the objects handled? Finger and hand moisture (autonomic function) may be observed or may be evaluated either by iodine test or by Wickler’s test. In addition to movement, muscle atrophy, Horner’s syndrome, and withdrawal from pinprick should be assessed. Any or all these tests may be difficult in an overweight newborn. The patient is placed supine on the operating table. Anesthesia is induced, avoiding paralyzing agents, and less than 2.0% fluorane levels are used. Bilateral surface skull electrodes for electroencephalograms are placed 3 cm from the sagittal suture and 8 cm from the coronal suture on the parietal region of the skull. Bifrontal skull electrodes also are placed. Needle electrodes are positioned at the base of the skull, over the C1–2 region. The reference electrode is the inion. Dermal electrodes are placed on the ipsilateral rhomboid, infrascapular, suprascapular, both heads of the deltoid, both heads of the biceps, triceps, extensor carpi radialis, flexor carpi radialis, adductor pollicus minimus, abductor pollicus brevis first interosseous, and adductor minimus V muscles. The head is turned to the contralateral side. The ipsilateral arm is extended, lowering the clavicle on the affected side. Identification of the sternal notch, the acromiun process, and the position of the clavicle permits palpation of the brachial plexus in the sleeping patient. Following thorough cleaning of the surgical site, both anterior cervical neck areas as well as both lower extremities are draped in a specially adapted clear plastic drape that permits assessment of upper extremity muscle movements during direct stimulation of nerve of the brachial plexus (Fig. 19–1). A curvilinear incision is made on the lateral border of the sternocleidomastoid muscle to the medial portion of the clavicle and then carried laterally 1 cm below the clavicle to the axillary junction. Evidence of prior subcutaneous injury with xanthochromic staining of scar tissue, dense scar tissue of ruptured muscles, thick fasciallayer injury, induced fatty degeneration, increased vascularity, and attempted regrowth of neural tissue will blanket the normally loose adipose—fascial plane over the brachial plexus. No distinct surgical planes of cleavage will be present. The internal jugular vein is carefully dissected to its junction with the subclavian vein under the clavicle. The carotid artery is palpated medial to the jugular vein. The external jugular vein is ligated and coagulated at its junction with the internal jugular vein. A large transverse vein superior to the scalene anterior muscle is usually present and is ligated to permit access to the distal phrenic nerve. The entire length of the phrenic nerve is carefully dissected from the anterior surface of the scalene anterior muscle and noted to be intact morphologically. The proximal phrenic junction with the C-4 nerve root is identified. The C-4 root is explored to its neural foramen and its exit from the spinal cord. The distal C-4 nerve is dissected to expose the three distal branches, which are freed to their entrance into the colli muscles of the neck. Identification of the XI cranial nerve distal branches into the sternocleidomastoid muscle and exposure of the XII cranial nerve’s hypoglossal division are made to prevent injury to these structures. The C-5 nerve-root contribution to the phrenic nerve is exposed, and the C-5 nerve root is dissected to its neural foramen. Dense postinjury scar tissue is usually adherent to a neuroma. The overlying thinned, scarred, ruptured platysma and cervical muscles are identified. The omohyoid muscle is transected at its medial origin near the internal jugular vein and distal transection as it passes inferior to the clavicle. Removal of a postinjury scarred fat pad usually (95%) reveals a fusiform neuroma. Proximal exposure of the neuroma will expose the previously dissected C-5 nerve root. Identification of the suprascapular peripheral nerve to the infrascapular and suprascapular muscles as it exits from the upper trunk permits exposure of the distal portion of the neuroma. Vascular loops placed around the nerves and around the neuroma are for retraction purposes. Before proceeding with the distal dissection of the neuroma, the subclavicular area structures (subclavian artery and vein) need to be identified. The scar tissue surrounding the distal brachial plexus divisions and cords and peripheral nerves near the clavicle is removed. Vascular loops are placed around the posterior division of the upper trunk, the upper trunk, the anterior-division musculocutaneous nerve complex, the posterior division of the middle trunk, middle trunk, and lower trunk of the brachial plexus (Fig. 19–2).
INDICATIONS AND PREOPERATIVE EVALUATION
INTRAOPERATIVE TECHNIQUES
Anesthesia and Positioning
Exposure
Dissection and Exploration
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


