Chapter 41 Surgical Management of Lesions of the Clivus
Different pathologic lesions can develop in this region.1 Histologically, clival lesions can be benign (e.g., meningiomas, epidermoid cyst, cholesterol granuloma, or glomus jugulare tumors with major petroclival involvement), of low-grade malignancy (e.g., chordomas and chondrosarcomas), or of high-grade malignancy (e.g., squamous cell cancer, adenocarcinoma, basal cell carcinoma, osteogenic sarcoma, or metastases). Some of these tumors have an intradural location, whereas others are extradural.
The lesions that most often involve this region are meningiomas (commonly intradural), followed (much less commonly) by chordomas, which are often extradural. The former grow from the dura that covers the clivus or the passage from the clivus and the petrous bone (petroclivus fold),2 whereas the latter originate directly from embryonic residues enclosed in the bone of the clivus.3–6
Tumors in the region of the clivus are difficult to treat using conventional neurosurgical approaches. Until a few decades ago, because of the relative inaccessibility of the clivus and its proximity to the brain stem and surrounding neurovascular structures, the results of surgical treatment were so dismal that these tumors were often considered incurable.1
Advances in microsurgery of the skull base have resulted in the development and refinement of approaches to petroclival and clival lesions,7–57 better methods for tumor removal, and innovative techniques44,45,58–62 to minimize injury to neural and vascular structures during tumor removal. These factors enable the surgeon to treat these tumors more effectively, aiming at a radical excision with an acceptable morbidity and mortality.
In some cases, the combined effort of the neurosurgeon with those in other disciplines interested in skull base surgery (e.g., otolaryngology or maxillofacial surgery) constitutes real progress in the realization of special approaches that aim at improving the exposure of the tumor and reducing trauma to the brain during surgery. Endoscopic skull base surgery is the most recent result of this multidisciplinary concept.63
In recent years, the introduction of the endoscope in trans-sphenoidal surgery and the use of extended endoscopic approaches have allowed resection of chordomas involving the lower clivus, and even the odontoid, with good short-term results and low surgical morbidity.64–72
Surgical Anatomy
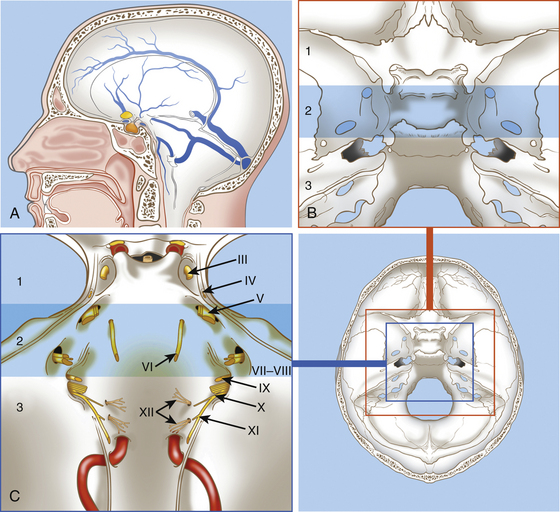
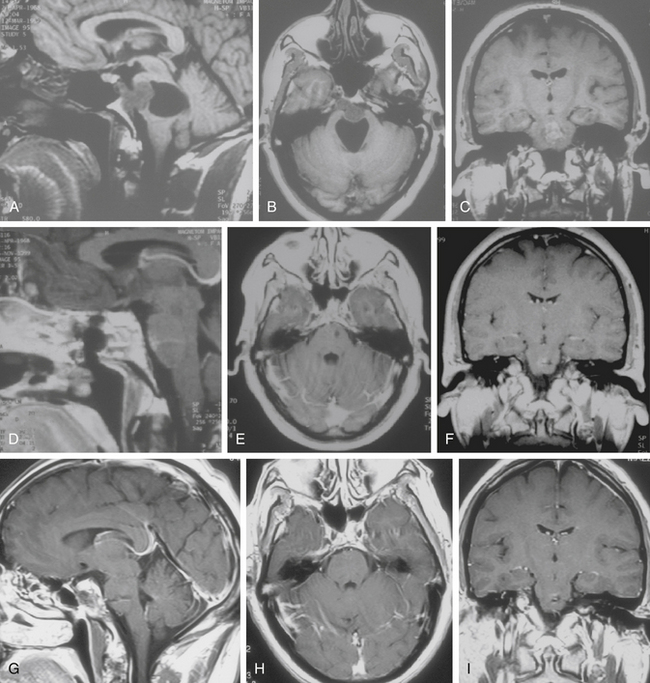
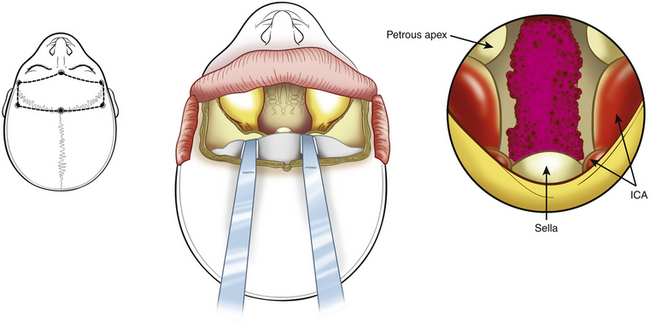
The clivus is located at the midline, in the deepest part of the skull base. It constitutes the inclined anteroinferior surface of the posterior cranial fossa and extends from the dorsum sellae to the foramen magnum (Fig. 41-1). It is formed by a sphenoidal part (corresponding to the superior third) that extends from the dorsum sellae to the spheno-occipital synchondrosis and by an occipital part (corresponding to the inferior two thirds) that reaches the anterior intraoccipital synchondroses.3,73
The clivus is usually divided into the upper, middle, and lower clivus25 (see Fig. 41-1) or into superior and inferior halves of the clivus.74
The topographic anatomy of the clivus makes several surgical approaches feasible.1,11,34,35,37,41,75,76 The choice of an approach to remove a tumor from this region must take into account the nature and location of the lesion (i.e., whether the lesion is intradural or extradural, its position in respect to the clivus, and its lateral extension).
The surgical approaches to the clivus are divided into three general groups: (1) anterior, (2) anterolateral, and (3) posterolateral. Anterior approaches are mainly used for extradural lesions that primarily involve the clivus and extend extracranially (e.g., chordoma and chondrosarcoma). For these tumors, the anterior approaches are usually extradural and include the trans-sphenoidal, transethmoidal, transoral–transpalatal, transmaxillary, and transcervical. A subfrontal transbasal extraintradural anterior approach can also be indicated for huge tumors with maximal involvement of the clival area and surrounding structures (e.g., chordoma, pituitary tumors, and craniopharyngiomas).
Extradural Lesions: Chordomas
Chordomas are the most common extradural tumors of the clivus; they arise from remnants of the embryonic notochord and are located in all areas where the notochord existed (i.e., the entire clivus, sella turcica, foramen magnum, C1, and nasopharynx).3,5 From there, they may spread to the upper cervical region, petrous bone, posterior fossa, cavernous sinus, middle fossa, nasopharynx, and sphenoid sinus.3,5 Chordomas grow slowly but may present the characteristics of a malignant tumor in that they are locally aggressive with a tendency for regrowth.77 About 20% of chordomas recur as early as 1 year after surgery despite extensive surgical resection.48,78 Ten percent of chordomas show histologic signs of malignancy.5 Although it is considered difficult to identify histologic features indicative of aggressiveness,79,80 recent studies indicate that some molecular features of these tumors are associated with an aggressive biologic behavior.47,48,78,81,82 Metastases are relatively rare.78,80
Chordomas infiltrate the bone and spread into the epidural space, seeding the dura with microscopic deposits well beyond the limits of the tumor bulk.5,83 For this reason, they may invade the dura and become adherent to the arachnoid and pia mater. The tumor is often gelatinous and soft, with a jelly-like consistency, but it may also appear as a firm cartilaginous mass.
Chordomas are usually classified according to the portion of clivus involved by the tumor and by the extension to surrounding structures (e.g., upper clivus, middle clivus, lower clivus, and craniocervical junction tumors, with or without invasion of sphenoid, cavernous sinus, and petrous bone).1,3
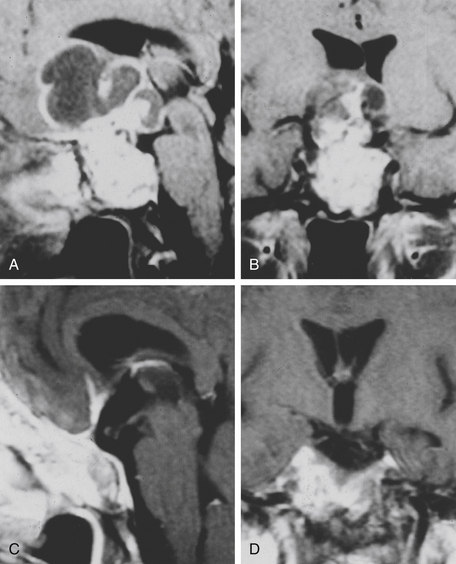
Computed tomography (CT) scan and magnetic resonance imaging (MRI) are the most important radiologic tools for diagnosis. The CT scan reveals the destruction of bone, whereas MRI shows the extension of the tumor, which appears nonhomogenously hyperintense on T2-weighted images and with a variable contrast enhancement after gadolinium.4
The most commonly involved cranial nerve is the sixth, and diplopia is the most common presenting symptom, particularly in the midclivus chordomas. Other symptoms include headache, pituitary dysfunction, visual field defects, cerebellar syndrome, torticollis, and brain stem syndrome.84
Surgical Treatment
Its deep position (at the central base of the skull) and its tendency to infiltrate the bone make total removal of the clivus chordoma difficult. Total resection leads to a significant improvement in survival at 5 years, with 90% and 52% with complete and partial resection, respectively;85 at 10 years, the recurrence-free survival rate in a large series for primarily operated patients (with a complete resection of 83%) was 42%; for reoperation cases (complete resection achieved in 30% of patients), it was 26%.86
In recent years, because of the development of innovative and complex approaches to the clival area29,30,34,35,37,41,42,67,68,86–91 and the extensive application of standard procedures to this area,12,13,16,36,38,84,92–100 many possibilities are at the disposal of the surgeon attempting radical removal of these tumors.
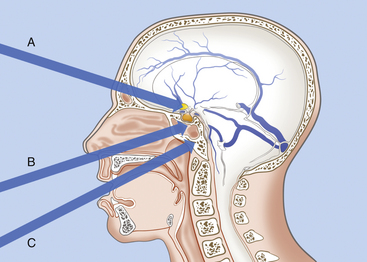
Because chordomas are basically extradural and midline tumors, they displace the neuraxis dorsally or dorsolaterally. Anterior midline extradural approaches are generally preferred (Fig. 41-2).20,46,52,83,92,101–105 These approaches allow a midline exposure of the clivus and a short working distance, avoiding any retraction of the brain.
The choice of surgical approach depends on the location and extension of the tumor. Even when only anterior extracranial approaches are considered, many options exist. These include the transbasal,13 extended subfrontal,104 microscopic trans-septal trans-sphenoidal,16,84,93–94 modified microsurgical endoscope-assisted sublabial or endonasal trans-sphenoidal,98,99 endoscopic endonasal trans-sphenoidal,64,67–71 trans-sphenoethmoidal,92 transmaxillary transnasal,106 transfacial,107 facial translocation,108 transmaxillary,109–110 midfacial degloving,103 transoral,12 mandible-splitting transoral,94 transcervical transclival,111 and anterior cervical112 approaches; Le Fort I osteotomy;113 unilateral Le Fort I osteotomy;114 total rhinotomy; and pedicled rhinotomy.115
All of these approaches are devoted to removing all clival lesions localized on the midline without important lateral extent. In the case of massive lateral extension, in which a midline approach is insufficient for the removal of the entire tumor, complex lateral approaches can be utilized as a primary or secondary procedure.1,5 These include, for lesions of the upper clivus, the subtemporal, transcavernous, and transpetrous apex approaches; for lesions of the midclivus, subtemporal and infratemporal approaches; and for lesions of the lower clivus with lateral extension to the occipital condyle, jugular foramen, and cervical area, the extreme lateral transcondylar (“far lateral”) approach.26,43,86,116
• For chordomas located in the upper and middle clivus, the trans-sphenoidal approach is favored.
• For lesions of the lower clivus that involve the foramen magnum, C1, and C2, the transoral approach is preferred, with or without splitting of the palate.
• For tumors in the lower clivus, foramen magnum, and first cervical spinal bodies, with important lateral extension, the Le Fort I osteotomy can be used with a midline incision of the hard and soft palate and lateral swinging of the two flaps of the hard palate.
• For huge tumors involving the entire clival area, the sphenoid, and the sellar region and extending anteriorly to the optic nerves, the transbasal or extended subfrontal route is utilized.
• For lesions that involve the lower clivus and the upper cervical region and that extend laterally into the occipital condyle and the jugular bulb on one side, the extreme lateral approach with partial condylectomy seems particularly well suited.
Other anterior approaches can be utilized, including the following:
• The trans-sphenoethmoidal approach92 provides access to the entire sphenoid sinus, prepontine space, and superior clivus; a limited medial maxillectomy improves access to the inferior clivus.
• The transfacial approach107 is indicated for extradural tumors confined on the midline and extending from the level of the sellar floor to the foramen magnum. This approach offers direct access to the clivus along its rostrocaudal extent up to the anterior arch of C1; with depression of the palate, the odontoid can also be visualized. The main advantage is to add, by this single facial route, the possibilities of the trans-sphenoidal and transoral routes, avoiding any injury to the hard and soft palate. The disadvantages are a facial scar and osteotomy of the facial skeleton.
• The recent application of the endoscope to trans-sphenoidal surgery, in either endoscope-assisted or pure endoscopic approaches, provides wider visualization of lesions extending from the upper clivus to the odontoid process; in the future, they will probably be substituted for most transfacial routes, even for tumors extending inferiorly to the odontoid and laterally to the petrous apex.64–72117
Trans-sphenoidal Approach
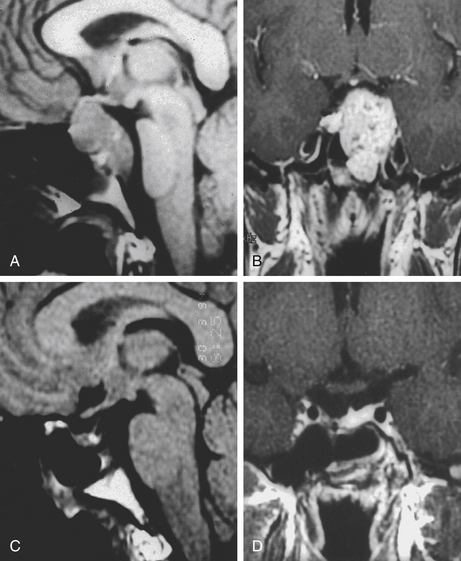
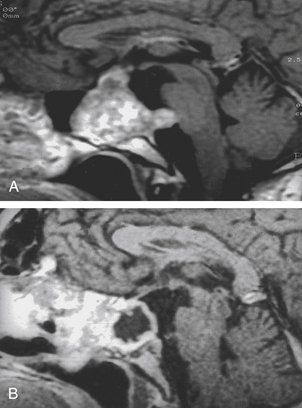
The trans-sphenoidal approach provides excellent exposure to chordomas of the sphenoid sinus, sella turcica, and upper and middle clivus (see Fig. 41-2), minimizing the morbidity of more complex surgical approaches13,16,84,96 with a route that, where necessary, can easily be repeated. The technique utilized for the sublabial trans-septal trans-sphenoidal procedure has already been described.118 Extensive experience obtained with pituitary tumors119–120 and with craniopharyngiomas121 has made this route safe and effective, even for other pathologies (Figs. 41-3 to 41-6). Several papers have reported that gross total tumor removal can be achieved in up to 70% of cases using the trans-sphenoidal approach, with excellent long-term survival and no evidence of disease at a mean of 38.6 months after surgery.84,94,95,98,99
The main disadvantages of this approach are represented by the limited lateral exposure and the deep and narrow field. Nevertheless, the correct use of long and angled curettes can allow a skillful surgeon to remove even large tumors (greater than 4 cm) that are not strictly confined to the midline.78 Application of endoscopy to the trans-sphenoidal route may increase the surgical field and allow even extensive tumors to be removed.45,64,67–71
When the tumor is found to be located intradurally, an opening of the dura mater can be realized to remove the intradural tumor. Afterward, an accurate reconstruction must be realized. We usually use a dural patch and fibrin glue. When a major intraoperative CSF leak (grade 3122) is evident, a lumbar drain is kept in place for 48 to 72 hours postoperatively.
Transoral Approach
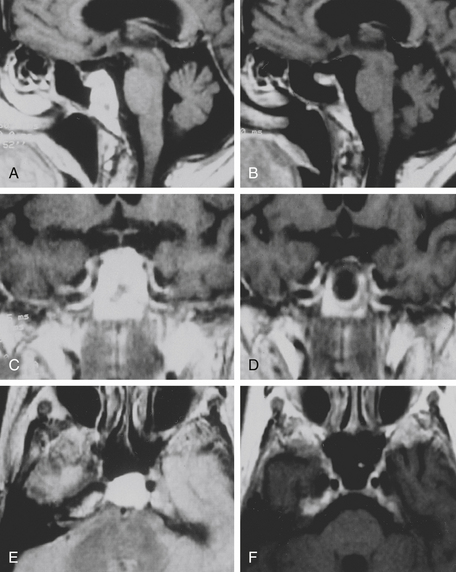
The transoral route is indicated for extradural lesions of the inferior clivus that are confined to the midline, protrude into the posterior pharyngeal region, and extend to C1 to C2 (see Fig. 41-2). The approach provides good exposure with limited surgical trauma.75,123 This route has been used for many years for epidural tumors of the cervical spine.124 Several reports have described the utilization of this surgical route to treat clivus chordomas.125–127
A modified transoral version has been described for chordomas.110,113 It combines the Le Fort I osteotomy with a midline incision of the hard and soft palate and allows lateral swinging of the two flaps of the hard palate based on their own palatine artery and nerves. The advantage is extensive exposure of the region, inferiorly and laterally (Fig. 41-7); the wound must be closed carefully to preserve occlusion and functioning of the palate. A unilateral Le Fort I osteotomy can be realized for laterally growing tumors.114 Neuronavigation in transoral approach has been found to be a useful tool for planning and checking the limits of resection and for reducing morbidity in chordoma surgery.44
The Endoscope: A Surgical Adjunct for Wider Vision and Exposure
As a result of technological progress and collaboration between neurosurgeons and otolaryngologists,63 the endoscope has been applied to trans-sphenoidal and transoral surgery to get visualization in these deep surgical corridors that is wider than the microsurgical vision. The use of the endoscopes in microsurgical approaches has allowed a view behind the corner achieved by angled (30 and 45 degrees) scopes.98,99 The main limit of endoscope-assisted microsurgery remains though the narrow surgical corridor in which the endoscope is positioned; this reduces the endoscope to a complex mirror to visualize tumor remnants, as tumor removal under an endoscopic view may be not possible because of the space limitation created by the self-retractor.
In recent years, “pure” endoscopic trans-sphenoidal approaches have been developed63 that use only the endoscope as a visualization tool. The approaches are performed through both nostrils to allow for a bimanual technique and a wide range of free motion. The major limit of pure endoscopic skull base surgery is the loss of the binocular vision provided by the microscopic technique. When the wider visualization achieved by the endoscope is coupled with wider exposure, the full advantage of the endoscopic technique is achieved, extending the realm of trans-sphenoidal surgery to the cavernous sinus,128 petrous apex,117 lower clivus, and odontoid process.65,72
Results of the endoscopic series in the treatment of clival chordomas are at least comparable to the microsurgical trans-sphenoidal series,64,67,68,71 though the small number of patients and the short follow-up preclude definitive conclusions in terms of survival and recurrence rate.
The endoscope has also been applied to the transoral approach to the anterior craniovertebral junction in limited series.129 A pure endonasal endoscopic approach to C1 and the odontoid process has also been described.72,130 The main advantage of this approach, as compared to the transoral, is the visualization of the whole clivus and the avoidance of the soft palate splitting; its major limitation is the lowest extension of the surgical field, which is usually 9 mm above the base of the C2 body. The application of the endoscope to the transoral approach may reduce the need for splitting the soft palate yet maintain a satisfactory surgical maneuverability.131
Subfrontal Transbasal or Extended Frontal Approach
The subfrontal transbasal or extended frontal route can be utilized for chordomas with both intradural and extradural extension and with extensive involvement of the clivus and surrounding structures.5 The approach is a modification of the “transbasal approach” of Derome.13,132,133 After a bifrontal craniotomy (including the orbital roof and nasal bones), the anterior skull base is exposed extradurally on both sides (Fig. 41-8; see also Fig. 41-2). The planum sphenoidale and part of the anterior wall of the sella are removed. The clivus is reached anterior to the sella and exposed up to the rim of the foramen magnum (see Fig. 41-2). If the lesion presents an intradural extension, the frontal dura is opened. It also allows for the removal of tumors that extend near to the clivus (i.e., the frontal suprasellar region, orbits, paranasal sinuses, and temporal fossa). This approach has been used for different tumors such as craniopharyngiomas (Fig. 41-9), meningiomas, or pituitary tumors.
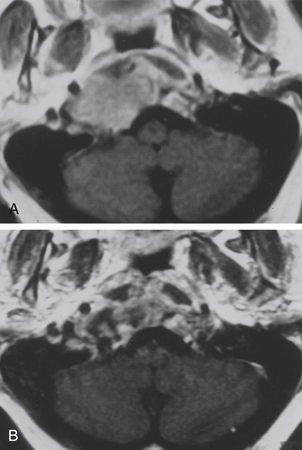
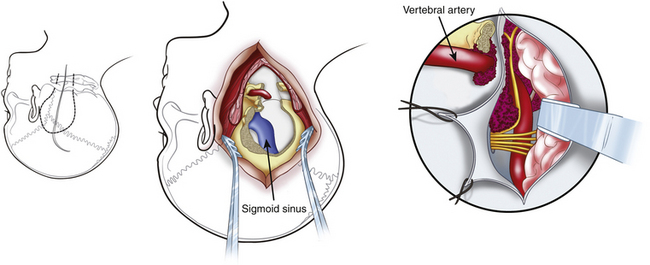
Extreme Lateral Transcondylar Approach
The extreme lateral transcondylar approach is useful for the management of both intradural and extradural lesions that involve the lower clival and foramen magnum regions (Figs. 41-10 and 41-11), with extension into the occipital condyles, jugular bulb, and upper cervical spine.15,26,134,135 The technical steps of the approach have been described by many authors.8,26,43,76,118,133 The main advantage of this route is the direct view that it offers to the ventral aspect of the foramen magnum without requiring brain stem retraction.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree