Chapter 42 Surgical Management of Posterior Fossa Meningiomas
Posterior fossa meningiomas are uncommon lesions that are most often slow-growing neoplasms manifesting in clinically indolent fashion. Based on clinical and radiographic information, the differential diagnosis is relatively straightforward; however, the range of management options can be considerable, including observation, surgery, and radiation in various forms and combinations. Although chemotherapeutic agents have been and continue to be investigated, this form of therapy is generally considered only for intractable, atypical, and malignant tumors and is not part of the general armamentarium in the majority of patients. Although the surgical management of meningiomas located in the posterior fossa may be challenging, patient-based outcomes studies suggest that long-term results can be encouraging.1
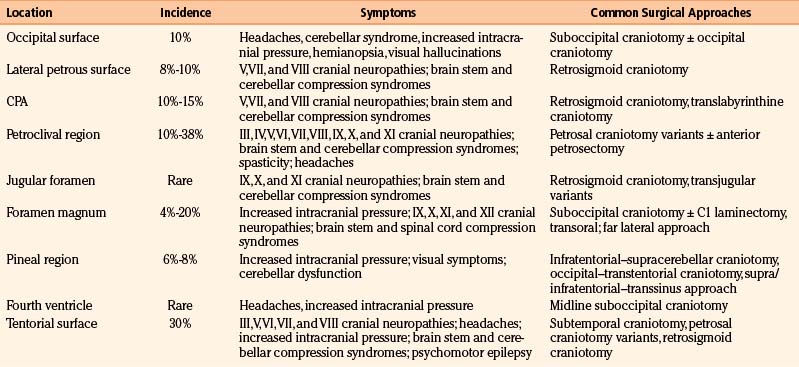
Posterior fossa meningiomas can be found anywhere in the posterior fossa, and individualized management recommendations depend primarily on size, growth rate, clinical presentation, and location (i.e., surgical accessibility). Tumors are primarily classified by their anatomic origin along the suboccipital surface of the cerebellum, lateral (i.e., lateral to the internal auditory meatus) petrous bone, cerebellopontine angle (CPA), petroclival region and clivus, jugular foramen, foramen magnum, pineal region, fourth ventricle, or tentorium (Table 42-1). Surgical accessibility varies based on location, with the most straightforward originating on the suboccipital surface of the cerebellum and lateral petrous bone; the more difficult originating on the tentorial surface, in the fourth ventricle, and at the CPA; and the most difficult originating at the petroclival junction. Each location is associated with different clinical implications regarding presentation and treatment strategy. Contemporary radiation therapy and radiosurgical decisions also depend on tumor location and the proximity of the tumor to critical neural elements. This chapter reviews the topic of posterior fossa meningioma from diagnosis though management and follow-up, in terms of both general and specific approaches relative to the various anatomic sites.
General Clinical Presentation and Diagnosis
The clinical presentation of posterior fossa meningiomas varies according to the location and size of the tumor, but because meningiomas are mostly slow-growing tumors, size plays less of a role in presentation and more of a role in choice of treatment strategy. Anatomically, the presenting clinical symptoms most often are related to involvement of cranial nerves and to a lesser degree the cerebellum, brain stem (i.e., long tracts), and fourth ventricle (i.e., hydrocephalus). Headaches are a common but nonspecific symptom. More specific clinical features based on location are discussed in the individual sections (see Table 42-1).
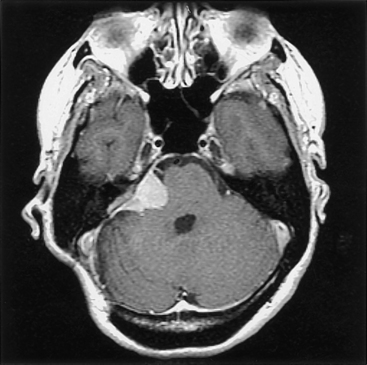
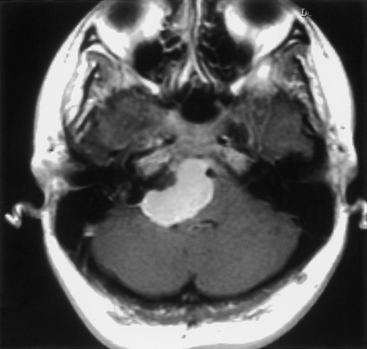
The diagnosis of meningioma is generally made radiographically, and most tumors share certain imaging characteristics. Plain radiographs, although no longer commonly utilized, often demonstrate bony hyperostosis, bony erosion, calcification, and occasionally, evidence of enlarged vascular channels. Transaxial computed tomography (CT) most often shows a hyperdense tumor signal (75% of cases) that intensely and homogeneously enhances after contrast administration. Cystic regions within the tumor can be seen but are uncommon, and peritumoral low-density suggestive of edema is noted in up to 60% of tumors.2 Calcification can also be noted on CT, but hemorrhage is distinctly uncommon. Three-dimensional computed tomography angiography (3D CTA) is useful in patients with skull base meningiomas. 3D CTA provides images that clearly depict the anatomic relationship between the meningioma and the bony structures of the skull base, as well as the relationship between the tumor and the neighboring vessels.3 Magnetic resonance imaging (MRI) most often reveals an isointense or hyperintense lesion on T1-weighted imaging, which is heterogeneous on T2-weighted imaging. These tumors almost always intensely enhance after gadolinium administration. The dural tail sign is one of the most revealing characteristics of meningioma, even though it is not pathognomonic (Fig. 42-1). A high-intensity signal noted on T2-weighted imaging is typical of peritumoral edema.2 While unproven in a large series of patients, diffusion-weighted MR imaging has been noted to correlate with the histopathologic features of certain meningiomas before resection.4 Cerebral angiography commonly (but not invariably) reveals an intense vascular supply, primarily from the dural arteries; a prolonged stain in the late venous phase of the angiogram is also common. Given the efficacy of magnetic resonance angiography (MRA), magnetic resonance venography (MRV), and 3D CTA for diagnosis and surgical planning, conventional angiography is used less frequently today. Nevertheless, it is still required for preoperative embolization.
Cerebral Angiography and Embolization
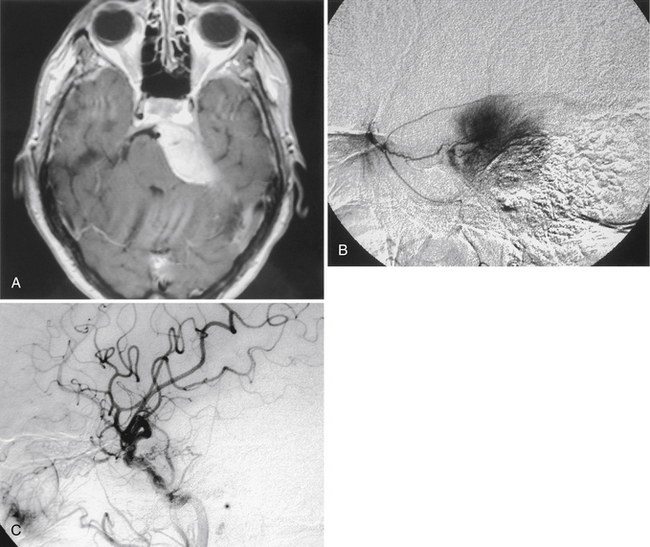
Given the limited space in the posterior fossa, the surgical removal of a highly vascular lesion can be fraught with difficulty (e.g., persistent bleeding obscures the operative field, requiring greater patience on the part of the surgeon to avoid increased morbidity), and although ideally the surgeon will select an approach that allows eradication of the tumor’s vascular supply early in the operation, this is not always possible or sufficient. In these instances, preoperative arterial embolization can be helpful, especially for selected tumors in the posterior fossa5 (Fig. 42-2). The primary reservations regarding embolization generally include risk of stroke, retroperitoneal hematoma, and secondary tumor necrosis and swelling (possibly leading to clinical deterioration). In addition, because the vascular supply is commonly made up of internal and external vessels, external carotid embolization may shift vascular supply to more-difficult-to-control internal carotid branches. Nevertheless, our experiences and those of others suggest that embolization can be helpful.6,7 Most authors conclude that to be most helpful, embolization must achieve complete or near-complete eradication of the vascular supply to the tumor: partial interruption of the blood supply may leave the surgeon with a significant intraoperative bleeding challenge.
An additional issue relates to the timing of the surgical procedure relative to embolization. After an investigation of 50 patients, Chun and colleagues observed that more favorable results of embolization were noted with delays of longer than 24 hours, although the optimal delay was not specified.8 It has become the practice with all posterior fossa tumors at Henry Ford Hospital to delay the surgical procedure 48 to 72 hours from the time of embolization; because of the potential risk (albeit rare) of clinical deterioration from tumor swelling, the patient is admitted to the hospital until surgery.
General Treatment Considerations
The general management considerations surrounding meningiomas located in the posterior fossa run parallel to those for treating these lesions located in other regions of the brain. Because meningiomas are mostly slow-growing neoplasms, urgent and emergent management decisions are seldom required. Recent reports on residual disease after surgical resection of petroclival tumors indicate that the average growth rate is 0.37 cm/yr; this is associated with a median time to progression of 36 months, a median progression-free survival of 66 months, and a 5-year progression-free survival rate of 60%.9 Older age, menopause, and previous radiation therapy can be associated with slower growth. In addition, we found that meningiomas with evidence of calcification on CT scan have longer doubling times. Despite this indolent nature, the neoplasms seem to grow relentlessly, often by en-plaque growth along tissue planes, along the dura, and through the basal cranial foramina, thereby making accurate growth assessment by CT or MRI a challenge. For practical purposes, four management options are available: (1) observation alone, (2) surgical resection, (3) radiation therapy or radiosurgery, and (4) some combination of surgery and radiation.
Surgery
Realistically, most surgeons focus primarily on the removal of the significant bulk (i.e., Simpson grade III) of the tumor and “decompression” of neurologic structures, including the brain stem and cranial nerves.10 Although it is known that recurrence often follows when the tumor is not entirely removed, the morbidity associated with attempts at total resection is clearly higher. However, in the modern era, and in the hands of experienced surgeons, the extent of resection has dramatically improved and has been associated with a marked decrease in morbidity.11 This decrease in morbidity largely relates to the use of skull base surgical approaches that rely on bone removal as opposed to brain retraction to create tumor exposure.
General concepts are important for the successful removal of most meningiomas; these include adequate bony exposure, early eradication of vascular supply, debulking of tumor mass, and maintenance of the arachnoid plane. A sufficient bony exposure greatly facilitates surgical manipulation and allows the surgeon an opportunity to move from one section of the tumor to another. Although it is preferable to internally debulk most tumors so that the tumor capsule can be more easily separated from adjacent normal structures, for many vascular lesions, an approach that provides access to and early elimination of the vascular supply is desirable (Fig. 42-3). Once the vascular supply is eliminated, a far less challenging resection may be possible.
Caused partially by the location of the cells of origin of meningiomas, these tumors are commonly situated next to cerebral venous structures, the preservation of which is often critical. Generally, acute occlusion of major draining veins or sinuses as a result of surgical approach and/or dissection is likely to lead to cerebral edema and significant neurologic deficit, and it should be avoided. Despite this, instances of resection of the tumor-infiltrated walls of a patent sagittal sinus with successful repair, complete tumor resection, and maintenance of sinus patency have been reported.12 In addition, division of the sigmoid and transverse sinuses during petrosal and pineal approaches, respectively, have been reported.13,14 In principle, however, it is safest to avoid division of major veins and sinuses. It is quite reasonable to consider radical subtotal resections, leaving patent venous structures intact and following the patient to monitor growth of the residual tumor with consideration of delayed radiation.
Radiation
Conventional Radiation Therapy
Meningiomas are best managed with total excision, if that is achievable with acceptable morbidity. However, about one third of meningiomas are not fully resectable because of tumor location, size, and proximity to adjacent tissue and vascular structures. The posterior fossa is also a common site of residual postoperative disease.15 Because subtotal resection is associated with a higher chance of clinically significant recurrence than is total resection, postoperative radiotherapy has been common practice and is associated with improved local tumor control and low morbidity.16,17 The goals of radiotherapy are to prevent tumor progression, prolong the interval to recurrence, and improve survival whether administered as adjuvant or primary therapy.
As primary therapy, radiation therapy has been shown to be efficacious for tumor control and long-term relapse-free survival.18–21 The standard recommendation for external beam radiotherapy is a dose of 5400 to 6000 cGy in fractionated doses of 180 to 200 cGy to the entire tumor plus a 2-cm margin. Histologically benign meningiomas have most often been treated with a lower dose of about 5400 cGy, and malignant meningiomas have been treated with 6000 cGy. To these dosing standards, the recent addition of intensity modulated radiation therapy (IMRT) has significantly improved the delivery process. IMRT allows multiple and highly conformal radiation beams to be delivered to the tumor volume while significantly decreasing the dose to immediately adjacent tissue (e.g., the optic tracts, acoustic and facial nerves, and brain stem). Three-dimensional radiography, coupled with CT- or MRI-assisted computerized treatment planning, and precise tumor localization and patient immobilization techniques have all served to improve progression-free survival as compared with the techniques used previously.22
Radiotherapy has been used primarily as an adjuvant treatment after subtotal resection, for infiltrating tumor into the adjacent brain parenchyma or pathologic finding of atypia, and after multiple recurrences. Although postoperative radiotherapy has never been evaluated in a randomized trial, there have been large retrospective analyses, and the results of these strongly support its role following subtotal resection.17,18 Recurrence rates of 60% after subtotal resection versus 32% after subtotal resection plus radiotherapy at mean follow-up of 78 months, and 5-year freedom from recurrence of 59% after subtotal resection alone versus 77% after postoperative radiation therapy, have been noted.16 These studies also found that median time to recurrence was doubled by radiotherapy (i.e., 66 vs. 125 months), and this analysis was notable in that many of the irradiated patients had more adverse factors such as surgically unfavorable sites (e.g., posterior fossa) than did patients treated with surgery alone.
In another report, findings for skull base meningiomas (including those in the posterior fossa) did not differ significantly in terms of progression-free survival from similar findings for other, more favorable sites.15 An interesting observation suggests that the progression-free survival rate at 5 years for those patients treated before 1980 was 77% versus 98% for those treated after 1980, when CT and MRI became available for tumor localization and treatment planning.22 The Royal Marsden Hospital experience also supported the role for postoperative radiotherapy, particularly following subtotal resection.21 All patients were treated to a total dose of 5000 to 5500 cGy over 6 to 6.5 weeks. Interestingly, there was no significant difference in disease-free survival of minimum postoperative residual versus bulky residual; with actuarial disease-free survivals at 5, 10, and 15 years, patients with minimum residual tumor had survival rates of 78%, 67%, and 56%, respectively, whereas patients with bulky residual tumor had survival rates of 81%, 68%, and 61%, respectively.
As salvage therapy for patients with recurrent or progressive disease, radiotherapy may be used either alone or as an adjuvant to surgical resection. In these cases, local control with the radiotherapy appears equal or superior to that seen with resection alone.17,23,24 With a total dose of 4500 to 5500 cGy using older megavoltage radiation, the crude salvage rate was 50% as compared with 37% for reoperation alone.23 More recent reports showed 10-year tumor control rates in the range of 80% with adjuvant radiotherapy following reoperation, as opposed to 10% to 30% for surgery alone.24 Although the local control rate following salvage radiotherapy compares favorably with rates seen with immediate postoperative radiotherapy, these data should not be interpreted as sole justification for withholding radiation in the early postoperative period. Given the natural history of many meningiomas, progression, although common, is often extremely slow, and the decision as to when to radiate (i.e., immediate postoperative period vs. time of recurrence) is a matter for the treating physician and patient. In our practice, radiation is generally postponed to the time of demonstrable radiographic or clinical progression.
• Group I (low risk) includes gross total resection (Simpson grade I-III) and subtotal resection with World Health Organization (WHO) grade I. These patients will be closely observed.
• Group II (intermediate risk) includes gross total resection with WHO grade II and recurrent WHO grade I meningioma, irrespective of resection extent. These patients will undergo radiotherapy (54 Gy/30 Fr) by 3D CTA or IMRT.
• Group III (high risk) includes newly diagnosed or recurrent WHO grade III of any resection extent, recurrent WHO grade II of any resection extent, and newly diagnosed WHO grade II subtotal resection. These patients will be treated with radiotherapy (60 Gy/30 Fr) by IMRT.
Stereotactic Radiation Therapy and Radiosurgery
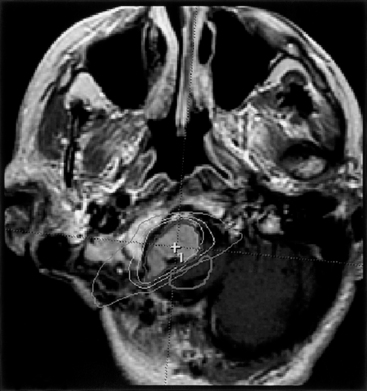
Despite the favorable results obtained with conventional fractionated radiotherapy for subtotally resected, unresectable, and “inoperable” meningiomas, the use of radiosurgery has evolved as both adjuvant and primary therapy. Controversy still exists, however, regarding the use and efficacy of radiosurgery. The arguments against the routine use of radiosurgery are largely based on the lack of long-term radiosurgical data and on the fear of potential delayed radiation injury to the brain tissue. However, considering the encapsulation of most benign meningiomas, the relatively low risk of infiltration into the adjacent brain tissue, the steep dose gradient characteristics, and the low reported morbidity (albeit after relatively short-term follow-up), the use of radiosurgery has become firmly established and is readily applied to meningiomas in the posterior fossa. Another significant concern has been the likelihood that secondary tumors will develop in the wake of radiosurgery, although few reports have appeared in the literature to date.25 Fractionated radiosurgery has also become readily available (Fig. 42-4), largely as a result of noninvasive patient immobilization methods, including “head mask” frame (i.e., noninvasive) and frameless image-guidance systems.
A recent report evaluating fractionated stereotactic radiotherapy showed survival rates of 97% for 5 years and 96% for 10 years after treatment, with local failure seen in only 3 out of 189 patients with WHO grade I meningiomas (22.5% located in the posterior fossa).26 These researchers noted tumor shrinkage (i.e., more than 50% reduction) in 14% of patients and resolution of preexisting cranial nerve symptoms in 28% of patients. Clinically significant treatment-related toxicity was seen in 1.6% of the patients.26 Outcomes data for radiosurgery are available for intracranial meningiomas generally, as well as for those located in the posterior fossa. Engenhart et al. reported an experience of radiosurgery in 17 patients with histologically proven benign meningiomas. Using a linear accelerator radiosurgery system, a maximum single dose of 10 to 50 Gy was used, with mean dose of 29 Gy prescribed to the 80% isodose line matching the tumor volume.27 The dose was chosen based on tumor volume, tumor location, and radiosensitivity of the adjacent brain tissue. Freedom from tumor progression was noted in 80% of patients, and late complications included transient neurologic deficits with perifocal brain edema and one case of visual loss.
Relating to intracranial meningiomas in general, Kondziolka et al. reported 2-year radiosurgical tumor control rates of 96% in 50 patients.28,29 The radiosurgery dose was 10 to 25 Gy (mean 17 Gy) to the tumor margin using a gamma knife unit; the doses were chosen based on tumor volume, location, previous radiotherapy dose, and adjacent critical normal tissue (e.g., optic chiasm). Tumors greater than 35 mm in diameter and located within 5 mm from the optic chiasm were excluded for radiosurgery. Three patients experienced delayed neurologic complications, thought to be consistent with radiation injury at 3 to 12 months following radiosurgery.28–30 In another report from the Mayo Clinic on radiosurgical results for meningioma (in which 77% of 206 tumors were located at the cranial base), the median tumor margin dose was 16 Gy and survival rates at 5 and 7 years were 94% and 92%, respectively.31 The overall tumor control rate was 89% at 5 years, with 56% of tumors decreasing in size. Taken together, the available data relating intracranial meningiomas (with the endpoint being freedom from progression after radiosurgery) indicate that tumor control appears to be in the range of 90%, with tumor shrinkage noted in approximately one third of radiosurgical patients.
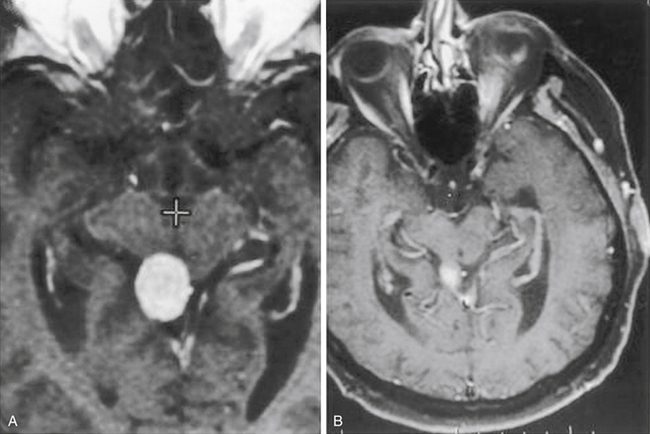
Meningiomas in the posterior fossa often require radiation as either adjuvant or primary therapy. The radiosurgical experiences for acoustic and other schwannomas, as well as those for various benign and malignant tumors, have provided an important database regarding the responses of the cranial nerves and brain stem. For practical purposes, most cranial nerves are tolerant to radiosurgical doses up to 16 Gy, whereas the optic nerves, chiasm, and tracts seem more sensitive; for these, lower doses up to 10 Gy seem reasonable.32 The radiosurgical response may vary depending on the length of nerve irradiated; the microenvironment of the nerve (e.g., ischemia), the degree of compression by the tumor, prior surgery and radiotherapy effects, retreatment and treatment intervals, and additional host factors33,34 (Fig. 42-5). Motor morbidity rates appear to be less than 5%. However, the assessment of sensory nerve function poses more difficult problems, depending on the tumor type and location. For example, whereas the radiosurgical impact on cochlear nerve function may be less significant when dealing with meningiomas, radiosurgical dosing for acoustic neuroma has undergone a gradual decrease, possibly as a result of the intimate relation of tumor to nerve. One recent report on 55 patients with skull base meningiomas (including three of the petrous apex, four of the tentorium, two of the clivus, five of the CPA, and three of the jugular foramen), with average follow-up of 48.4 months, noted tumor stabilization in 69%, shrinkage in 29%, and enlargement in 2%.35 Mean tumor volume was 7.33 cm3, and doses ranged from 12 to 25 Gy. All complications were transient, including seven trigeminal pareses and three patients with diplopia. Radiosurgical data on 62 patients with petroclival meningiomas treated with tumor margin doses of 11 to 20 Gy documented tumor shrinkage in 23%, stabilization in 68%, and growth in 8%.36 Median follow-up was 37 months.
For tumor residuals intimately attached to the dural sinuses, similar principles apply. Based on the current literature, it is reasonable to use radiosurgery for a tumor located adjacent to or inside a dural sinus. There does not appear to be increased risk of weakening of the walls of the sinus, venous infarction, or other vascular-related complications, and it seems unlikely that radiosurgery will lead to progressive sinus occlusion. Larger experience and longer-term follow-up are needed to confirm these findings.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree