Chapter 159 Surgical Techniques in the Management of Thoracic Disc Herniations
The initial use of laminectomy to treat herniated thoracic discs was met with uniformly unacceptable results.1,2 As a result, numerous methods have been developed to treat thoracic disc herniations. Unfortunately, no standard algorithm exists to aid the surgeon in selecting the best procedure for a given patient. Each technique offers a combination of advantages and compromises that needs to be evaluated for each patient. Despite the relatively low prevalence of symptomatic thoracic herniated discs, any surgeon managing a moderate proportion of spinal disease in his or her practice will invariably be confronted with this condition. Therefore, a basic understanding of the available surgical options and the indications and limitations of each procedure is vital.
Important Concepts
• Thoracic disc herniations, although uncommon, are encountered by spine surgeons.
• Laminectomy is an unacceptable treatment for thoracic disc herniations.
• Posterior techniques include the transpedicular, Stillerman’s transfacet pedicle sparing, transcostovertebral, costotransversectomy, and lateral extracavitary.
• Posterior approaches are generally favored in cases of more lateral, noncalcified, extradural disc herniations.
• Anterior approaches include the transthoracic, retropleural, and transsternal.
• Anterior techniques offer better ventral exposure for discs that are centrally located, calcified, and/or intradural.
• Complication rates for the common posterior and anterior procedures are similar.
Thoracic disc herniations account for a minority of the disc herniations evaluated by a spine surgeon. This reflects the relative immobility of the thoracic spine as compared with the cervical and lumbar regions and thus the low incidence of degenerative changes. Contemporary series suggest that thoracic herniated discs represent less than 1% of all symptomatic discs and, accordingly, represent less than 1% of all disc operations.1 This establishes an incidence of 1 symptomatic patient per 1 million individuals per year.2–4
The majority of thoracic herniated discs are asymptomatic. As many as 37% of patients harbor an asymptomatic herniated thoracic disc as defined on randomly sampled magnetic resonance imaging (MRI) scans.5 More conservative estimates propose this number lies in the range of 10% to 15%.1,6,7
The majority of symptomatic discs are found in the lower third of the thoracic region, with most being found between the T8 and T11 levels.1,7 Discs in the upper third of the thoracic spine are rare. Herniated discs in the thoracic spine commonly occur centrally within the canal (77% to 94%) and are often calcified (22% to 65%).1,8 A small but very important 6% to 7% of discs prove to be intradural.9
Symptomatic thoracic herniated discs manifest with a wide array of findings. Stillerman and colleagues8 presented an exhaustive review of their personal findings in 71 patients with thoracic disc disease as well as a meta-analysis of 13 series encompassing 247 patients (Table 159-1). Both of these surveys demonstrated that sensory changes were seen in more than 60% of cases. Pain was a finding in greater than half of the patients but was actually more likely to be axial than the typically presumed radicular pattern. Motor weakness and spasticity or hyperreflexia were present in 55% to 58% of patients. As with many cervicothoracic lesions, bowel and bladder dysfunction was one of the least-common symptoms, appearing in only 24% to 35% of patients.8
Table 159-1 Comparison of the Present Study and Earlier Thoracic Disc Series
| Factor | 13 Contemporary Series (1986-1997) | Present Study |
|---|---|---|
| Demographics and Disc Characteristics | ||
| No. of patients/no. of discs | 247/263 | 71/82 |
| Sex (F/M) | 112/95 (1.18/1) | 37/34 (1.09/1) |
| Age, yr | 18-79 | 19-75 |
| Trauma | 37% (59/161) | 37% (26/71) |
| Levels (total) | T1-L1 (244) | T4-L1 (82) |
| Level/frequency (no.) | T8-9: 17% (41) | T9-10: 26% (21) |
| T11-12: 16% (39) | T8-9: 23% (19) | |
| T10-11: 11% (26) | T10-11: 17% (14) | |
| Calcified | 22% (33/151) | 65 % (53/82) |
| Intradural | 6% (5/90) | 7% (6/82) |
| Canal location | ||
| Central/centrolateral | 77% (113/146) | 94% 77/82) |
| Lateral | 23% (33/146) | 6% (5/82) |
| Multiple discs | 8% (20/242) | 14% (10/71) |
| Presenting Signs and Symptoms | ||
| Localized/axial pain | 56% (111-199) | 61% (43/71) |
| Radicular pain | 51% (94/185) | 16% (11/71) |
| Sensory deficit | 64% (145/226) | 61% (43/71) |
| Bowel/bladder deficit | 35% (72/208) | 24% (17/71) |
| Motor impairment | 55% (114/208) | 61% (43/71) |
| Results∗ | ||
| Pain/total | 76% (106/140) | 87% (47/54) |
| Localized/axial | 80% (39/49) | 86% (37/43) |
| Radicular | 74% (29/39) | 91% (10/11) |
| Sensory deficit | NR | 84% (36/43) |
| Bowel/bladder deficit | 80% (47/59) | 77% (13/17) |
| Motor impairment | 69% (65/94) | 58% (25/43) |
NR, not reported.
∗ Number resolved or improved/total number of patients in groups reporting this result.
From Stillerman CB, Chen TC, Couldwell WT, et al: Experience in the surgical management of 82 symptomatic herniated thoracic discs and review of the literature. J Neurosurg 88:623-633, 1998.
The radiographic identification of these lesions is obviously most commonly performed with MRI. MRI allows visualization of the disc herniation and the surrounding neural elements (Fig. 159-1). However, computed tomography/myelography remains a viable imaging technique with excellent resolution of the affected region, despite the inconvenience and invasiveness of the procedure. Plain computed tomography scanning also serves a supportive role because it often assists MRI in evaluating whether a given disc is calcified and offers a better analysis of the bony anatomy (Fig. 159-2).

FIGURE 159-1 Sagittal T2-weighted magnetic resonance imaging demonstrates a thoracic herniated disc and associated syrinx.

FIGURE 159-2 Axial computed tomography scan of same patient demonstrates calcification of the herniated disc.
Selecting patients for surgery is much like selection for degenerative processes afflicting the remainder of the spine. That is, the indications for surgery are by no means objectified and established but rather are physician defined. As with most cervical lesions, myelopathy with or without bowel or bladder involvement is a nearly absolute operative indication. Surgical treatment of thoracic herniated discs for radiculopathy, back pain, or sensory changes is much more difficult to uniformly define. The natural history of thoracic disc herniations is not completely understood. Brown and colleagues10 followed 40 patients with symptomatic thoracic disc herniations and determined that 77% returned to work symptom free without surgical intervention. Therefore, an argument can be made to manage patients who do not have significant neurologic insult (weakness, spasticity) in a fashion similar to those with degenerative cervical and lumbar conditions. These nonoperative measures can include a combination of rest, physical therapy, oral antiinflammatory medication (steroidal and/or nonsteroidal), and/or steroid injections.
One of the reasons for the development of this variety of procedures is the surgical constraint of the thoracic spine anatomy. In this region, the spinal cord lies within the relatively narrow thoracic spinal canal and the thecal sac cannot be manipulated as freely as within the lumbar region. Therefore, the operative approach needs to minimize manipulation of the dura and spinal cord. Although this feature is similar to the cervical region, the anterior approaches to the thoracic region (excluding the very superior thoracic spine) are more involved than standard anterior cervical procedures. Thus the ideal procedure would afford the surgeon a ventral view of the region while maintaining the more straightforward technical aspect of a posterior approach. As a result of these requirements, more-aggressive posterior procedures have been developed in attempts to gain greater “anterior” perspectives and circumvent the need for more-involved anterior thoracic exposures.
Considerations for an operative approach for herniated thoracic discs include the following:
• Mediolateral localization of the herniation (location with respect to canal and cord and the foramen and root and the resultant symptoms)
• Complicating factors of the disc itself (intradural, calcification)
• Presence of multiple disc herniations
Although not inclusive, the following guidelines can be made in terms of operative approaches.
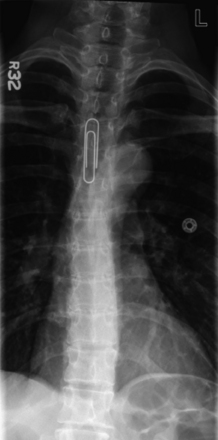
Intraoperative Localization
First, a surgeon needs to identify the level of a herniated disc using the same method by which the preoperative level is identified. That is, if the preoperative investigations identify the affected thoracic level counting down from C1, then the surgeon should not necessarily use the sacrum as a reference point intraoperatively, because a lumbarized sacral segment could obviously cause an error in localization. Rather, the surgeon can employ an intraoperative anteroposterior (AP) radiograph and count down from the first thoracic ribs, or the sacrum can be used to count upward, if this has been confirmed as an accurate means of reference. A preoperative localization can be easily performed by taping a radiopaque marker to the patient and obtaining a standard AP radiograph (Fig. 159-3).
Description of Individual Procedures
Posterior Procedures
Transpedicular
The transpedicular approach is perhaps the most commonly considered procedure for a thoracic disc herniation. Its origins date to the initial description of Patterson and Arbit11 in 1978, which represent a modification of Carson’s12 1971 technique. The transpedicular approach allows the surgeon relatively straightforward access into the most lateral region of the spinal canal ventral to the spinal cord (Fig. 159-4). The patient is placed in a prone position on gel rolls or a Wilson frame, and a vertical midline incision is centered over the level of interest. Sharp dissection is carried deeply to the thoracodorsal fascia. A unilateral exposure can be performed to minimize trauma to the contralateral paravertebral musculature. Once through the thoracodorsal fascia, a subperiosteal dissection is performed with Cobb elevators until the lateral facets are exposed on the affected side.
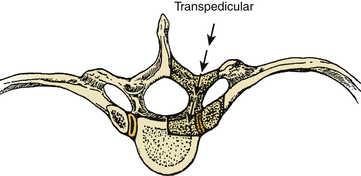
FIGURE 159-4 Schematic demonstrates the region of bone removal in the transpedicular approach.
(From Fessler RG, Sturgill M: Review: Complications of surgery for thoracic disc disease. Surg Neurol 49:609-618, 1998.)
Viewing the facet joints, the surgeon needs to then develop an idea as to the location of the pedicle and the associated nerve root. The thoracic pedicle to be drilled is centered 1 to 2 mm beneath the edge of the inferior facet of the superior vertebra (Fig. 159-5). For example, a for a T7–8 disc herniation the surgeon will aim to drill the T8 pedicle, which is centered just below the inferior edge of the T7 inferior facet.
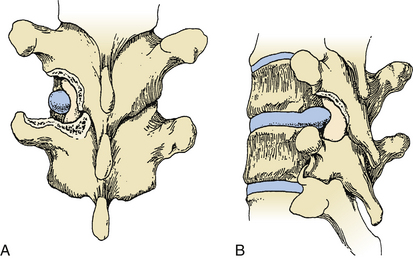
FIGURE 159-5 Transpedicular approach after drilling of facet and superior pedicle.
(From Kumar R, Dunsker SB: Surgical management of thoracic disc herniations. In Schmidek HH, Sweet WH (eds): Operative Neurosurgical Techniques, 4th ed. New York: WB Saunders, 2000, pp 2122-2131.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree