and Colin L. W. Driscoll2
(1)
Department of Otolaryngology – Head and Neck Surgery, Stanford University, Stanford, CA, USA
(2)
Department of Otorhinolaryngology, Mayo Medical School, Rochester, MN, USA
Repair of Temporal Lobe Encephalocele
Concept
Defects in the bone of the temporal floor (the tegmen) are repaired.
Conditions treated
CSF leak from the middle cranial fossa into the temporal bone
Temporal lobe meningocele or encephalocele
Risks
Injury to the temporal lobe such as contusion, edema, or vascular compromise
Temporal lobe seizure
Aphasia
Hearing loss and dizziness if the labyrinth is violated
Facial nerve injury, typically if the geniculate ganglion is dehiscent and not recognized
Dry eye if the greater superficial petrosal nerve is transected
Recurrence of disease
Meningitis
Benefits
Direct and wide exposure of the defect(s) or pathology.
Placing a vascularized muscle flap between the brain and the ear reduces the recurrence risk.
Additional notes
Small defects (<1 cm2), especially those located more lateral and posterior, can usually be repaired from below via a mastoidectomy. Most commonly, these are from iatrogenic injury. Typically, a cartilage graft can be squeezed through the bony opening and placed between the dura and the tegmen bone. The approach described here is for larger defects, multiple defects, and those located more anterior or medial.
In our opinion, patients with a chronic CSF leak preoperatively should be treated with lumbar subarachnoid drainage for 3–4 days postoperatively. This is because their CSF production has increased to compensate for the leak. Suddenly stopping the leak can lead to elevated intracranial pressure, which will predispose the repair to failure. This is not necessary for patients without a CSF leak or for those who are being treated for an acute-onset CSF leak.
If the amount of brain herniation into the mastoid and middle ear is relatively small, the entire procedure can be done through the middle fossa portion alone. A mastoidectomy may not be needed.
Spontaneous CSF leaks have become more common along with the rise in obesity. There are often multiple defects, and therefore, we repair all of these through a middle fossa craniotomy. This allows us to lay tissue and bone broadly across the floor. Even with some small solitary defects or encephaloceles, we often prefer to work from above. It is easier to be confident of graft placement and hemostasis. Working from below, pushing material up through a defect is less precise, and there is the potential to cause bleeding that cannot be seen.
Many patients use CPAP to treat obstructive sleep apnea, and deciding when to allow them to resume this is unclear. We know that the middle ear pressure is increased when using CPAP, thus there is a risk of pneumocephalus. The risks of oxygen desaturation and tension pneumocephalus must be assessed. While this varies on a patient-by-patient basis, it is nice when CPAP use can be held for at least 7 days after surgery. This typically requires a monitored bed in the hospital, however.
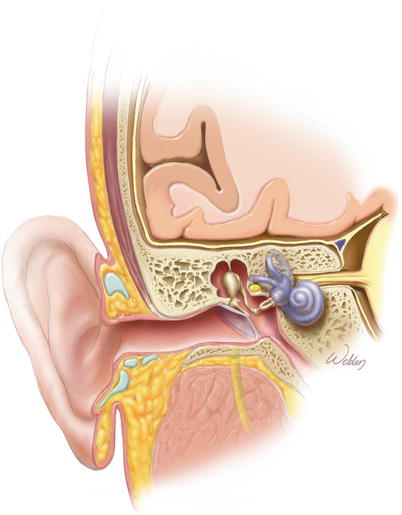
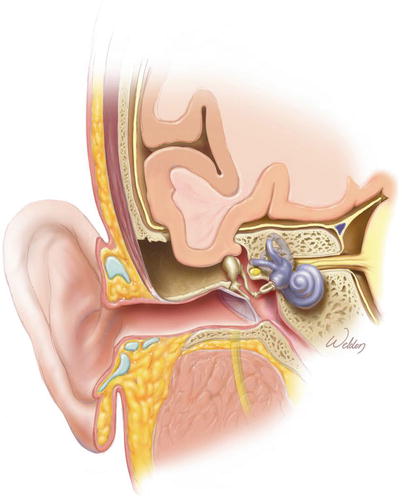
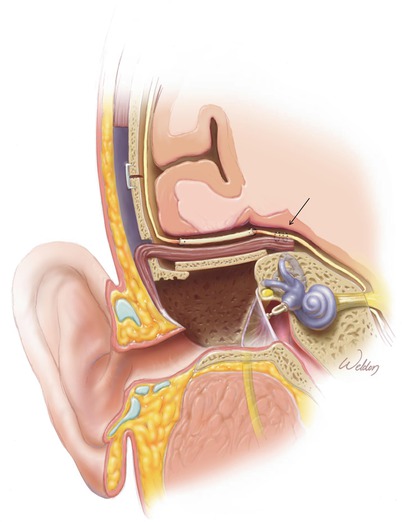
1.
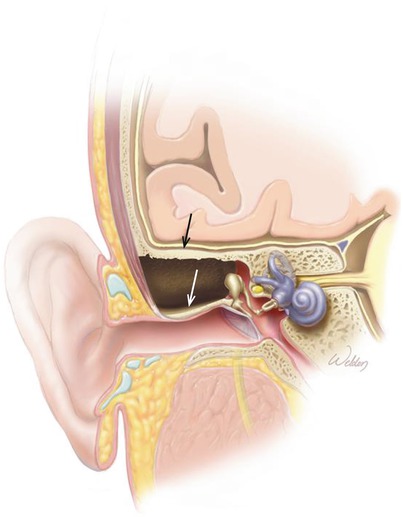
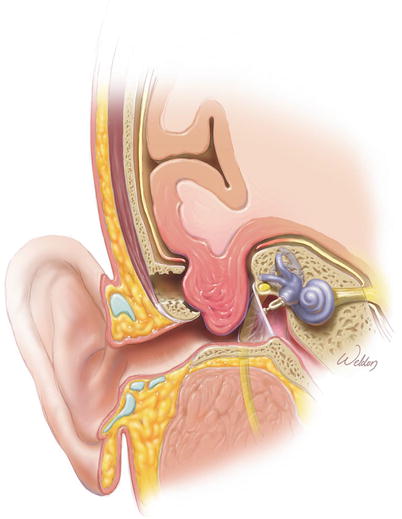
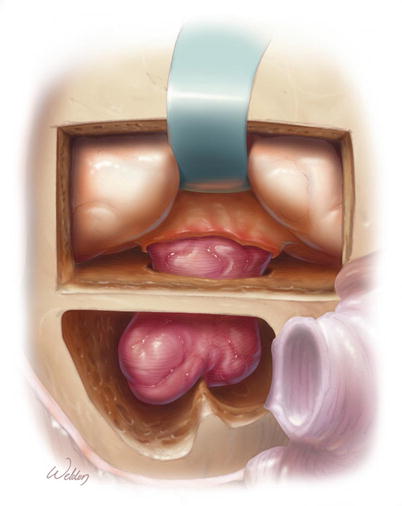
Normal coronal view of the temporal bone.
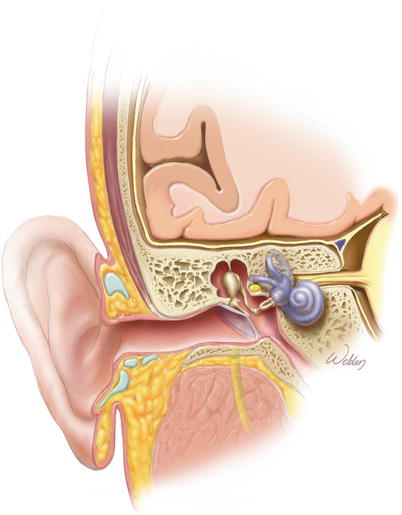
2.
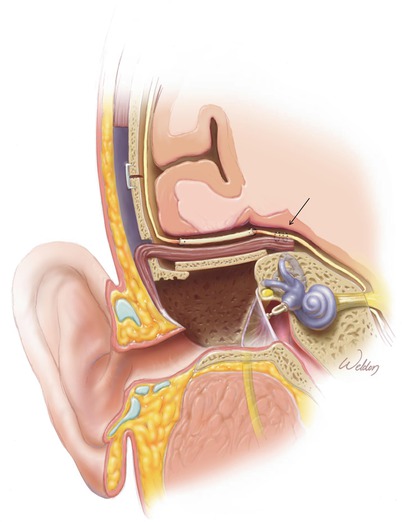
Proper postoperative appearance of a canal wall up mastoidectomy. Note that the tegmen (black arrow) and the posterior–superior ear canal are intact (white arrow).
3.
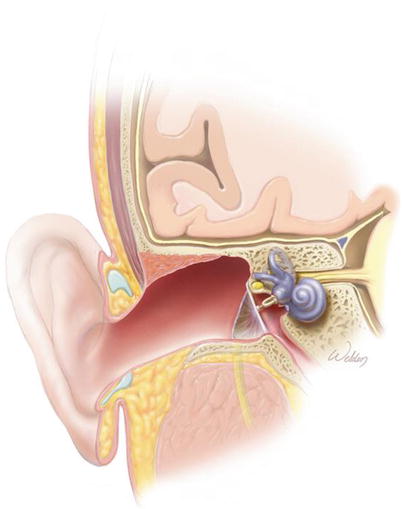
Proper postoperative appearance of a canal wall down mastoidectomy. In this case, the tegmen is intact, but the tympanic membrane lies across the horizontal and vertical portions of the facial nerve because the ear canal has been removed. There is also a large meatoplasty, and the ear canal slopes downward to promote healthy drainage.
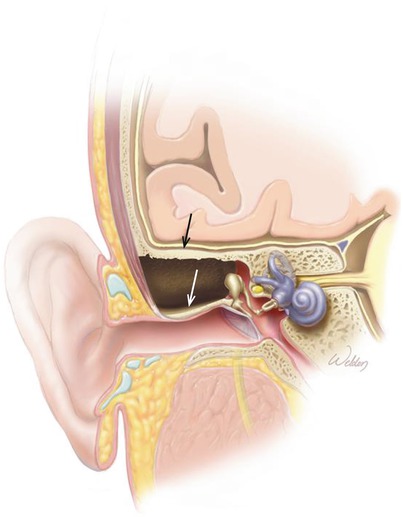
4.
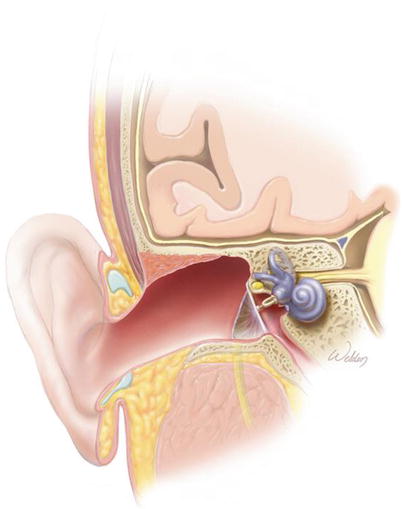
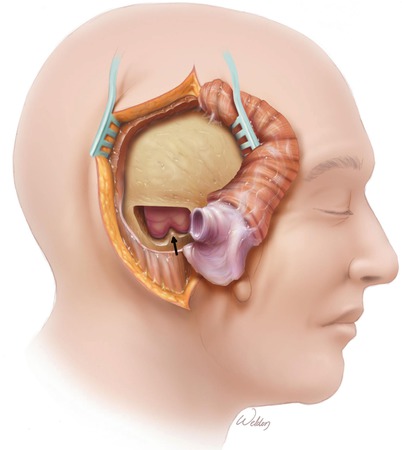
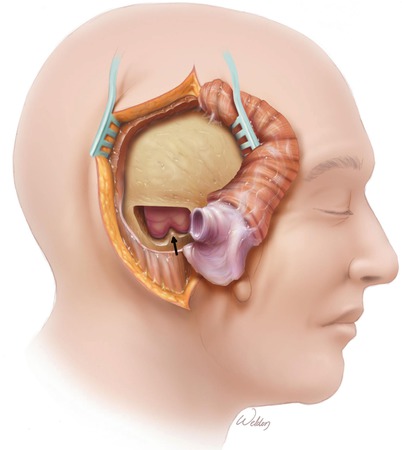
Inadvertent injury to the tegmen, and possibly also the dura, can lead to a temporal lobe encephalocele. This may not occur immediately after surgery but even years later. This image depicts an encephalocele into a canal wall up mastoidectomy.
While CSF, or even brain, may be appreciated behind the tympanic membrane, often the only sign is a visible pulsing of the eardrum that synchronizes to the patient’s heartbeat. This reflects transmitted brain pulsations to the middle ear and mastoid air space. It can be noted both with binocular microscopy and on tympanometry when the patient is sitting upright. This sign usually resolves when the patient is laid flat so that the brain does not exert as much downward pressure.
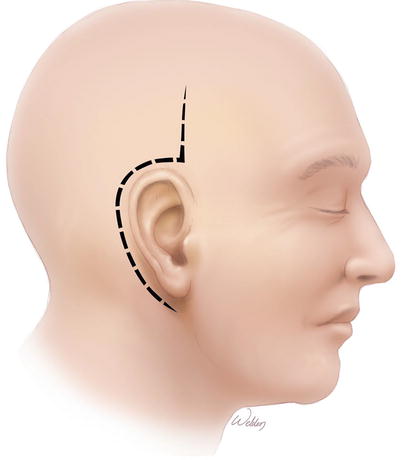
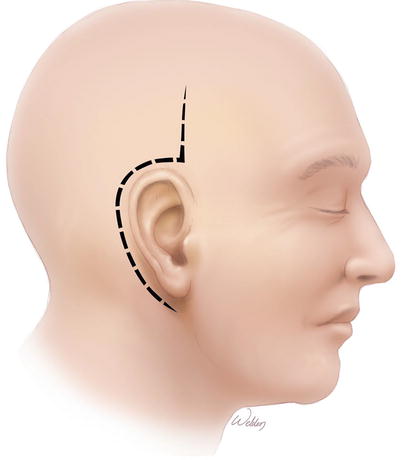
5.
Treatment for an encephalocele is surgical. The incision is a standard postauricular incision that extends superiorly.
6.
The temporalis is exposed superiorly and the sternocleidomastoid muscle attachment to the mastoid process exposed inferiorly. The periosteum over the mastoid process is elevated to the ear canal.
7.
The temporalis muscle is then retracted off the skull anteriorly. A standard cortical mastoidectomy performed to expose the encephalocele (asterisk). For a small encephalocele, particularly those in patients that have never had mastoid surgery before, a mastoidectomy does not need to be performed as the encephalocele can be treated through a middle fossa craniotomy alone.
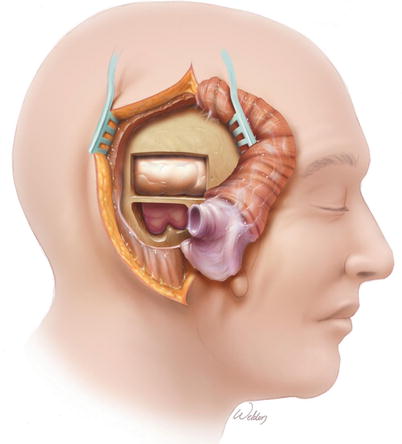
8.
A middle fossa craniotomy is performed. This can be centered over the area of the encephalocele identified by preoperative imaging to allow it to be quite small. Details of this opening are given in Chap. 3.
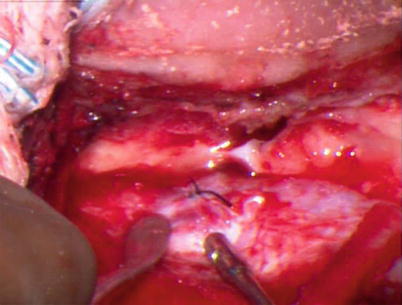
9.
Extradural dissection with a periosteal elevator is performed to trace around the circumference of the dural defect.
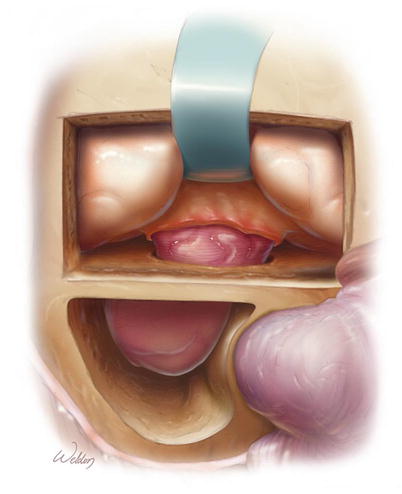
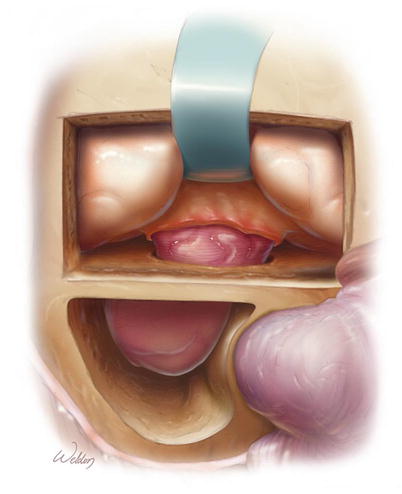
10.
Large, plunging encephaloceles do not contain viable brain. A bipolar cautery is used to carefully divide the devitalized brain below from the healthy brain above. After this process, the healthy brain typically retracts up, and it is important not to lose track of any bleeding vessels when this happens. Meticulous hemostasis inside the dura is necessary.
11.
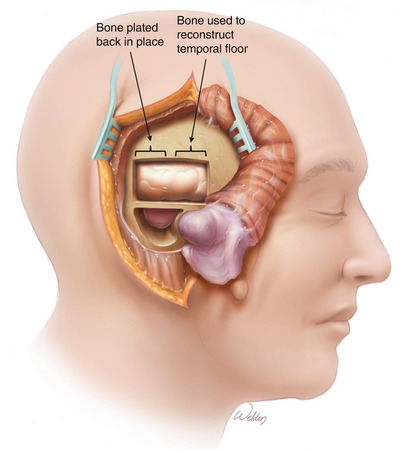
A three-layer closure is performed. The superior layer is a dural patch consisting of fascia, cadaveric dura, or artificial dura (i.e., Duragen). A larger piece than one expects to use is carefully inserted through the dural defect and the edges tucked up between the brain and the dura. Thus, the downward pressure of the brain when the patient is upright will help seal the defect. We usually cover this with a dural sealant as well (i.e., Tisseal or Duraseal).
The inferior layer is the bone graft. The bone flap removed during the craniectomy is cut and a portion of it used to bridge the bony defect in the tegmen. Usually, we cut the anterior half off and use it to reconstruct the tegmen. It is important to make sure it is laid on top of the medial edge of the defect for support. Sometimes, it is hard for the bone graft to stay in the appropriate location. In this case, it can be plated to the skull to prevent lateral migration.
Finally, the posterior half of the temporalis muscle is separated from the anterior half vertically and then rotated between the dural patch and the bone graft to form the middle layer. This should be sutured to a hole drilled in the skull or to the soft tissue around the ear canal to prevent the muscle from retracting out when the patient wakes up and begins to chew.
There are multiple ways to layer in your choice of tissues that are all likely to be successful. We like to put an intradural patch in those patients with multiple defects and very atrophic dura. An incision can be made over the lateral aspect of the temporal lobe and medial dissection performed intradurally. This allows us to place a large graft, essentially covering the whole floor.
Finally, the remaining bone flap is plated back to cover the craniotomy site. It is most important to cover the posterior portion of the defect as the temporalis muscle flap enters the middle fossa through the anterior portion and will provide adequate bulk to prevent trauma should the patient be bumped in the side of the head postoperatively.
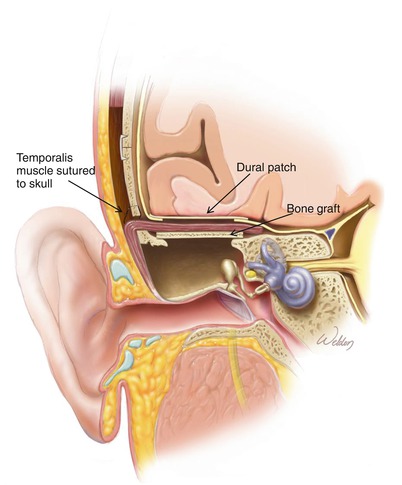
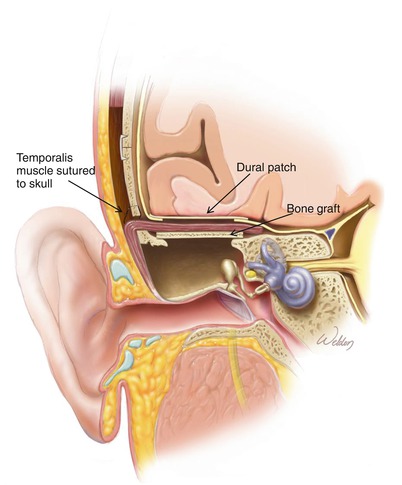
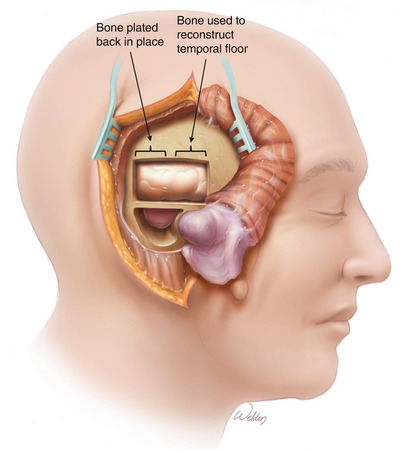
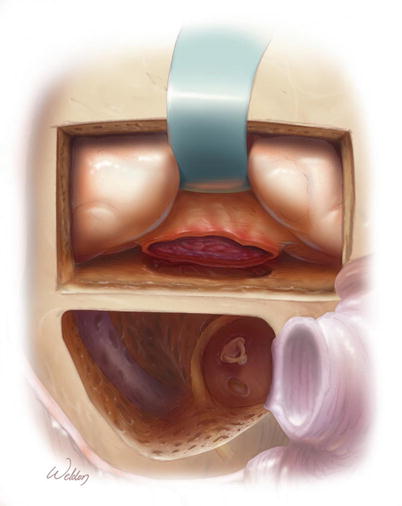
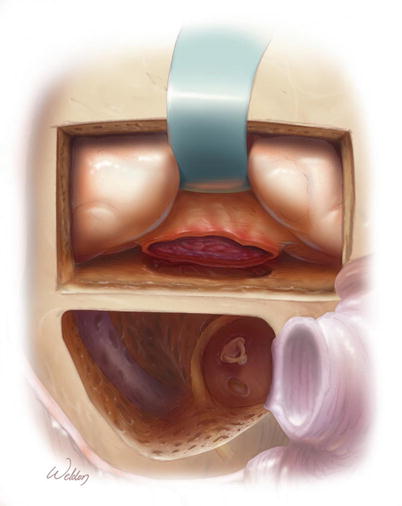
12.
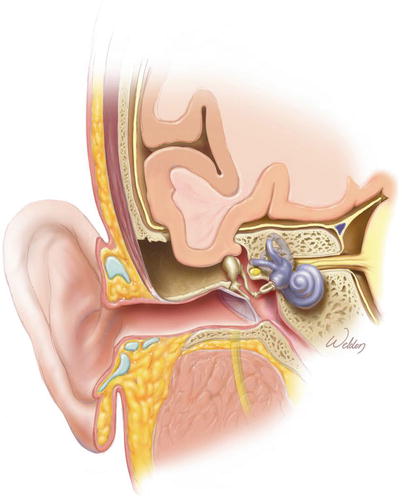
Diagram of a temporal lobe encephalocele into a canal wall down mastoidectomy. This is even more concerning than the canal wall up situation because the brain is directly exposed to the outside environment.
In some cases, the skin of the cavity overlying the encephalocele is thick, and the repair can be done from above without violating the cavity. When this skin can be kept intact, the risk of post-op CSF leak is reduced, and the risk of infection may be less.
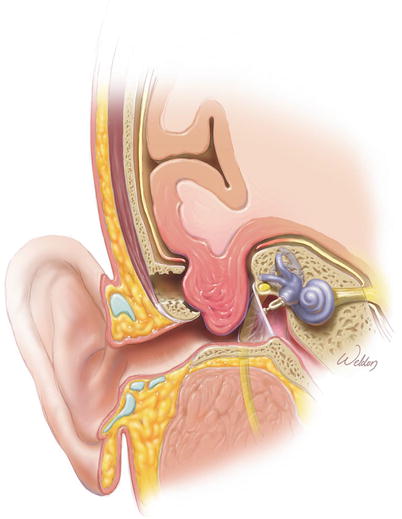
13.
In other cases, the mastoid and middle fossa must both be opened up. The same incision can be used as for the canal wall up procedure.
14.
Exposure of the temporalis muscle.
15.
The mastoidectomy defect is opened. The facial ridge can be seen to be too high in this illustration (arrow). The anterior ear canal skin is left tethered to provide a vascular supply to the tympanic membrane.
17.
The dural defect is exposed circumferentially.
18.
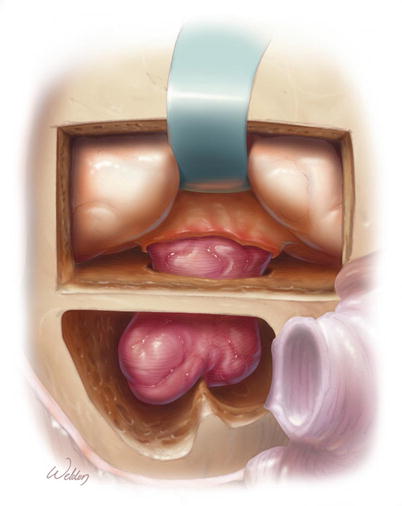
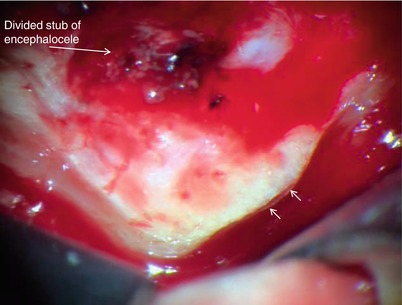
The encephalocele is divided and the facial ridge lowered.
19.
A three-layered closure is performed as described above. In this illustration, an alternative technique for suturing the tip of the temporalis muscle to the medial dura is shown (arrow). This technique, while challenging, is probably more secure than suturing the base of the muscle flap. Once the first stitch is tied down, it is impossible to get any more placed. Thus, two or three stitches should be thrown and then cinched down together using your assistant to help.
The tympanic membrane may also need to be reconstructed using temporalis fascia and/or cartilage using routine otologic techniques. Ossicular chain reconstruction can be performed if desired (not shown).
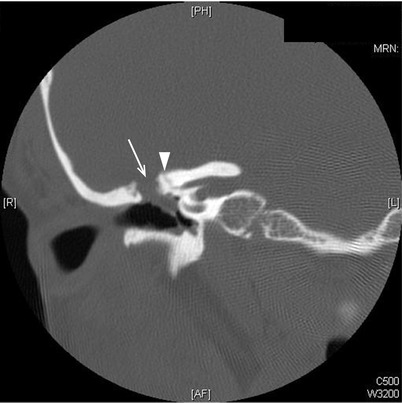
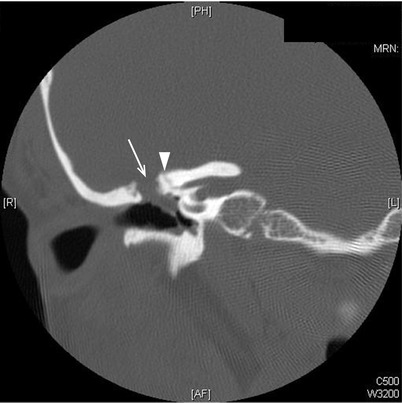
20.
Case 1. Coronal CT of a patient with an idiopathic right temporal lobe encephalocele (arrow). She presented with CSF rhinorrhea and conductive hearing loss. Also, note the superior semicircular canal dehiscence (arrowhead), which is often found in patients with this condition.
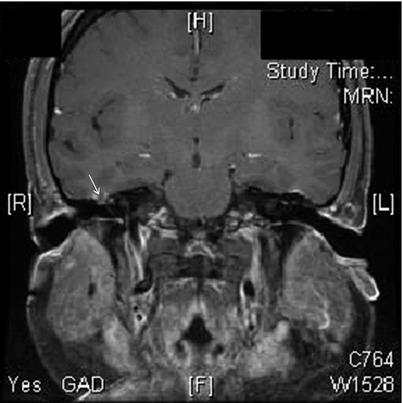
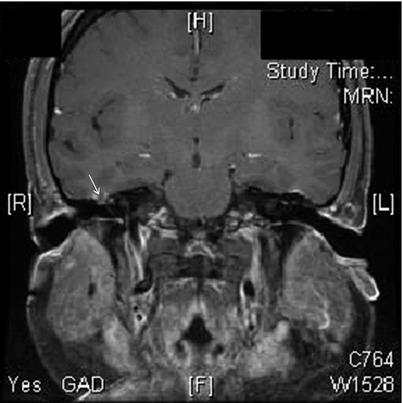
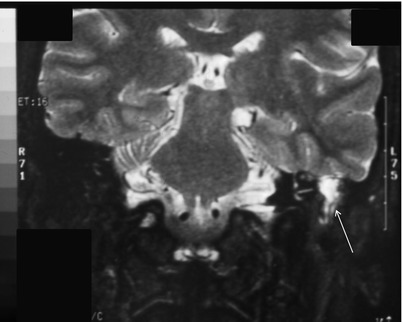
21.
Coronal MRI demonstrates a very small encephalocele (arrow) on the left side.
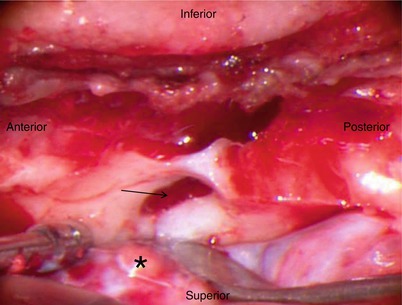
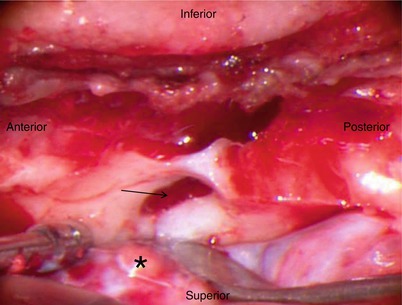
22.
Only a middle fossa craniotomy was needed to reduce the encephalocele and repair this small skull base defect. Here, the surgeon is sitting at the head of the patient, and the temporal lobe is retracted by the malleable retractor in an extradural fashion. However, the small encephalocele is visible to the left of the retractor (asterisk). The defect in the temporal floor is clearly seen (arrow).
23.
The encephalocele was reduced and the dura closed with a suture.
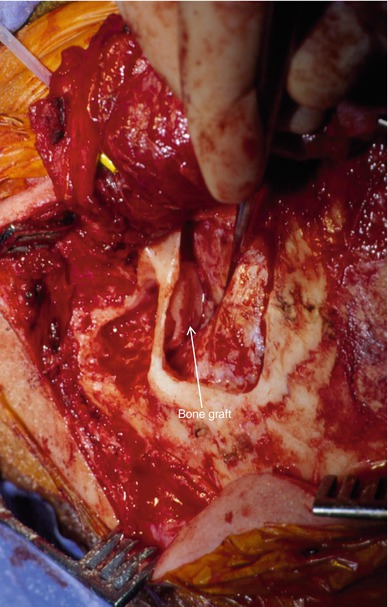
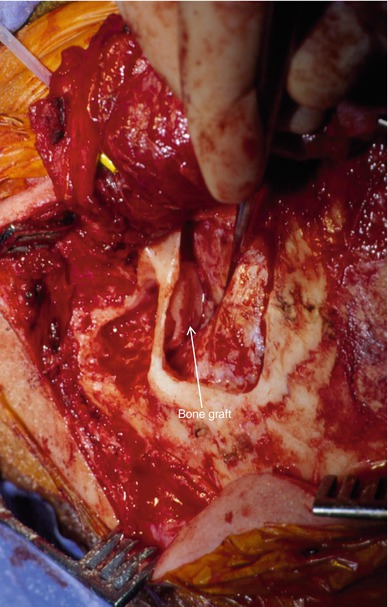
24.
A bone graft was inset to cover the defect. This was the anterior half of the bone flap harvested during the craniotomy.
25.
The posterior half of the temporalis muscle was then swung in between the bone and the dura (edges outlined by arrows) and the posterior half of the bone flap plated. The temporalis muscle bulk protects the anterior half of the craniotomy site where there is no bone. The temporalis muscle was sutured to the bone flap to hold it in position.
26.
Case 2. Coronal CT scan demonstrates a larger left temporal lobe encephalocele (arrow).
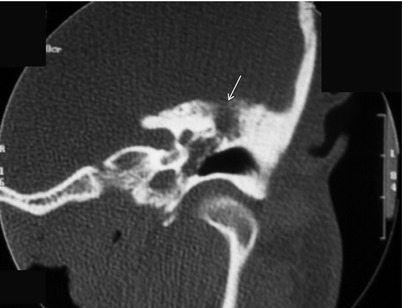
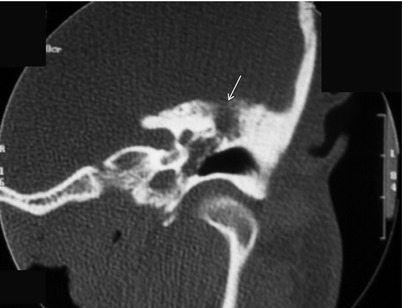
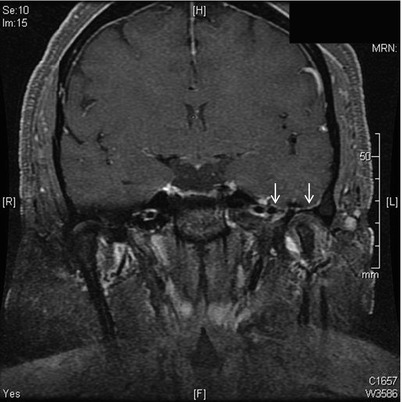
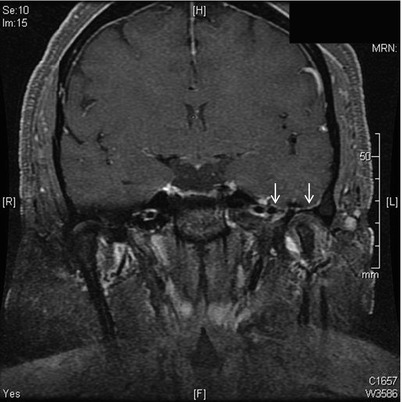
27.
T2 coronal MRI demonstrates CSF penetration into the mastoid cavity (arrow).
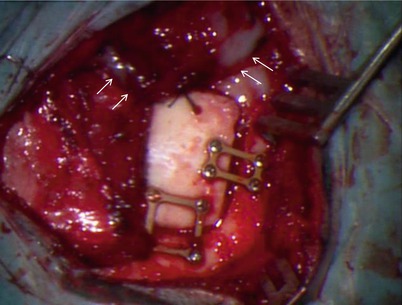
28.
A mastoidectomy and middle fossa craniotomy were performed. The encephalocele was identified and resected using the bipolar to cauterize across the neck of the devitalized brain at the level of the tegmen and then dividing it with a microscissors. This revealed the defect in the temporal floor (tegmen; arrow).
29.
The temporal lobe was elevated and a bone graft inset to cover the defect.
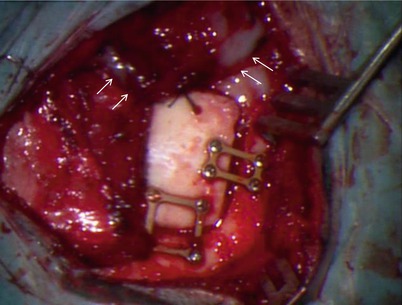
30.
Because of the size of the defect and because the bone graft did not remain in a stable position, a titanium plate was used to fix the bone graft securely.
31.
The posterior third of the temporalis muscle was then separated from the anterior portion of the muscle for use as a vascularized flap. It is being held up by the forceps.
32.
After insetting the flap through the inferior aspect of the craniectomy, the remaining bone was plated back. Because we needed a larger bone graft than typical, we used a piece of mesh in this case to cover most of the defect.
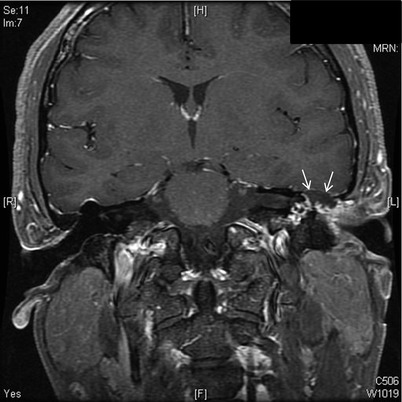
33.
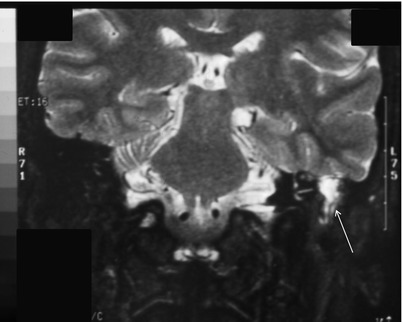
Case 3. A large meningocele protruding into the left mastoid (arrows). This patient presented with recurrent meningitis. The inflammation of the mastoid can be noted at the enhancement within the mastoid air cells on this coronal T1 MRI with gadolinium.
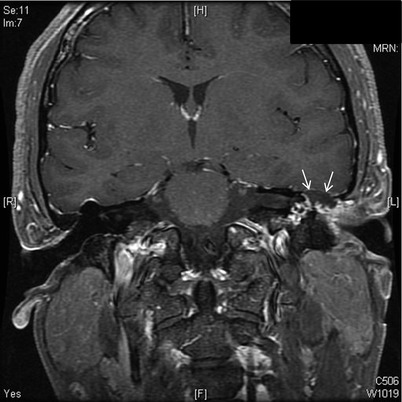
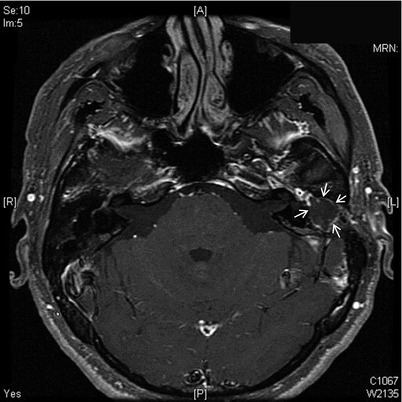
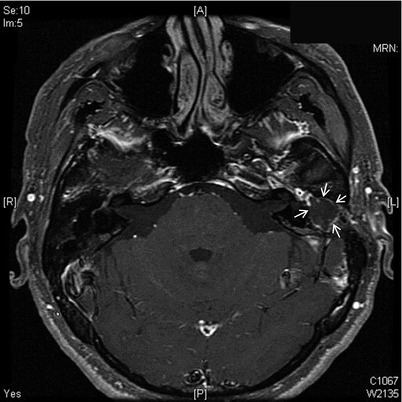
34.
Axial view of the same patient demonstrating the large circular meningocele in the mastoid antrum (arrows). Surgical repair was performed using only a middle fossa approach.
35.
Case 4. A patient presenting with CSF rhinorrhea. Axial T2 MRI demonstrated that the mastoid, middle ear, and petrous apex were filled with fluid.
36.
Coronal T1 MRI with gadolinium from the same patient demonstrates that the left temporal lobe was lower than the right temporal lobe. Also, the lining of the dura was inflamed (arrows).
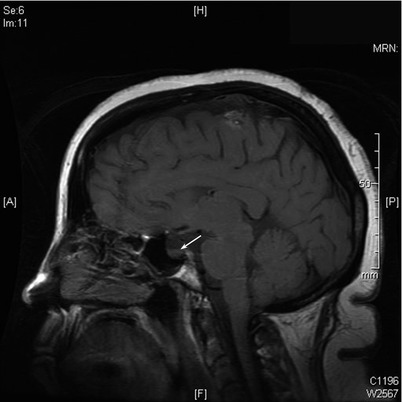
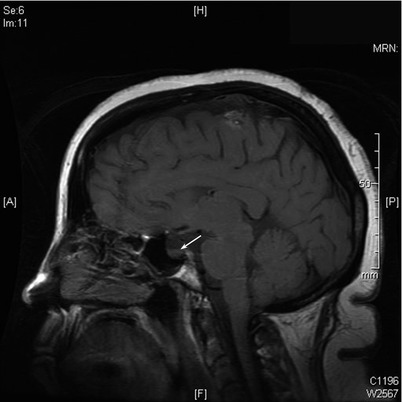
37.
Sagittal T1 MRI from the same patient demonstrates flattening of the pituitary gland (arrow). This “empty sella” sign suggests the patient has intracranial hypertension and is often found in patients with idiopathic spontaneous temporal lobe encephalocele or CSF leak. A neuro-ophthalmology consult should be obtained to look for ocular manifestations of increased intracranial pressure.
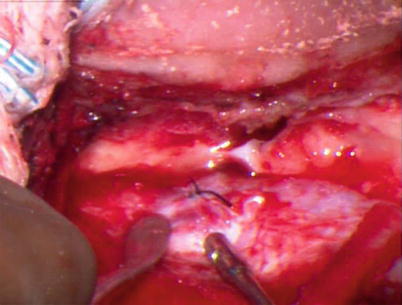
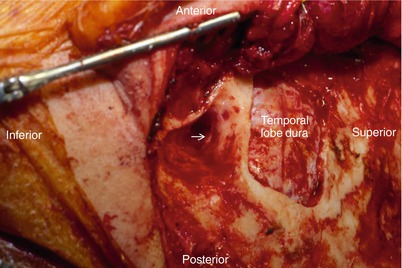
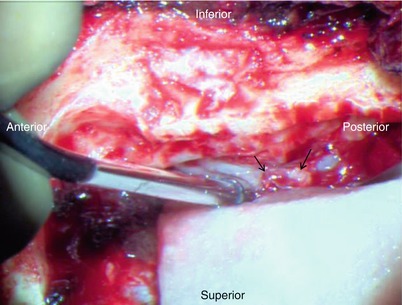
38.
Case 5. Intraoperative photos from a patient with a right temporal lobe encephalocele into the middle ear causing conductive hearing loss. Because it was relatively small, only the middle fossa portion of the procedure needed to be performed. After performing a craniotomy, the temporal lobe dura was retracted superiorly by a malleable. The herniated brain is seen (arrows).
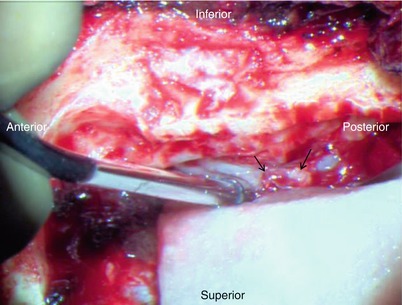
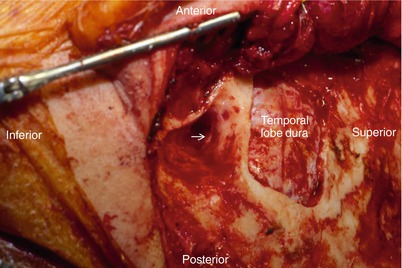
39.
The encephalocele was divided at its neck and dissection continued medially. This patient also had superior semicircular canal dehiscence (the groove at the dome of the arcuate eminence; arrows).
40.
The encephalocele was microdissected out of the middle ear.
41.
Removal of the encephalocele. Note that several patches of missing bone were connected together to improve access.
42.
After removal of the encephalocele.
43.
A piece of the bone flap was plated in place. Some pieces of Gelfoam were placed under the bone flap to help seal around the edges.
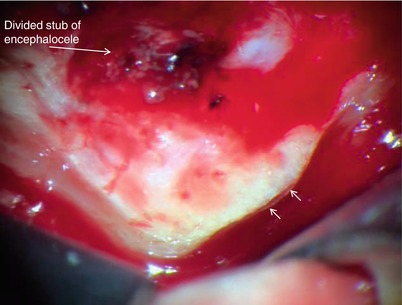
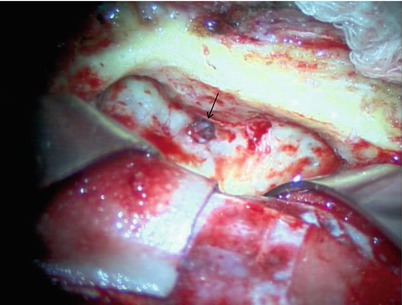
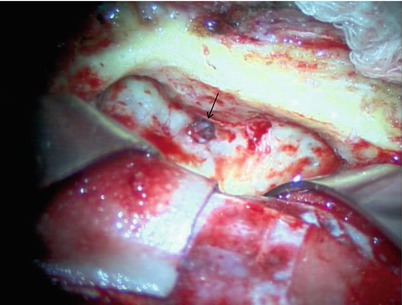
44.
Case 6. A small right idiopathic temporal lobe encephalocele removed via the middle fossa approach. The craniotomy has been performed, the dura of the temporal lobe elevated, and the encephalocele truncated at its neck. The defect filled with the encephalocele is visible (arrow).
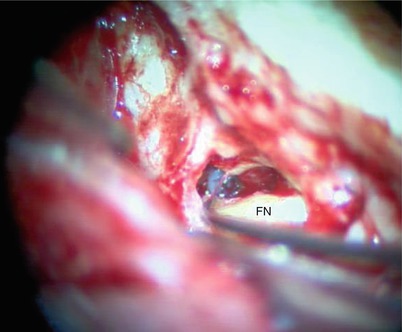
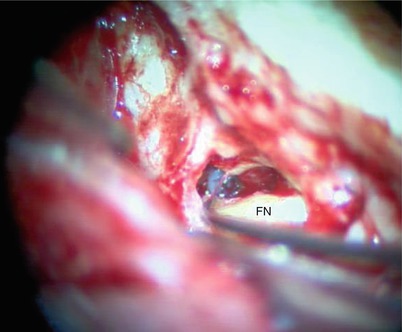
45.
Microdissecting the encephalocele off the ossicular chain with a Rosen needle. The bony sheath covering the horizontal facial nerve is seen (FN).
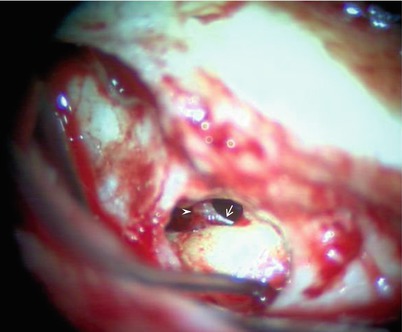
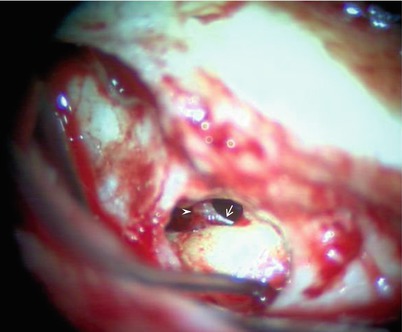
46.
After removing the encephalocele, the stapedial tendon (arrow) and the incudostapedial joint (arrowhead) are visible.
Repair of Superior Semicircular Canal Dehiscence
Concept
Erosion of the bone of the temporal floor into the superior semicircular canal. This creates a “third window” whereby loud sounds evoke vertigo when the sound pressure wave passes through the vestibular system.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree