and Colin L. W. Driscoll2
(1)
Department of Otolaryngology – Head and Neck Surgery, Stanford University, Stanford, CA, USA
(2)
Department of Otorhinolaryngology, Mayo Medical School, Rochester, MN, USA
Simple Mastoidectomy for Acute Mastoiditis
Concept
A simple mastoidectomy with myringotomy and placement of a pressure equalization tube drains purulence from both the mastoid and the middle ear.
Conditions treated
Acute coalescent mastoiditis
Acute mastoiditis with a subperiosteal abscess
Risks
Hearing loss
Facial nerve injury
Benefits
While myringotomy and placement of a pressure equalization tube often are sufficient to treat acute mastoiditis, the addition of a mastoidectomy reduces the risk of an intracranial complication or facial nerve paralysis developing.
It is best to not give preoperative antibiotics when operating for acute mastoiditis because they can affect the culture results. The patient will often require long-term antibiotics, and it is best to use culture-specific antibiotic therapy. Immediately upon opening the wound, cultures are taken. Then, broad-spectrum antibiotics can be started. When the culture results are available, the antibiotic spectrum can be narrowed.
Additional notes
The need for a mastoidectomy in acute mastoiditis is certainly debated. Overall, it probably decreases hospital length of stay, speeds recovery, and decreases the risk of developing the more serious complications of mastoiditis. For experienced surgeons, it is a short and low-risk operation. If there is a subperiosteal abscess or other complication such as facial nerve weakness, we will perform a mastoidectomy at the time of PE tube placement. In cases of noncoalescent mastoiditis and no other complications, a PE tube is generally adequate.
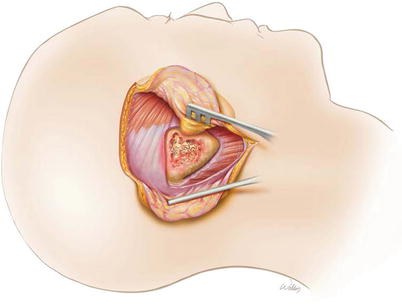
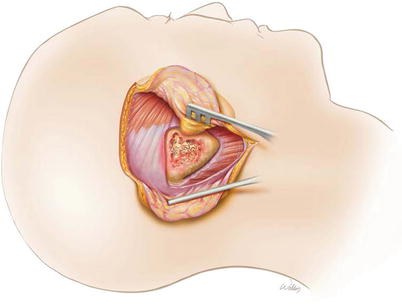
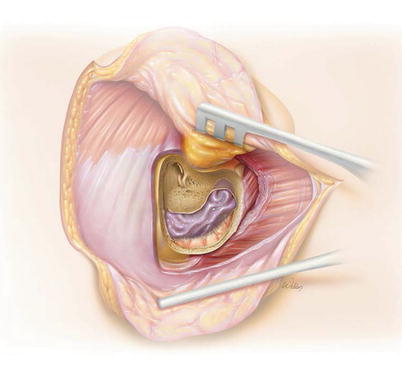
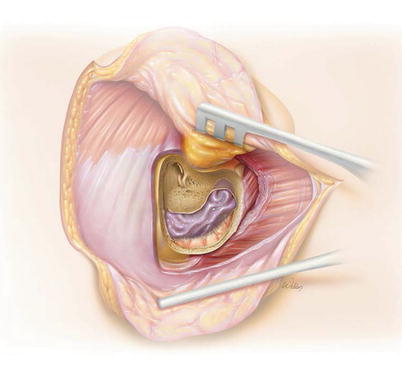
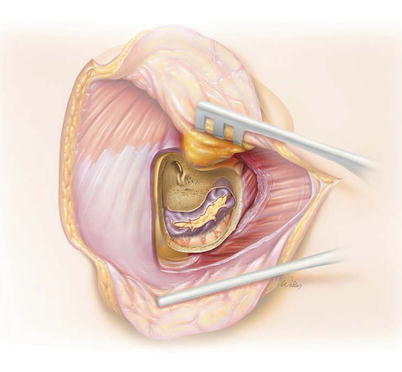
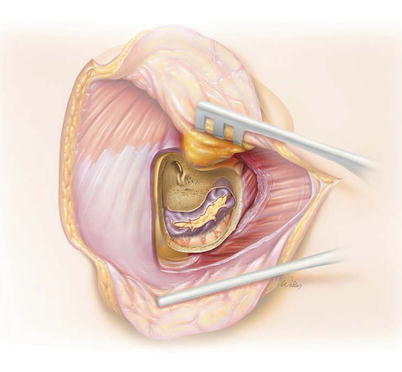
1.
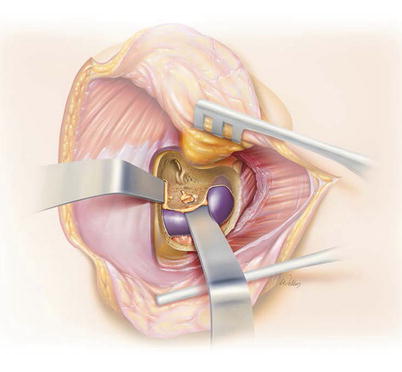
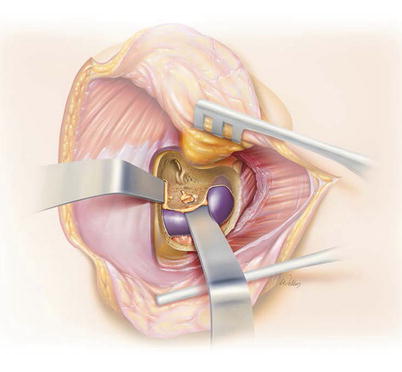
A subperiosteal abscess is illustrated. A standard postauricular incision is used, and cultures are taken immediately once the purulence is expressed.


2.
Elevation of the periosteum often reveals soft, inflamed mastoid cortex bone.
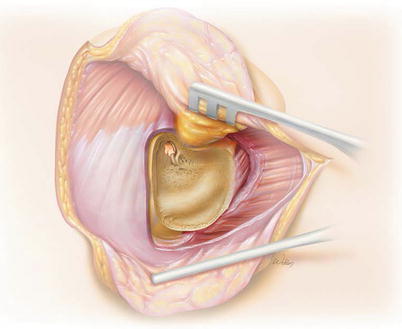
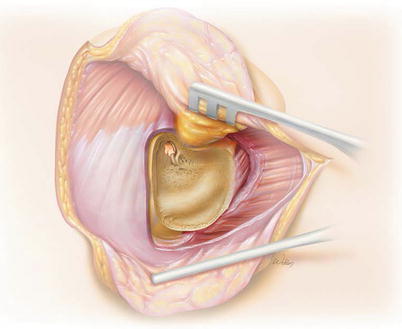
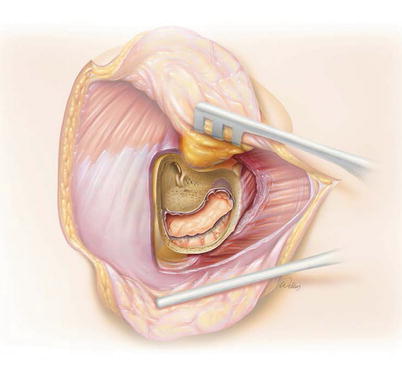
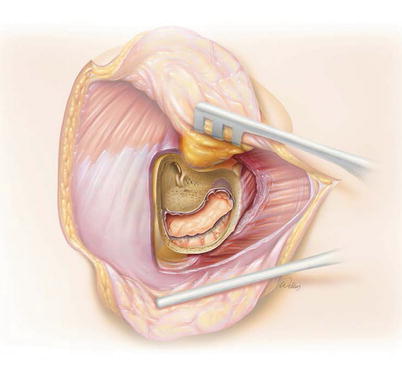
3.
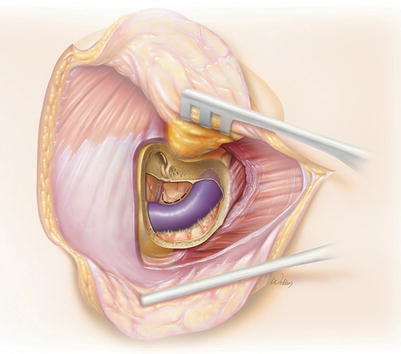
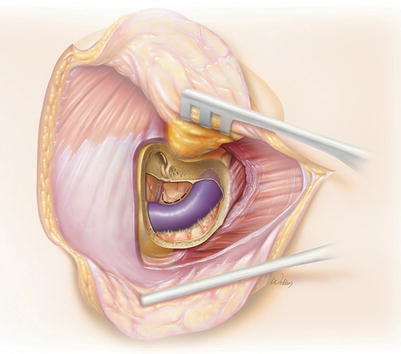
A simple mastoidectomy is performed with identification of the sigmoid sinus, the tegmen, the mastoid antrum, and the lateral semicircular canal. A bone pate collector can be used to collect bone dust for tissue culture if desired.
Only the antrum needs to be opened. There is no need to try and remove all inflamed granulation tissue from the aditus ad antrum, the facial recess, or even all the mastoid air cells.
After performing a mastoidectomy, the cavity is irrigated. The mastoid can be filled with ototopical antibiotic drops if desired.
The wound can be closed with a Penrose drain protruding from the mastoid cavity through the bottom of the incision if desired. The goal is to prevent reaccumulation of purulence within the mastoid.
A myringotomy with pressure equalization tube is then placed to drain the middle ear.
4.
Case 1. Acute mastoiditis with a subperiosteal abscess. There is postauricular erythema and swelling.


5.
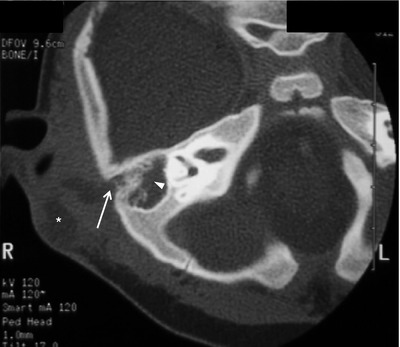
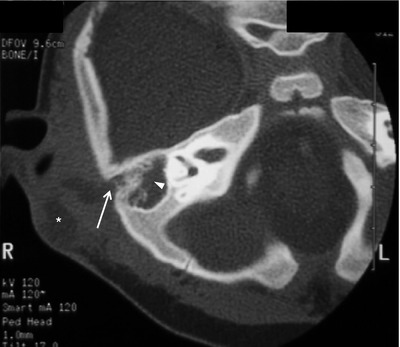
CT demonstrates erosion of the mastoid cortex (arrows).


6.
Case 2. Acute mastoiditis with a subperiosteal abscess in a baby.


7.
CT scan demonstrates erosion of the mastoid septae (arrowhead), the mastoid cortex (arrow), and a subperiosteal abscess (asterisk).
Retrolabyrinthine Craniotomy for Intracranial Complications of Acute Mastoiditis
Concept
Perform a simple mastoidectomy, and then expose the posterior and/or middle fossa dura to address an intracranial complication.
Conditions treated
Acute mastoiditis with an intracranial complication including sigmoid sinus thrombosis, an epidural abscess, or a subdural abscess
Risks
Hearing loss
Facial nerve injury
Meningitis
CSF leak
Benefits
The procedure not only drains the infectious etiology within the mastoid but also provides direct access to the intracranial sites of disease extension.
This is a hearing preservation approach.
Additional notes
The management of an intracranial abscess that results from mastoiditis is also controversial. If the abscess is contiguous with the mastoid, we usually drain the intracranial component at the time of mastoidectomy. If it is not contiguous with the mastoid and the abscess is large, a separate approach will likely be required. However, a small intraparencymal abscess will likely not need surgical treatment and can usually be managed with intravenous antibiotics, close monitoring, and sequential imaging to verify that it is resolving.
8.
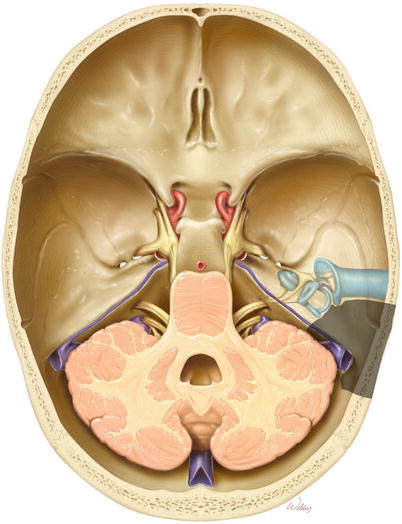
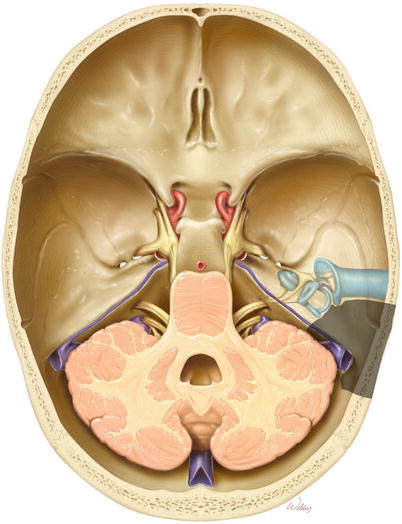
Overview of the bone to be removed (gray).
9.
The retrolabyrinthine craniotomy begins with a standard postauricular incision.
10.
The periosteum is elevated off the mastoid cortex.
11.
A simple mastoidectomy is performed with identification of the sigmoid sinus, the tegmen, the mastoid antrum, and the lateral semicircular canal.
12.
The retrosigmoid dura is identified and thinned with a large diamond burr. The bone is then removed.
13.
The bone over the sigmoid sinus is thinned and “egg shelled.” A Joseph or Freer elevator is used to remove the bone fragments to visualize the sinus.
14.
Malleable retractors are then used to retract the posterior and middle cranial fossa dura away from the bone. This bone is then removed down to the level of the labyrinth.
15.
A completed retrolabyrinthine craniotomy provides access to the sigmoid sinus, the presigmoid posterior fossa dura, and the middle fossa dura superior to the mastoid.
16.
Representative illustration of a patient with sigmoid sinus thrombosis in which the lateral surface of the sigmoid sinus is distorted but intact.
The concept of making an exploratory opening into the sigmoid sinus to assess for thrombosis is not often used. Typically, preoperative imaging is sufficient to make this diagnosis. Palpation can help determine if the sinus is patent; a clot will feel firm and is not easily compressed. If there is a question intraoperatively about whether or not there is a clot in the sinus, a vascular Doppler probe should be brought in to assess for blood flow.
17.
More commonly, however, the wall of the sigmoid sinus is disrupted when there is an infectious thrombosis (i.e., thrombophlebitis or an abscess within the sigmoid sinus). Simply exposing the sigmoid sinus reveals the problem.
18.
Gentle curettage of the abscess/clot/granulation tissue can be used to debride the sinus down to the medial wall. We typically do this with a Freer or duckbill elevator. In our experience, this usually won’t bleed because both the proximal and distal sigmoid sinuses are occluded by the disease. However, this approach permits drainage of the abscess and necrotic tissue.
19.
Representative illustration of a patient with an epidural abscess involving both the middle cranial fossa and the posterior cranial fossa. Removing the overlying bone reveals granulation tissue and necrotic material adherent to the dura, which can be curetted out.
20.
Representative illustrations of how to manage a posterior cranial fossa subdural abscess that lies directly under the presigmoid dura. This can be treated by incising the dura over the abscess. Alternatively, a retrosigmoid craniotomy could be performed.
21.
Opening the dura reveals the abscess wall.
22.
The abscess can be opened with a knife and the pus suctioned out. No attempt is made to dissect out the wall of the abscess. It will resolve with intravenous antibiotic therapy.
23.
The dura should be closed in a watertight fashion to prevent CSF leak into the ear. Tisseal is helpful here.
24.
Case 1. A child presented with a protruding right ear. Axial CT with contrast demonstrated acute mastoiditis. There was erosion of the mastoid septae, and the wall of the sigmoid sinus was thickened (arrows). This child was very lethargic and in the ICU.










