Chapter 22 Case A 40-year-old man, who is a smoker, has C7 radiculopathy that did not respond to medical treatment, and a large, soft single disc. Participants Advocating Against Artificial Cervical Discs: Rasha Germain and Volker K.H. Sonntag Application of Artificial Cervical Discs: Ricardo B.V. Fontes and Vincent C. Traynelis Posterior Discectomy for Soft Disc Herniation: Miguel A. Arraez Moderator: The Puzzling Development of Artificial Cervical Disc Arthroplasty: A. El Khamlichi Anterior cervical discectomy and fusion is the most common surgical procedure used and has proven successful in the treatment of symptoms caused by degenerative cervical disc disease. First described by Smith and Robinson in the 1950s and modified over the years, this procedure remains the gold standard for the treatment of disc herniation, foraminal and spinal stenosis, and axial discogenic pain. Excellent clinical and radiographic outcomes are obtained in 85 to 95% of patients. Despite these good outcomes, however, long-term studies of patients after discectomy and fusion have shown that as many as 25% of patients may develop recurrent radicular symptoms from adjacent segment degeneration. Furthermore, surgical intervention for symptomatic adjacent-level disease has been reported in as many as 2.9% of patients annually after fusion.1 Finally, although it is not clinically correlated, radiographic evidence of adjacent-level disease has been reported in as many as 92% of fusion-treated patients 5 years after surgery.2 The cause of adjacent-level disease after fusion is debated. It may be the result of an altered biomechanical environment or due to the natural history of the degenerative process.3 The effects of cervical fusion on spinal bio-mechanics have been heavily studied. Intradiscal pressures increase significantly during flexion at both superior and inferior adjacent levels.4 Kinematic studies show increases in mobility and angular displacement at adjacent levels, both near and remote, after fusion.5,6 Nonetheless, no direct clinical correlation with these biomechanical findings has been established. Whether the progression of cervical disease can be halted by maintaining preoperative kinematics is still unknown. The development of nonfusion spinal devices for use in cervical arthroplasty has been driven by the hope that maintaining motion may decrease the incidence of adjacent-level disease. Over the past 10 years, technology in the realm of cervical arthroplasty has evolved and improved, with various design revisions and the establishment of clear indications for arthroplasty. The many device designs and their kinematic characteristics must be considered when selecting the appropriate device for implantation.7 Most arthroplasty devices have single-gliding or double-gliding interfaces, including ball-and-socket and saddle designs, which allow rotation and translation around an axis of rotation. To protect the facet joints from abnormal stresses, an implant must have an axis of rotation that is near-physiological. In some implants the axis of rotation is fixed, and in others it is mobile. These devices also may be semiconstrained or unconstrained, in which case they rely on surrounding soft tissues to provide restraint in the extremes of range of motion. Maintaining the posterior longitudinal ligament enhances stability, and resection of this ligament has been associated with hypermobility at the index level and implant failure. Unconstrained devices allow translation and diminish stress at articulating surfaces, although they may subject the facet joints to greater stress. Unconstrained devices with a mobile axis of rotation are more forgiving of small errors in placement; fixed axis- of-rotation devices require more precise placement. Constrained devices achieve greater stability but transmit greater stresses to articulating surfaces and require stronger fixation. The Prestige (Medtronic Sofamor Danek, Memphis, TN), ProDisc-C (Synthes, Paoli, PA), and porous coated motion (PCM) (Cervitech, Rockaway, NJ) are semiconstrained devices, whereas the Bryan disc (Medtronic Sofamor Danek) is unconstrained. Both the Bryan and Prestige discs have mobile centers of rotation, in contrast to the fixed centers of rotation of ProDisc-C and PCM devices. Thus, aside from general procedural considerations with the placement of a prosthesis, there are concerns about which device will best serve the patient. Clinical trials in Europe, Canada, the United States, Australia, and China have sought to determine the safety and short-term efficacy of several of the available cervical discs. Many studies have focused on the Bryan disc, ProDisc-C, and Prestige.8–10 Early surgical results appeared promising, with most reported complications related to the learning curve associated with device implantation. Early and 24-month clinical results appeared promising as well, with good postoperative ratings of patient satisfaction, an improved neck disability index, improved neck and arm pain scores, and an earlier return to activity as compared with traditional anterior cervical discectomy and fusion.11–13 Nonetheless, longer follow-up has raised several concerns that merit further investigation. First, it is difficult to assess the accuracy of clinical outcomes obtained through patient surveys. Within the noninferiority studies conducted in the U.S., a primary determinant of “success” has been more than a 15-point improvement in the neck disability index, a survey outcome measure that each patient completes during follow-up. When a new device becomes available, patients’ enthusiasm for the “improved” technology is a well-known phenomenon. Patients who complete follow-up assessment forms are likely to express an inherent bias, especially if they are dissatisfied about not receiving the “new technology.” Studies done with patients randomized at surgery, with both the patient and examiner blinded during follow-up to the treatment received, will help resolve this issue. Second, the purpose of cervical arthroplasty has been to maintain the patient’s preoperative level of functional spinal unit-motion parameters, including range of motion, translation, and center of rotation. Although most short-term studies document near-physiological motion after cervical arthroplasty, the magnitude of prothesis motion has been noted to decrease with time. Kinematically, therefore, several devices become equivalent to a fusion over time. In 2008, Sasso and Best14 reported that, at 24 months, more flexion and extension motion was retained in the group of patients undergoing Bryan disc replacement than in those receiving plates at the index level (6.7 degrees vs. 0.6 degrees, respectively). During flexion and extension, however, the range of motion both above and below the operative level was not significantly different between the groups of patients. Likewise, at the 12-month follow-up, the increase in anterior/posterior translation initially noted at 6 months at the level above fusion in patients receiving plates was not significantly different from that of the disc replacement group. Longer follow-up is needed to determine whether disc replacement preserves preoperative kinematics at the levels adjacent to fusion, or whether the trend will continue toward loss of motion even with arthroplasty. Heterotopic ossification, both anteriorly and posteriorly, resulting in fusion across the implant level has also been reported. McAfee and colleagues15 proposed a classification scheme to study heterotopic ossification in the lumbar spine, and Mehren and associates16 adapted the scheme for heterotopic ossification in the cervical spine (Table 22.1). In a prospective study of 54 patients (77 total implanted prostheses, ProDisc-C, Synthes), only 33.8% of patients showed no signs of heterotopic ossification at 1 year. Ossification of grade 2 to 3 was present in 49.4% of patients, and 10.4% of the patients had heterotopic ossification that restricted their range of motion. Spontaneous fusion of the treated segment was noted in 9.1% of cases. Furthermore, the rate of heterotopic ossification was significantly higher in multilevel cases compared with single-level cases. Goffin and colleagues17 measured the range of motion of 139 implanted Bryan cervical discs at 1 year. The range of motion of 18 discs (12.9%) was less than 2 degrees, and further evaluation with computed tomography (CT) showed evidence of anterolateral paravertebral ossification. With a 3-year follow-up, Sola and coworkers18 found evidence of heterotopic ossification in 16 of 21 patients with implanted Bryan discs (76.2%), missing motion in 10 (47.6%), and definite fusion in six patients (28.6%). The ossification appeared anteriorly in all of these patients. In the U.S., current investigational device-exemption study designs include a 2-week course of postoperative nonsteroidal antiinflammatory drugs, which, in orthopedic surgeries, have been shown to inhibit ossification when administered early in the postoperative period. The outcomes of long-term studies of this issue will be interesting. Recently, several papers have addressed the issue of changes to sagittal cervical alignment after disc replacement. In 2004, Pickett and colleagues19 reported that pre-operative alignment worsened in all 14 of their patients who underwent implantation of a Bryan disc, with a mean change in end-plate angle of −3.8 degrees, and a mean change in functional spinal unit angle of −6 degrees. Similarly, Johnson and associates20 reported that, of 10 patients undergoing single-level arthroplasty, 80% developed end-plate kyphosis through the prosthesis, with a mean loss of 4.7 degrees of lordosis. The overall loss of lordosis (C2-C7) was −2.7 degrees, which was not statistically significant. Fong and coworkers21 reported that 9 of their 10 patients undergoing single-level arthroplasty developed kyphosis through the operative level, with a mean change of −9 degrees. No significant change in overall cervical alignment was detected. In a larger study by Sears and associates,22 both the median loss in functional spinal unit lordosis and the median development of prosthesis shell kyphosis was 2 degrees. The mean overall loss in cervical lordosis (C2-C7) was 4 degrees. None of the changes in sagittal alignment were clinically correlated in any of the studies. Pickett and colleagues,23 however, described one patient with marked segmental kyphosis after cervical arthroplasty who underwent revision surgery 8 months later to correct the deformity. His symptoms resolved 12 months after the second surgery. Table 22.1 Grades of Heterotopic Ossification in Cervical Arthroplasty
The Application of Artificial Discs
Advocating Against Artificial Cervical Discs
Grade | Extent of Heterotrophic Ossification |
0 | None present |
I | Detectable in adjacent soft tissues, but not within the confines of the intervertebral disc space |
II | Present between end plates, with possible effect on prosthesis motion |
III | Present with bridging osteophytes; restricting, but still permitting motion |
IV | Causing fusion across the treated level |
Source: Modified from McAfee PC, Cunningham BW, Devine J, Williams E, Yu-Yahiro J. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech 2003;16:384–389; and Mehren C, Suchomel P, Grochulla F, et al. Heterotopic ossification in total cervical artificial disc replacement. Spine 2006;31:2802–2806.
Many studies have focused on the effect of fusion on the sagittal alignment of the cervical spine, and the development of kyphosis may prove to be clinically important in the development of adjacent-level disease and symptoms of pain. Kawakami and associates24 found that the risk of axial symptoms after cervical fusion was significantly related to cervical kyphosis and loss of vertebral body height at the fused segment. In addition, one factor found to promote degenerative change in the levels adjacent to a fusion was kyphotic change across the fused segment and overall loss of cervical lordosis.25 As yet, no single surgical or clinical factor appears directly responsible for the development of postoperative kyphosis after cervical arthroplasty. The issue merits further investigation if indeed kyphotic change is associated with progression of disease.
Finally, preservation of motion through nonfusion technology introduces the possibility of same-level degeneration, a problem not typically encountered after solid fusion. Same-level degeneration may involve the intervertebral disc, facet joints, or ligamentum flavum. Because segmental motion is preserved, progressive facet arthrosis leading to joint hypertrophy is a concern.26 Exclusion criteria for cervical arthroplasty include facet arthrosis at the affected level.
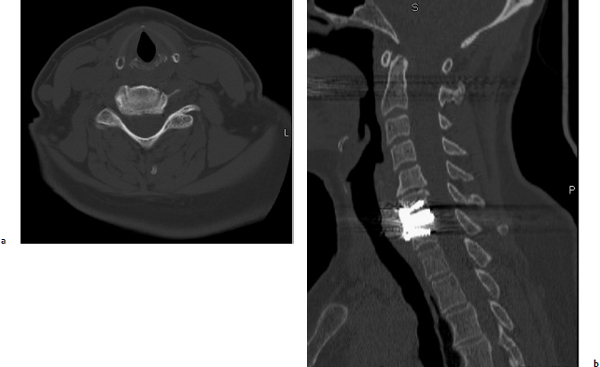
Furthermore, imaging after cervical arthroplasty is problematic. Magnetic resonance imaging (MRI) is the standard modality for evaluating patients both before and after surgery. Despite promising early clinical results, reoperation at the index level after cervical arthroplasty has been reported, and imaging is necessary in the event of suspected device failure or in patients with new neurologic symptoms.27 Due to image artifact after disc replacement, it may be more difficult to determine the presence of same- or adjacent-level disease. The clarity of MRIs was analyzed by comparing four available devices.27 Both Bryan and Prestige LP devices enabled satisfactory visualization of the spinal canal, exit foramina, and both adjacent levels. However, the quality of MRIs deteriorated significantly at both index and adjacent levels with the ProDisc-C and PCM devices. The relatively high metal content of the devices also produced artifact on CT scans. Thus, after initial flexion/extension plain films have been obtained, further evaluation of the implant position and range of motion would require CT myelography.
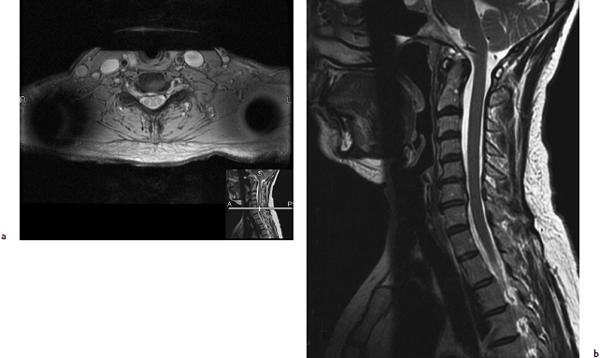
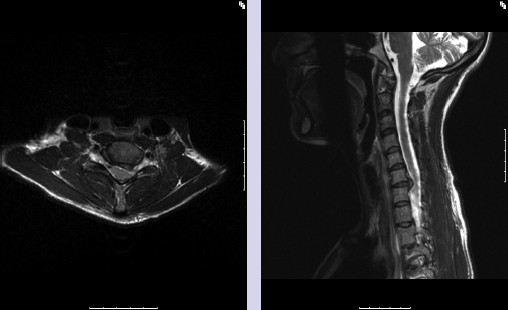
More years of follow-up are needed before the role of cervical arthroplasty in the treatment of degenerative cervical disc disease can be determined. If the goals are to maintain segment motion and to offset the progression of adjacent-level disease, the focus must be on demonstrating that cervical arthroplasty meets these demands. Few reports on the long-term outcomes of cervical artificial discs are available, but some trends are developing. With 3 years of follow-up, Sola and associates18 reported anterior ossification in 16 of 21 operated levels (76.2%), missing motion in 47.6%, and definite fusion in 28.6%. We have noted the progression of adjacent-level disease in patients after cervical arthroplasty (Figs. 22.1, 22.2, 22.3).
The experience with lumbar disc replacement has provided clues and ideas about how to avoid pitfalls with patient selection and device construction. Likewise, long-term studies with lumbar devices may provide clues about the future of cervical arthroplasty. With a 17-year follow-up, Putzier and associates28 reported a spontaneous fusion rate of 60% with lumbar disc replacement. Bertagnoli and Schönmayr29 reported a 5% incidence of adjacent-level degeneration with a 2-year follow-up, whereas Huang and colleagues30 reported a 24% incidence with a 9-year follow-up.
Until long-term information about implanted cervical devices is available, our expectations and patient selection criteria should remain conservative. The device should be offered only to patients who stringently meet the determined criteria. Furthermore, the potential for progressive adjacent-level disease must be recognized, irrespective of the surgical technique employed.
Fig. 22.1a,b Preoperative axial (a) and sagittal (b) T2-weighted magnetic resonance imaging(MRI) scans showing a C6/7 herniated disc with right foraminal stenosis. The patient had suffered from persistent right-arm pain consistent with a right C7 radiculopathy for 2 years, and conservative treatment had failed.(Courtesy of the Barrow Neurological Institute.)
Application of Artificial Cervical Discs
Several operative approaches are available to treat the cervical radiculopathy from this patient’s disc herniation. We believe that cervical arthroplasty represents the best treatment strategy in such a relatively young individual who presents with single-level symptomatic disease with normal alignment and relatively little spondylosis. In this section, we present the evidence supporting this opinion.
Posterior Discectomy
Posterior cervical decompression promptly relieves radicular symptoms, and fusion is not required. Unfortunately, the durable efficacy of this treatment option has yet to be defined in any scientifically valid study. Experienced surgeons have published descriptions and analyses of the procedure and a critique of the most significant works follows. Scoville and colleagues31 presented 208 cases with long-term follow-up, but the review is seriously flawed because of selection bias. The reported experience represents only 13% of the total group of patients treated with a posterior cervical discectomy over the time of the study, and no information is provided to explain how the study group was chosen. Therefore, the findings from such a highly selected group cannot be expected to represent the overall outcomes of this procedure. Murphey and associates32 treated 648 patients over a 34-year period but chose to report the outcomes of only 380 cases. Similar to the work of Scoville and colleagues, the reasons for limiting the review to a small subset of the total experience are unclear. These authors do not provide any information concerning the duration of follow-up, and data regarding axial neck pain and the need for additional surgery are not included. These shortcomings completely negate the reported findings.
Henderson and colleagues33 performed a retrospective review of 846 consecutive patients with a mean follow-up of 146 weeks. Radicular symptoms recurred in 172 patients (20.3%) and a second procedure was required in 103 patients (12.2%). The average time between the two operations (169 weeks) was greater than the mean length of follow-up for the entire series, which led the authors to speculate that “the long-term recurrence rate might well be higher than indicated.” Furthermore, in the course of the study, 32 patients (3.8%) were ultimately treated with an anterior cervical fusion.
Kumar and associates34 addressed the outcome after cervical foraminotomy for radiculopathy due to osteophytic nerve-root compression, and the records of 89 consecutive patients were retrospectively reviewed. Although the mean postoperative follow-up was only 8.6 months, further surgery for recurrent root symptoms was required in 6.7% of patients, which represents a relatively high failure rate over such a short time. Clarke and coworkers35 retrospectively reviewed 303 patients treated with a posterior cervical foraminotomy. In this group, 20% had less than 3 months of follow-up and 30% had less than 1 year of follow-up. The main interest of this study was to assess adjacent-segment disease after posterior discectomy, but the poor follow-up does not allow for a valid assessment of that problem.
All of these papers represent the best data available. Unfortunately, the selection process and short follow-up introduces significant bias, and none of the studies employed validated outcome measures. Axial neck pain and return to work were not included in the reviews. The best long-term study suggests that this procedure is associated with a relatively high failure rate.33 In summary, although posterior cervical discectomy may have excellent short- and long-term results, there are no data to support this conclusion.
Anterior Fusion and Arthroplasty
Anterior cervical discectomy and fusion (ACDF) enables direct neural decompression and reconstruction of the anterior spinal column. The overall outcomes of ACDF have been reported in numerous retrospective studies, and data have accumulated from prospective investigations. The best data were acquired in the arthroplasty trials, which compared single-level cervical arthroplasty to an instrumented anterior fusion. Each of these studies is reviewed in the following paragraphs.
In 2007, the results of a randomized trial comparing single-level arthroplasty with the metal-on-metal unconstrained Prestige cervical disk system (investigational) to an instrumented ACDF (control) were published36 (Fig. 22.4). The 32-center study enrolled a total of 541 patients (276 arthroplasty, 265 ACDF), and 80% of the patients treated with arthroplasty and 75% of those treated with ACDF completed clinical and radiographic follow-up at the end of 2 years. The mean operative time was 90 minutes, and the average hospitalization was 1 day for both groups. The need for secondary surgical procedures (revisions, supplemental fixation, and hardware removal) in the ACDF group was 8.7%, which was statistically greater than that of the arthroplasty group (1.8%). Additionally, second surgeries at the adjacent levels were also more common in the ACDF group, with 11 procedures as opposed to three in the arthroplasty group. The incidence of adverse events was statistically similar in both treatment arms (arthroplasty 6.2%, ACDF 4.2%). Clinical outcome measures included the Neck Disability Index (NDI), the Short Form questionnaire (SF-36), neck and arm pain numeric rating scales, and neurologic and work status. Although great improvement was seen in both treatment groups compared with the patients’ preoperative state, there were some discrepancies between the cohorts. The arthroplasty group showed higher rates of NDI improvement at all postoperative intervals compared with the ACDF group, achieving statistical significance at 3 months. The arthroplasty group had statistically favorable neck pain scores at 12 months compared with the ACDF group. Neurologic success was higher in the investigational group (92.8%) compared with the control group (84.3%) at the 2-year point. Patients undergoing arthroplasty returned to work 16 days sooner than those undergoing ACDF. The Prestige implant maintained segmental sagittal angular motion averaging more than 7 degrees at the 2-year follow-up.
The results of the semiconstrained metal-on-high- molecular-polyethylene ProDisc-C were published in 2009.37 This study involved 13 centers at which 209 patients were enrolled. The investigational group consisted of 103 patients who underwent single-level arthroplasty with ProDisc-C, and the control group included 106 patients treated with an instrumented ACDF. Of these patients, 98% of the investigational group and 94.8% of the control group completed the 24-month follow-up period. The average intraoperative times for the investigational and control groups were 107.2 and 98.7 minutes, respectively. Blood loss and total hospitalization times were similar. The NDI scores improved tremendously after treatment with both modalities. Visual Analogue Score pain scores and the physical and mental components of the SF-36 showed statistically significant improvement compared with preoperative levels, but there was no difference between the two groups. Patient satisfaction was higher at all time points in patients undergoing reconstruction with an arthroplasty. Secondary surgical procedures occurred at a rate of 1.9% in the ProDisc-C group and 8.5% in the fusion group, similar to the results of the Prestige study. Device success (defined as no revision, removal, or reoperation) was 98.1% in the ProDisc-C group compared with 91.5% in the fusion group, which represented a statistically significant difference. The decline in narcotic and muscle relaxant use in the investigational group was statistically significant at 24 months. The ProDisc-C disc replacement successfully maintained motion throughout the study.
The study results for the Bryan cervical disc were also published in 2009.13 There were 30 investigational sites and the study randomized 242 individuals into the arthroplasty group and 221 into the ACDF group. Of these, 230 patients in the arthroplasty group and 194 patients in the ACDF group completed 2-year follow-up. As with the other studies, blood loss and operative and hospitalization times were similar between the treatment groups. Patients receiving an artificial disc did significantly better in terms of NDI improvement and neck pain scores than those treated with arthrodesis. Overall, 1.7% of patients in the investigation group and 3.4% of patients in the control group suffered implant-related serious adverse events. At the end of the follow-up, 2.5% of patients receiving a Bryan disc replacement and 3.6% of patients treated with an instrumented arthrodesis required a second operation at the index level. Preoperatively, the affected levels in the arthroplasty group had an average of 6.5 degrees of flexion/extension motion, which increased to 8.1 degrees at the final follow-up. Before surgery, 65% of the patients in both groups were working. The overall return to work significantly favored the investigational group (48 vs. 61 days).
Further cost analyses add an interesting dimension to the debate. Bhadra and associates38 studied the direct costs of four different surgical techniques to treat cervical radiculopathy. Arthroplasty yielded the second-lowest cost, second only to intervertebral allograft-only ACDF (without a plate). Recently, a health-economic assessment of cervical disc arthroplasty compared with allograft fusion showed that arthroplasty was associated with an average total savings of $6,978 per patient at 2 years after surgery. The cost difference was due to the lower reoperation rate and shorter return-to-work time of the arthroplasty group.39
Single-level ACDF does not alter global cervical motion, but there is increasing evidence that it alters biomechanical factors at adjacent levels, which may increase the risk of a patient developing adjacent-segment disease.40–43 Even if the incidence of symptomatic adjacent-segment disease after arthroplasty is equal to that seen with arthrodesis, we believe that preserving motion alone is an important goal. Although a single-level fusion does not have an impact on global cervical motion, the same is not true once multilevel fusions are necessary. Every segment that maintains normal physiological motion increases the potential for the patient to resume a fully active life.
Conclusion
Cervical arthroplasty is one of the most carefully studied and documented spinal procedures. It has been shown to be safe and effective and it preserves normal segmental motion. It is associated with a higher return-to-work rate and more rapid normalization of NDI and analogue pain scores than is ACDF. It appears to be associated with a decreased need for further surgery over the 2-year study periods, and it has an economic advantage over ACDF. For these reasons, we believe that arthroplasty is the best treatment alternative for this patient.
Posterior Discectomy for Soft Disc Herniation
A herniated disc is the most common indication for surgery in patients with disorders of the cervical spine. The posterior approach was developed in the 1930s and 1940s, but its obvious limitation in treating purely ventral herniated discs led to the use of the anterior approach. The posterior approach includes decompression techniques for patients with myelopathy as well as a posterolateral approach (laminoforaminotomy) for purely lateral root compression. This latter approach, which has been clearly encouraged in recent decades by the development of techniques for surgical field magnification, is the subject of this section.
Patient Selection
Patient selection through clinical and neuroradiological evaluation is of paramount importance for this approach. Only patients with cervical radiculopathy are candidates for the posterolateral approach, and those patients with concomitant spinal cord compression (myelopathy, myeloradiculopathy, or both) must be excluded. The neurologic examination can be complemented with a neurophysiological study to confirm the extent and severity of radicular involvement.
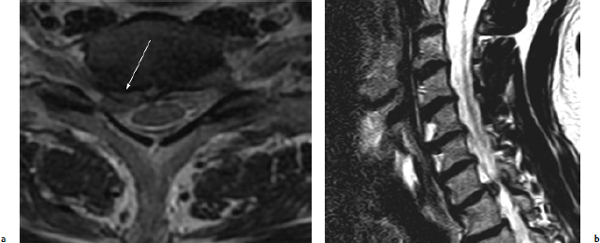
Pathophysiologically, root compression can be due to pure posterolateral disc herniation or to osseous root compression from foraminal stenosis. In patients with radicular involvement from a herniated disc, an MRI study can show the disc herniation as well as certain details of surgical interest, such as the site of the disc material in relation to the common posterior ligament and the foramen (Fig. 22.5). The most satisfactory surgical results can be obtained in patients who have radicular symptoms from pure disc herniation with posterolateral extrusion. In these patients, the symptoms are usually of sudden onset. The other group of patients who can benefit from this approach present with root pain in relation to the phenomena of osteophytosis of the uncovertebral processes or adjacent facets, constituting a clear foraminal stenosis. In these patients, a CT scan with bone algorithm is clearly indicated. This scan enables the surgeon to analyze the osseous anatomy of the foramen and suggests the degree of decompression and facetectomy needed (Fig. 22.6).
Surgical Technique
The procedure is performed with the patient under general anesthesia and in either a sitting position or a prone decubitus position. I prefer the sitting position, as the surgical field more easily remains bloodless, and it allows for some contralateral tilt, which contributes to a certain degree of aperture of the involved interlaminar space. A needle situated in the interspinous region permits radioscopic localization of the space. A skin incision of just a few centimeters is followed by sectioning of the subcutaneous plane and fascia, with subperiosteal dissection and unilateral separation of the paraspinal musculature. The use of a tubular or autostatic retractor exposes the laminas and joint processes. The advantages of tubular retractors include less blood loss, less postoperative pain, and a shorter hospital stay.44 Magnification is vitally important, either with microsurgery or endoscopy.
Fig. 22.5a,b (a) An MRI scan of a 45-year-old patient with an abrupt onset of right arm pain. The image shows a right herniated disc at C6-C7. Some fragments extrude through the posterior longitudinal ligament(white arrow) and compress the C7 root, a very good indication for the posterolateral laminoforaminotomy approach. (b) Sagittal view. The sequestered disc is completely out of the intervertebral space and behind the vertebral body.