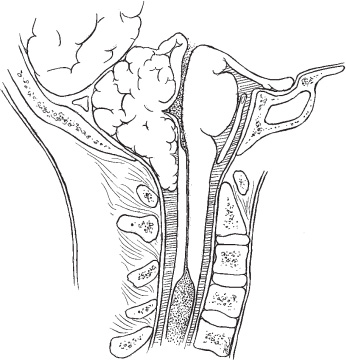
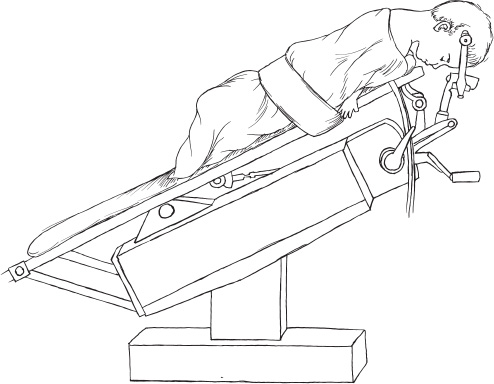
The Chiari I malformation (CIM) is the most subtle form of hindbrain herniation. It is generally not associated with congenital neural-tube defects and consists of caudal migration of the cerebellar tonsils through the foramen magnum a variable distance. When cerebrospinal fluid (CSF) movement is severely restricted, it commonly causes syringomyelia. With the introduction of magnetic resonance (MR) imaging and the increased ease of visualization of the craniocervical junction, our ability to diagnose this condition has increased exponentially. At the same time, the safety of craniocervical decompression has increased, making operation a much more attractive option. The most difficult problems facing the clinician currently are what symptoms justify operation and defining the line between a truly pathological state and an innocent anatomic variant. Surgery for a patient with a CIM (Fig. 3–1) should be considered if the patient is symptomatic from spinal cord or medullary compression, if there is an associated syrinx, or if significant pain is thought to be produced from the lesion. Pain is currently the most common presenting symptom of a patient with a CIM. It is most easily appreciated when the patient is old enough to communicate effectively and consistently complains of sharp pain in the craniocervical junction or occiput induced by activities that cause abrupt increases in intracranial pressure (ICP). Children who are noted to begin laughing and then suddenly to grab the back of their neck in pain are diagnosed easily. Initiating activities may include coughing, vomiting, bowel movements, strenous physical exercise, or anything associated with a Valsalva maneuver. Less clear are cases of patients who have life-altering dull pain in the occipital region without any initiating factors; however, even within this group, I have seen dramatic improvements following surgical decompression. Symptoms specific to the compressive aspect of the problem are many and range from life-threatening alterations of basic functions (e.g., bradycardia, apnea), to motor disturbances (e.g., myelopathy), to cranial nerve signs (e.g., dysartharia, dysphagia, strabismus). This is the least common form of presentation today, but its life-threatening nature demands our attention. When present, the simplest to appreciate and most objective indication for surgery is the presence of an appropriate syrinx. Although there are numerous other causes of syringomyelia, hindbrain herniation is the most common. The syrinx usually is located in the cervical or upper thoracic region. The longer the skip area between the craniocervical junction and the syrinx, the more uncomfortable the clinican should become to attribute the cavity to the hindbrain CSF dynamic disturbance. Occasional patients will have a syrinx without an obvious cause (trauma, neoplasm, arachnoiditis) and have unimpressive caudal tonsillar descent. Even in this group, craniocervical decompression has been effective in resolving the intramedullary CSF collection. Great care must be exercised to search exhaustively for other causes before assuming this to be the case. FIGURE 3–1. Midsagittal drawing of the craniocervical junction of a patient with a Chiari I malformation. Note the descent of the cerebellar tonsil to the upper edge of C-1 and the presence of a large syrinx beginning at C-3 and extentding inferiorly. The C1-2 region is spared. Relative contraindications for a Chiari decompression include raised ICP, cervical instability, and significant upper cervical ventral compression. Evaluation of a patient for a CIM should begin with a complete history and physical examination, including a neurologic evaluation. Special attention should focus on the optic fundi for papilledema, pain on neck motion, scoliosis, leg- or foot-length discrepency, loss of pain or temperature over the trunk and an asymmetric abdominal reflex. Sensory testing in small children can mislead even experienced clinicians. Temperature assessments over the trunk are generally more reliable than testing the child with a sharp point. Today virtually every patient being evaluated for a CIM undergoes MR imaging. Exceptions are children with pacemakers, cochlear implants, or some other technical reason why MR imaging should not be performed. A small subpopulation of patients may need general anesthesia to obtain an adequate study. The detail and ease of MR imaging are truly impressive to anyone who has had experience with the pre-MRI era. No other radiographs come close to the precision of MR imaging in delineating the anatomy of the craniocervical junction or for the evaluation of syringomyelia. Rarely is useful information obtained with contrast enhancement, and it can generally be avoided. Much enthusiasm accompanied the introduction of cine-MR imaging to evaluate CSF flow in this region. We have had this capability for several years and still are awaiting critical information to be obtained using this modality that would be helpful and that would alter the decision based on the routine MR imaging. This includes the presence of CSF behind the tonsils in patients with large syrinxes who were effectively treated with posterior fossa decompression. MR imaging should include images of the cervical and thoracic spinal cord. On occasion, the syrinx from a CIM may skip the cervical region and appear only in the thoracic region. Some evaluation of ventricular size is necessary. This information can be obtained by either MRI or computerized tomography (CT). Hydrocephalus or raised ICP should be considered prior to any consideration of posterior fossa intervention. The bony anatomy of the craniocervical junction can be seen easily on routine radiographs of the cervical spine. To the extent the child will voluntarily move the neck, flexion and extension films will help to ensure pre-operative stability. These films should be done cautiously or under fluoroscopic control if neck pain is present. The art of persuading a frightened child to move the neck through the extremes of flexion and extension is routinely performed in pediatric centers without difficulty. Ventral compression by the dens or some other tissue in the region is increasingly recognized as a contributing factor in the formation of hindbrain hernias. Special attention should be given to this assessment. As with many other areas of medicine, ventral compression is not simply present or absent, but rather it may be some gradation along that spectrum from no abnormality to full impaction. If significant ventral compression of the dens into the medulla is present, consideration should be given to addressing this issue primarily and then reassessing the remaining factors. The assessment of ventral compression is done with sagittal MRIs. Flexion and extension MRIs can be obtained in the cooperative child but are technically difficult. As previously stated, hydrocephalus and raised ICP should be addressed before any consideration of surgery for the posterior fossa pathology. Posterior fossa decompression in the presence of hydrocephalus is dangerous and has little likelihood of resolving the CSF flow problem and avoiding a shunt or third ventriculostomy. Cervical instability may be addressed at the same time as the Chiari decompression, but more care will be necessary in positioning and fixating the patient during positioning for the procedure. Ventral compression of sufficient magnitude to warrant primary consideration is generally done by transoral resection of the dens and then careful reevaluation of the craniocervical stability. Once these three issues are resolved, operative planning for the Chiari decompression can begin. From the preoperative sagittal MRI, the extent of tonsilar descent can be assessed along with the position of the torcula and the degree of any brainstem displacement. The general condition of the skin and, in particular, the skin in the area of the incision should be evaluated. Open draining wounds, as from an insensitive foot ulcer, should be healed before this or any other elective procedure can be considered. A successful operation starts with proper positioning. The head is held in a pin head-holder, taking care to avoid a shunt, if present, or excessive pressure if the sutures are not fused. The patient is turned prone and the neck is flexed. Flexion is not extreme, and two fingers should be inserted easily between the chin and chest. The head of the bed is elevated until the operative field is parallel to the floor (Fig. 3–2), which decreases venous pressure and facilitates hemostasis. Once positioned, the midline occipital hair is clipped but not shaved. I use a chest Doppler both to detect air embolus and to listen to the heart rate. Small fluctuations in the heart rate occur with manipulation of vital medullary areas and can be appreciated easily. The initial exposure begins in the midocciput and extends to the spinous process of C-2 (Fig. 3–3A). It is rare that C-2 must be removed, and leaving the muscular and ligamentous attachments to C-2 minimizes postoperative pain and instability. The avascular plane between the nuchal muscles is identified by a small amount of fat that separates them. With the monopolar current or periosteal elevator, the muscle insertions on the occiput are removed. In the area of the posterior arch of C-1, care is taken to avoid the frequent bony spina bifida and inadvertant injury of the underlying neural tissue. Young infants will have significant cartilage in the posterior arch that can easily be penetrated by using monopolar current or an instrument. With the muscle and other soft tissue reflected laterally, exposing the mid-occiput to the foramen magnum and the posterior arch of C-1, a decision is made as to the extent of the lateral exposure. This is a midline operation, and there is no need for extreme lateral exposure. When both the foramen magnum and posterior arch of C-1 begin to turn vertically, exposure of soft tissue must be halted. Alternatively, the width of the spine from the MR imaging and the exposure necessary can be measured. There is little reason for a vertebral artery injury to occur with this procedure. In addition, the artery is encased in a venous plexus that will transmit an arterial pulse to warn the observant operator of the approaching structure. Burr holes are placed on each side of the midline and connected with a drill or rongeurs. The horizontal width of the foramen magnum opening should approximate the height of the exposure. The posterior arch of C-1 is removed with rongeurs. There is no place for a posterior fossa craniotomy that is replaced; this is a decompressive operation.
CHIARI I MALFORMATIONS
Surgical Indications
Preoperative Evaluation
Operative Planning
Intraoperative Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


