Figure 14.1. Bilateral hyperintensity in the striatum, with FLAIR sequence, in a patient with chronic hyponatremia which worsened after 3 weeks, not promptly corrected, corresponding to extrapontine myelinolysis.
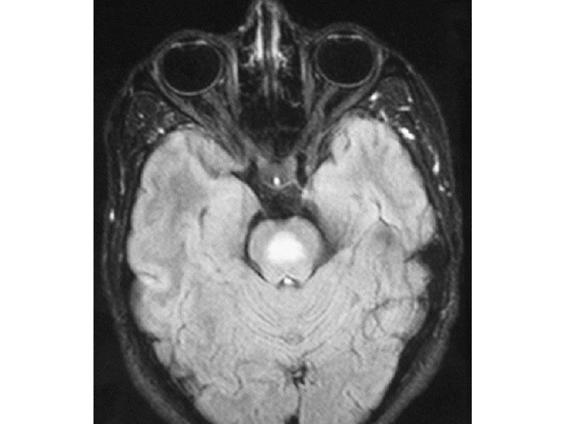
Figure 14.2. Marked hyperintensity in the pons of the same patient, with FLAIR sequence, corresponding to pontine myelinolysis.
14.2.6 Conclusions
Hyponatremia is a condition that can be identified and properly managed if the underlying causes are identified and possibly eliminated. On the basis of the patient’s symptoms, hyponatremia should be corrected, taking into account whether it is acute or chronic and whether it constitutes an emergency or not.
In acute and life-threatening cases, the aggressive correction of sodium levels is beneficial, and the occurrence of myelinolysis is unlikely. In chronic cases, the suspension of the cause and the delicacy of the sodium correction are key to recovery without sequelae. The broad symptomatic spectrum and the presence of other comorbidities difficult to the management of hyponatremia which requires clinical expertise to finally beat it.
14.3 Hypernatremia
14.3.1 Definition, Epidemiology, and Risk factors
Hypernatremia is defined as a blood sodium concentration >145 mEq/l. It is the direct result of water loss or gain of sodium, so there is a positive balance of the cation in the extracellular space, resulting in a response to counter it by thirst, water outflow from the intracellular space or by increasing the renal sodium excretion. It is a less common alteration than hyponatremia (5% of total electrolyte disorders) and equally affects both sexes. It has a higher incidence in the elderly and children, because of the difficulty of these groups to have free access to liquids or because misaligned in the thirst mechanism in older people. Patients with psychogenic hypodipsia, children and elderly or those mismanaged with inappropriate infusions (iatrogenic) have an increased risk of hypernatremia.
The mechanisms that produce hypernatremia can be summarized as follows:
- Loss of fluid due to insufficient vasopressin function (decreased secretion or inadequate renal response to normal secretion). Extrarenal loss: diarrhea, profuse sweating. Decreased fluid intake (central or psychogenic adipsia, unavailability of water). The most serious consequence of this loss is cellular dehydration.
- Increase of sodium in the extracellular space caused by fluid losses, with positive balance of the cation, which also contributes to hormonal imbalances such as primary hyperaldosteronism and Cushing’s syndrome. Further poor management of infusions (sodium bicarbonate, parenteral nutrition) and dialytic hypertonic solutions contribute to an iatrogenic increase in the sodium balance.
One of the major causes of hypernatremia is diabetes insipidus (DI), both central and nephrogenic. The cardinal symptom is polyuria, which can reach more than 15 litres per day. Central DI is caused by the insufficient production and subsequent secretion of vasopressin or antidiuretic hormone by the neurohypophysis, which implies that the kidney is unable to concentrate urine. Consequently, blood sodium is increased, triggering the thirst mechanism. There are multiple root causes: ablation surgery, pituitary tumours, trauma (skull base fracture), intracranial infections, and congenital malformations. The cause is unknown in about 30% of cases. Renal or nephrogenic DI is clinically indistinguishable from central DI; however, the simple infusion of exogenous ADH (desmopressin) and the change in urine osmolarity can help in making the diagnosis: it is central if there is an increase in osmolarity and nephrogenic if urine is diluted.
In renal DI, the kidney is insensitive to adequate concentrations of ADH in the blood, and starts concentrating the urine, creating a noticeable increase of sodium in the extracellular fluid. The causes are the use of aminoglycosides, rifampicin, lithium salts, oral hypoglycemic agents, amphotericin B, demeclocycline, etc. Systemic inflammation such as amyloidosis may arise, as well as polycystic kidneys and electrolyte imbalances such as hypocalcemia and hypokalemia.
Hypernatremia has a variable clinical expression and depends on how quick its onset is and on the degree of nervous system involvement. In adults it usually remain asymptomatic until reaching levels as high as 160 mEq/l. Thirst can be a guiding symptom, especially in the beginning of the disease, and if the subject urinates significant quantities. The evolution of symptoms to coma and seizures depends on how quick the onset of hypernatremia is; high levels of sodium are tolerated with minimal symptoms, because of the balance maintained with the gradual exit of fluid from the extracellular space. This is impossible to achieve if there is a sudden (within <48 hours) increase in plasma osmolarity at the expense of sodium. Consequently, the intracellular fluid space rapidly decreases, contributing to neuronal dehydration, and leading to a series of symptoms proportional to the intensity of dehydration.
14.4 Clinical Management and Treatment
The best approach is to try to eliminate the cause, but sometimes, given the urgency of symptoms, rapid correction of hypernatremia is essential. The correct measurement of volume and urine osmolarity are critical to guide the diagnosis: if there are large volumes of not concentrated urine, the diagnosis will be DI, and the elective diagnostic test will be the desmopressin test to identify whether it is central or neurogenic. In the case of small volumes of urine and a higher concentration of sodium, the kidneys try to conserve water from the extracellular space and excreted sodium, as in hypernatremia of extrarenal origin and iatrogenic diseases, Cushing’s syndrome or Cohn’s disease. Normal renal osmolarity in children and adults is between 400 and 800 mOsm/kg. Under conditions of fluid restriction for more than 12 hours, levels of osmolarity of 400 mOsm/kg or less could be an index of severe kidney damage. Hypernatremia should be managed taking into account the volume of extracellular space to find out if it is euvolemic or hypovolemic hypernatremia. The amount of water needed by the body can be calculated using the following formula:
Free water deficit = Body weight (kg) x Total body water (%) x ([Serum Na/140] – 1)
Where the percentage of body water (TBW) accounts for approximately 60% by weight, hence, the constant 0.6 times the weight of the patient.
If hypernatremia is hypovolemic, infusion of normal saline (0.9%) is the treatment of choice, until the signs of dehydration decrease. Hypotonic solutions (“D5” – 5% dextrose; hypotonic saline fluids such as 0.45% sodium chloride solution) should then be administered to restore the volume and reverse the hypernatremia.
In cases of euvolemic hypernatremia, as occurs in elderly patients with poor thirst mechanism, oral rehydration therapy is indicated and effective.
In central DI, in addition to water restriction and low sodium diet, desmopressin administration (intranasally or subcutaneously) can help to alleviate the deficit of vasopressin. In nephrogenic DI it is important to delete the trigger, usually a drug (phenytoin, lithium salts, acyclovir, demeclocycline, amphotericin B); this is sometimes enough to normalize serum sodium. Otherwise, a low-protein and low-sodium diet, supplemented with low doses of hydrochlorothiazide, is critical for relieving the kidney from solute overload.
Serum sodium should never decrease to <0.5 mEq/l/h because a rapid decline in serum sodium can cause cerebral edema. Do not administer more than 50% of the estimated deficit in the first 24 hours. The onset rhabdomyolysis and myelinolysis after aggressive correction of hypernatremia. Rhabdomyolysis and myelinolysis after aggressive correction of hypernatremia have been reported.
General References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







