Figure 4-1 A, Axial 3 Tesla (T) T2-weighted fast-spin echo (FSE) with fat suppression obtained after gadolinium arthrography demonstrates the origin of the tibial intraneural cyst from the posteromedial aspect of the superior tibiofibular joint (arrow), the “tail sign.” Tibial intraneural cyst extension (asterisk) is seen within the parent nerve. There is also extraneural extension of cyst arising from the anterior portion of the superior tibiofibular joint (black plus signs). Note the popliteus muscle denervation (white plus sign). B, Axial 3T T2-weighted FSE image with fat suppression proximal to part (A) shows intraneural cyst extension (asterisks) within the tibial nerve with crescentic displacement of nerve fascicles, the “signet ring” sign (arrows). C, Three-dimensional coronal reformatted image from a posterior perspective from a vastly undersampled isotropic projection reconstruction (VIPR) data set shows the origin of the intraneural cyst (asterisks) from the joint (arrow) with propagation along the articular branch of the nerve (“j-shape”) to the tibial nerve proper in the distal thigh (dotted line).
Operative findings
Balloon expansion of the tibial nerve was apparent at the level of the popliteal fossa. Distally, the cystic expansion became less prominent, but a cystic branch could be traced to the posterior aspect of the superior tibiofibular joint (Fig. 4-2). A small longitudinal opening was made into the cystic branch and an abundant amount of mucoid material was removed. The superior tibiofibular joint was resected, the small extraneural cyst anterior to the joint evacuated, and the articular branch of the tibial nerve ligated and disconnected near the joint capsule. A pathologic specimen of this articular branch was histologically consistent with an intraneural ganglion.
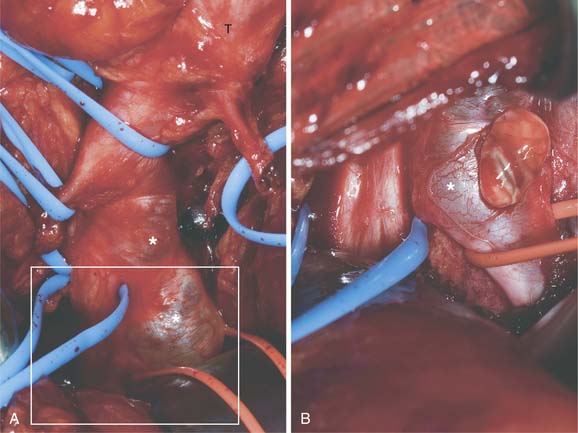
Figure 4-2 A, Intraoperative appearance of the tibial (T) intraneural nerve cyst (asterisks) at the level of the popliteal fossa from a posterior approach. The cystic articular branch (within the red vasoloop) can be traced to the posterior aspect of the superior tibiofibular joint. The blue vasoloop within the inset box surrounds the descending unaffected tibial nerve which has been protected. B, Enlargement of area within the inset box. A small longitudinal incision was made in the cystic articular branch (in red vasoloop) and an abundant amount of mucoid material was removed. The descending tibial nerve (in a blue vasoloop) is unaffected.
Postoperative course
Immediately after surgery, the patient had complete resolution of his pain and subjective improvement of toe flexion. Toe flexor strength improved clinically and electrophysiologically at follow-up assessment 3 months postoperatively, at which time an MRI documented no evidence of intraneural cyst recurrence.
CONCLUSION
Despite the finding of joint connections in only 40% of lower limb1 and 20% of upper limb3 intraneural ganglia cases in the literature, robust clinical, experimental and historical evidence has recently been presented to support a synovial origin of these cysts.1 The essential principle of the unifying articular theory rests on the presence of a joint connection to a neighboring, often degenerative, synovial joint. A capsular defect allows passage of joint fluid into an articular branch and subsequently into the parent nerve. The cyst follows the path of least resistance and tracks within the constraints of the epineurium, displacing fascicles. With increased intra-articular pressures, proximal extension of the cyst seems to be preferential. Cyst fluid can extend within the nerve for a considerable distance, for example, from the superior tibiofibular joint in the proximal leg as far proximally as the sciatic nerve in the buttock. In addition, cyst fluid within the tibial nerve that has reached the level of the sciatic nerve bifurcation can cross over4; i.e., a cyst that had ascended up the tibial nerve can fill the shared epineurial sheath within the sciatic nerve and then secondarily affect (namely, descend down) the common peroneal nerve (Fig. 4-3). The pressures and pressure fluxes that determine cyst propagation patterns can also help explain fluctuating symptoms and signs.1 Careful analysis of high resolution MRI has played a pivotal role in characterizing the pathogenesis of this entity. Reproducible, generalizable imaging findings have been reported in intraneural ganglia at different sites,5 which indicate a common formation and propagation. These imaging signs, exploiting anatomic descriptions, are illustrated in this report (see Fig. 4-1).
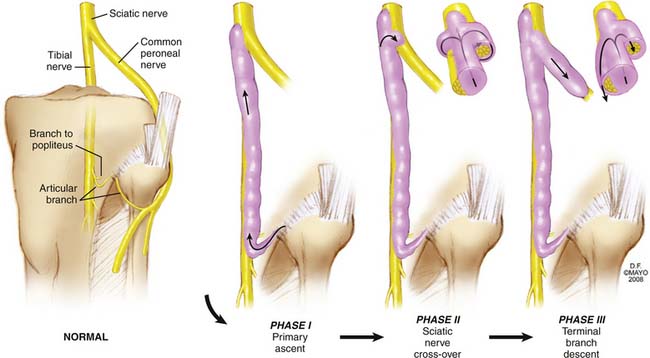
Figure 4-3 Artistic representation demonstrating primary ascent of the intraneural ganglion from the posterior aspect of the superior tibiofibular joint along an articular branch connection into the tibial nerve (Phase I). At the level of the sciatic nerve, cross-over can occur from circumferential filling of the common epineurial sheath (Phase II). Cyst reaching the sciatic nerve can then descend down either the parental or the cruciate (crossed) pathway (Phase III).
(By permission of Mayo Foundation for Medical Education and Research. All rights reserved.).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








