45 Thoracoscopic Approach
I. Key Points
– Working angles and trajectories to the thoracic spine are comparable between the thoracoscopic and open anterolateral (thoracotomy) approaches. Posterior elements, contralateral roots, and the contralateral pedicle cannot be accessed.
– Thoracoscopy allows access to the entire thoracic spine (T1 to T12) and eliminates the need for an approach surgeon. Similar access may be obtainable with mini-open techniques.
– Thoracoscopy requires a unique skill set, knowledge of anatomy, and familiarity with unusual instruments. Proficiency typically requires considerable laboratory preparation.
– Single-lung ventilation via a double-lumen endotracheal tube is required for thoracoscopic access. Patients with significant obesity, cardiac dysfunction, and/or pulmonary comorbidities may require specialist referral for preoperative clearance.
II. Indications
– Microdiscectomy for symptomatic thoracic herniation
– Sympathectomy: primarily utilized for palmar hyperhidrosis after failure of medical management. Craniofacial hyperhidrosis, axillary hyperhidrosis, reflex sympathetic dystrophy, and palmar ischemic phenomena are less common indications.1
– Osteomyelitis/discitis, epidural abscess, nerve sheath tumor, vertebral biopsy, corpectomy, costovertebral joint pain, vertebral reconstruction, and spinal deformity2
– Contraindications: malignant tumors requiring en bloc resection, intradural pathology. Due to high rates of intradural migration and calcification, open thoracotomy is favored for giant (occupying >40% of canal diameter) midline herniated discs.3
III. Technique
– The patient is turned to the lateral decubitus position, an axillary roll is placed, and the upper arm is gently raised and supported via an armboard. After the patient is secured to the operating table, the bed is rotated to assist gravity retraction of the lung.
– Single-lung ventilation ensues after reconfirmation of position of the endotracheal tube.
– The surgeon stands facing the patient’s chest. Various portal configurations are acceptable depending on the level of interest. Working portals are biased toward the anterior axillary line (usually equidistant from the level of interest), and the endoscopic portal is biased toward the posterior axillary line.
– A 1 cm incision is made along the superior costal margin. Blunt dissection with a hemostat and/or finger, as in chest tube placement, is used to pierce the parietal pleura. Working portals are placed under direct vision with the endoscope. Minor adhesions are lysed using a combination of blunt and sharp dissection.4
– Sympathectomy for palmar hyperhidrosis:
• One or two working portals are required (typically the third and/or fourth intercostal spaces), and the endoscope is placed at the fifth intercostal space.
• The second rib is identified inferior to the apical fat pad and the brachiocephalic and subclavian vessels. The sympathetic chain is then transected at the second and third rib heads with bipolar cautery followed by scissors. The ends are gently dissected and separated.1
– Discectomy
• Based on the necessary exposure, the parietal pleura overlying the rib heads and/or bodies is incised with cautery. The pleura can be reflected with elevators, cautery, or further sharp dissection. Segmental vessels are mobilized, ligated, coagulated, and transected when necessary (Fig. 45.1).
• A dissector is used to separate the neurovascular bundle from the inferior costal margin and to dissect the superior margin free from pleura and muscular attachment. The costovertebral joint is disarticulated using a levered Cobb elevator. The distal rib is transected, and the rib head is removed. The exposed pedicle is resected with Kerrison rongeurs. The dura and exiting root are now visualized.
• A cavity is drilled into the disc space and adjacent bodies, and the disc fragment is removed with careful curettage directed away from the thecal sac.
– Closure
• A chest tube connected to standard suction (–20 cm H2O) is directed toward the lung apex through a working portal and secured in an airtight fashion. The thoracic wall is inspected with the endoscope. The remaining working portals are closed, and the atelectatic lung is reinflated under direct vision.
• Chest tubes may be removed before the patient leaves the operating room. Alternatively, chest tubes can be left in place until output diminishes to less than 100 cc/day, transitioned to water seal, and removed later.4
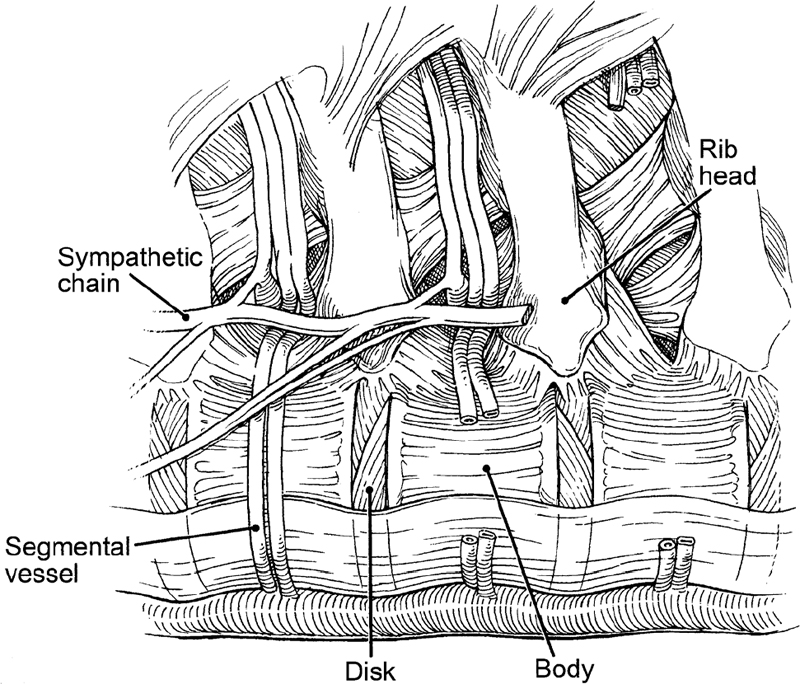
Fig. 45.1 Thoracic anatomy demonstrating relationship of vertebral bodies to ribs, sympathetic chain, and segmental vessels (used with permission from Barrow Neurological Institute).
IV. Complications
– Durotomy: Repair methods include hemoclips or fascial harvest for onlay graft with fibrin sealant, and temporary lumbar cerebrospinal fluid (CSF) diversion. Chest tubes should be placed to water seal. Occult CSF leaks may be identified with a Valsalva maneuver.
– Wrong-level procedure: Localization can typically be achieved by identifying anatomic landmarks with the endoscope and confirmed by fluoroscopy. Ribs articulate with the disc space above the corresponding vertebral body (e.g., the T5 rib leads to the T5 pedicle and T4/T5 disc space). A radiopaque fiducial may be placed preoperatively in the pedicle of interest.
– Persistent pneumothorax or atelectasis
– Miscellaneous complications: neurovascular compression syndromes (positioning), intercostal neuralgia (typically transient), gustatory sweating (sympathectomy), Horner syndrome (sympathectomy involving stellate ganglion), and chylothorax
V. Postoperative Care
– An upright anteroposterior radiograph is obtained in the recovery room and the next morning to evaluate for persistent pneumothorax.
– Aggressive pulmonary toilet, incentive spirometry, and nebulizer use are promoted to prevent atelectasis.
VI. Outcomes
– Sympathectomy
• Increase of more than 1°C in palmar temperature monitoring, an indirect marker of vasodilation, is a useful intraoperative prognostic for success.1
• Uniform reports of 96 to 100% relief of palmar hyperhidrosis. Rate of compensatory hyperhidrosis (e.g., legs, back, trunk) ranges from 50 to 61% in large series. No useful predictors of compensatory hyperhidrosis.4
– Discectomy
• Advantages reported over thoracotomy in terms of pulmonary complications, operative pain, wound complications, chest tube duration, intercostal neuralgia and rib resection, and decreased length of hospital stay
VII. Surgical Pearls
– To avoid inadvertent injury to lung parenchyma or to vascular or neural structures, the working tips of all instruments should be visualized at all times with the endoscope.
– A larger cavity drilled into the disc and body, if necessary, may be useful during discectomy. All movements should be directed away from the thecal sac.
– Disc calcification is not a contraindication to thoracoscopic microdiscectomy (unless giant) but may require more extensive drilling (e.g., diamond burr) to protect the thecal sac against levered resection during curettage.
– Portal incisions should be planned to facilitate conversion to open thoracotomy if needed.
– Use of an angled endoscope may be useful for confirming decompression of the anterior thecal sac and root(s), especially in the setting of suspected residual disc.
Common Clinical Questions
1. Describe characteristics of a herniated disc least appropriate for thoracoscopic microdiscectomy.
2. What are the success rate and most common side effect of thoracoscopic sympathectomy for palmar hyperhidrosis at T2/T3?
3. Name three surgical or postoperative strategies to prevent severe complications related to CSF leakage during thoracoscopic surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







