Anatomy of the circle of Willis.
- A1, ACA:
part 1 of anterior cerebral artery;
- A2, ACA:
part 2 of anterior cerebral artery;
- ACoA:
anterior communicating artery;
- BA:
basilar artery;
- iICA:
intracranial segment of internal carotid artery;
- MCA:
middle cerebral artery;
- P1, PCA:
part 1 of posterior cerebral artery;
- P2, PCA:
part 2 of posterior cerebral artery;
- PCoA:
posterior communicating artery;
- PICA:
posterior inferior cerebellar artery;
- V4, VA:
part 4 of vertebral artery.
Imaging tips
Using a hand-held probe (2 MHz) for routine examination of the circle of Willis through different acoustic and anatomical windows, the examiner can be oriented by the depth, the spectrum and the direction of the flow (toward and backward from the transducer). Details are introduced in the following section.
The first step is to localize the temporal acoustic (transtemporal, TT) window where the ultrasonic beam can penetrate and the flow in the MCA can be identified.
To shorten the time to find the window and to identify the flow in an artery, examination can begin with the maximum power and large sample volume (i.e., power 100%, sample volume 10–15 mm); subsequently we can reduce the above-detailed parameters until the quality of the sign can be evaluated well [8].
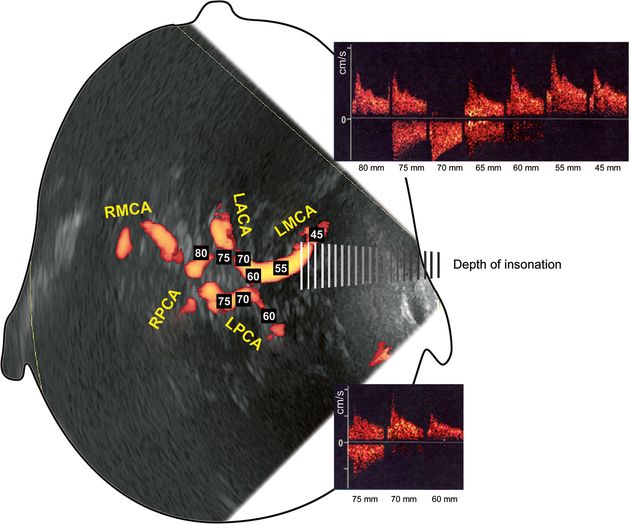
The recommended initial depth is 55–60 mm from the TT window. At this distance, Doppler signals from the carotid siphon, the MCA, ACA and even the PCA can be found.
The standard TCD requires registration of the Doppler signal at 2- to 5-mm intervals with a 3- to 6-mm gate (in other words, sample volume) in order to locate the intracranial vessels in optimal cases. The Doppler setting should be adjusted to obtain the highest velocity in all cases.
In case there is no acoustic window (7–20% of acute stroke patients, particularly elderly individuals and those from certain ethnic groups do not have an adequate acoustic window [9]), the examination can be carried out from the direction of the orbita and the foramen magnum, and also submandibularly.
Low (10%) power should be used when TCD examination is performed through the orbital window, burr holes or fontanel.
Flow can be orthograde and retrograde. Orthograde means that it is directed toward the probe, usually above the zero line. Retrograde means that it is directed from the direction of the probe, below the zero line. Note: the appearance of the direction of the flow can be changed on the display (above or below the zero line)!
Monitoring method was developed for long examinations with probe fixation on both sides (helmet or a different holding device incorporating the ultrasound probe).
The accuracy of TCD diagnosis depends both on the experience of the sonographer and the features of the ultrasound equipment. The artifacts (objective or operator dependent) that affect the ultrasound beam must be taken into consideration – they can lead to inappropriate conclusions [10].
Steps of investigation
Position of the patient
The standard TCD is performed with the patient in the supine position. It is strongly recommended that it is done after ultrasound evaluation of extracranial arteries. In some cases, TCD can be performed in the sitting or upright position of the patient depending on the research protocol (Figure 9C.2).

(A) Probe position in transcranial Doppler sonography to examine the iICA, MCA, PCA, A1 segment of ACA, ACoA and PCoA arteries. This is the transtemporal (TT) window. (B) Probe position for transorbital (TO) ultrasound examination. (C) The submandibular (SM) approach can be also used to study the distal ICA of the extracranial artery. (D) The transforaminal (TF) window is used for studying the posterior brain circulation. Head of the patient is bent forward and down.
Probe selection
TCD is performed using a standard 2-MHz pulsed-wave transducer or multifrequency 2–3.5-MHz probes. For children with an open fontanelle, adequate imaging is possible at a higher frequency.
Probe location
After fontanelle closure, the main available acoustic windows are the thinnest portion of the temporal bone, orbital aperture and foramen magnum (Figure 9C.3) [11,12]. Contact gel is used to decrease the resistance between the probe and the window’s surface.
Cranial approaches for TCD investigation: transtemporal (TT), transorbital (TO), transforaminal (TF) and submandibular (SM) windows.
Transtemporal (TT) window is detected in 90–95%, more difficult to find in adult women. The probe is placed over the area of arcus zygomaticus between the lateral edge of the orbit and the ear. This area is subdivided into three smaller windows (anterior, middle and posterior). By manually moving the probe the best Doppler signal is searched for. Initially the probe is focused at a depth of 55–65 mm looking for a signal from iICA, MCA, ACA or PCA. By stepwise changing the depth of insonation at 2- to 5-mm intervals it is possible to obtain sonograms from iICA, MCA, PCA, A1 segment of ACA, ACoA and PCoA arteries. Normally the highest velocity from MCA is recorded where the angle of insonation is the smallest.
Transorbital (TO) window is used for insonation of ophthalmic artery, carotid siphon and A1 of the homolateral ACA. The transducer is placed on the closed eyelid. Results can be disturbed by artifacts of the moving eye. The ultrasound beam should have a lower power (50–80 mW/cm2) and a sample volume of 10 mm. In case of a signal superimposition from two or more vessels, CCA compression tests may be applied for their identification.
The transforaminal (TF) or transnuchal window is used for studying the posterior brain circulation – both vertebral (VA) and the basilar (BA) arteries. In some cases signals from PCA (P1), cerebellar arteries and PCoA could be obtained [13]. The patient may be in a supine or sitting (head bent forward and down) position. The transducer is placed over the upper neck at the base of the skull and angled through the foramen magnum toward the nose. An increased gain and higher sample volume are required.
Other approaches for TCD examination:
A submandibular approach (SM) can be also used to study the distal ICA in the neck. The MCA/ICA mean flow velocity ratios can be calculated (Lindegaard index) [14].
In infants, open fontanelles (OF) provide additional acoustic windows for TCD examination. Through the anterior fontanelle it is possible to study iICA and the circle of Willis in coronal and sagittal planes. The superior sagittal sinus can be evaluated through an open sagittal suture. The posterior circulation can be insonated via the posterolateral fontanelle.
Identification of the basal cerebral arteries
The basal cerebral arteries are identified by the following criteria: (1) transcranial approach; (2) depth of insonation; (3) blood flow direction toward or away the probe; (4) visual and spectral analysis of the sonograms; (5) change of blood flow direction during common carotid artery (CCA) compression. All these criteria should be evaluated simultaneously [11,12].
Intracranial segment of ICA (iICA). It can be insonated by both TT (50–70 mm-depth) or TO (60- to 75-mm depth) windows. Through the TT window the signal is orthograde and stops during compression of the ipsilateral CCA. If the study is performed through the TO window the signal from the subclinoid segment is orthograde, from the genu of the ICA siphon is bidirectional and from the supraclinoid segment is retrograde (Figure 9C.4).
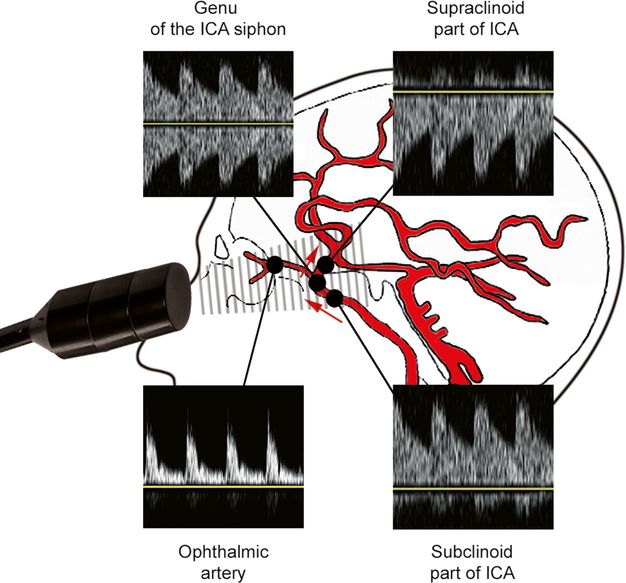
Single-ranged TCD pattern of ophthalmic artery and carotid siphon obtained by TO window.
The ophthalmic artery (OA) is evaluated in 35–50 mm depth using TO window. Its blood flow is orthograde with a typical pattern of a peripheral vessel. The study must be performed at reduced power settings to prevent ocular injury (Figure 9C.4).
MCA/ACA bifurcation. Its identification is made by using TT window in 55- to 60-mm depth. The signal from the bifurcation is bidirectional – the MCA signal is toward the probe (orthograde), ACA is away from the probe (retrograde). From 60- to 65-mm depth, iICA and PCA can be also recorded.
Middle cerebral artery (MCA). It is examined by the TT window in 40- to 55-mm (M1 segment) and 25- to 40-mm depth (M2 segment). The MCA should be tested at 2- to 5-mm intervals from its most superficial point to the MCA/ACA bifurcation. The Doppler signal is toward the probe (orthograde). At greater distances the signal may overlap with that of iICA, PCA or ACA. Upon ipsilateral CCA compression the velocity decreases or disappears, while during the contralateral CCA compression does not change.
Anterior cerebral artery (ACA). The Doppler signal from ACA can be obtained by using TT or TO windows in a depth of 60–70 mm. It cannot be found due to technical reasons in 20–30% of the cases. Its direction is below the zero line (retrograde) examined via TT window. In case of occlusion/severe stenosis of an ICA the flow direction of A1 can be reversed in collateral circulation of ACoA. The ipsilateral CCA compression reverses the direction of ACA blood flow (from retrograde into orthograde) if the ACoA is patent. In the presence of ACA hypoplasia the blood flow in the contralateral ACA is accelerated.
Posterior cerebral artery (PCA). The PCA is insonated by TT window in a depth from 55 to 80 mm. In some cases the signal can be obtained using TF window in a depth more than 95–100 mm. The signals from the precommunicating (P1) segment are orthograde and those from postcommunicating part (P2) are retrograde. The velocity parameters are lower than in other brain arteries due to the higher angle of insonation. The ipsilateral CCA compression reflects in increased PCA blood flow if the PCoA is passable.
Anterior communicating artery (ACoA). This artery can be investigated through TT or TO window. Its signal is provoked in the presence of significant vascular pathology. The direction of the Doppler signal depends on the direction of collateral blood flow to the probe. The ipsilateral CCA compression increases the contralateral ACA blood flow causing a typical noise.
Posterior communicating artery (PCoA). The signal from these arteries is also provoked by severe arterial obstructions or anatomic variants of the circle of Willis. It can be obtained by placing the probe over TT window in a depth of 55–65 mm. The PCoA blood flow is almost perpendicular to the probe therefore the actual blood flow velocity cannot be measured. The change of blood flow direction during CCA compression should be taken into account.
Basilar artery (BA). This is investigated through TF window at a depth of more than 85 mm (smaller depth can be used in smaller heads or children). The signal is retrograde with an average speed higher than that of the VA. Technically, the BA cannot be found in about 10–20% of people.
Vertebral arteries (VA). These are investigated using TF access in a depth range of 45–85 mm at 2- to 5-mm intervals. The normal signals are retrograde and often asymmetrical (based on different caliber of the VAs). The velocity parameters remain stable and slightly growing in depth. The identification of both VA is not easy due to anatomical variations in their course. The extracranial compression of VA behind the mastoid process stops the blood flow in the ipsilateral VA. This test is easily used in children and gracile individuals.
Posterior inferior cerebellar artery (PICA). This artery could be studied by TF window in a depth of 50–70 mm. A bidirectional blood flow is recorded from the VA/PICA bifurcation. The PICA blood flow is toward the probe and the signal is recorded above the zero line.
The stepwise, single-range TCD pattern of basal cerebral arteries using a TT window is presented in Figure 9C.5.
TCD interpretation
Normal TCD parameters
Doppler curves with spectral analysis are recorded from each depth of insonation (at 2- to 5-mm intervals along the entire course of the vessel), synchronic to the cardiac cycle.
The estimated TCD variables are: blood flow velocities (BFV) such as peak systolic velocity (PSV), mean flow velocity (MFV) and end-diastolic velocity (EDV) of the basal cerebral arteries (not angle corrected) and their indices: pulsatility index (PI, a measure of the variability of blood velocity in a vessel, equal to the difference between the peak systolic and minimum diastolic velocities divided by the mean velocity during the cardiac cycle); index of Pourcelot/resistance (RI: systolic velocity − diastolic velocity/systolic velocity); pulsatility transmission index (TPI: PI of study artery/PI of reference artery, e.g., MCA/ICA); asymmetry index (AI: mean MCA velocity/mean ICA velocity); and vasomotor reactivity (VMR: percent changes of M1 mean flow velocity after vasomotor stress, e.g., hypo- to hypercapnia) (Table 9C.1) [11,15]. Table 9C.1 shows the normal values of TCD velocities and indexes. Among them the mean velocity of the MCA is the most stable, reproducible and sensitive variable [16].
| Artery | Window | Depth (mm) | Flow direction | Mean velocity (cm/s) | RP | PI | TPI |
|---|---|---|---|---|---|---|---|
| MCA | ТТ | 30–60 | Orthograde | 58±12 [14] 62±12 [1] 58±15 [13] | 0.50±0.04 [17] | 0.92±0.16 [17] | 1.02±0.15 [17] |
| MCA/ACA | ТТ | 55–65 | Bidirectional | ||||
| ACA | ТТ (ТО) | 60–80 | Retrograde | 53±11[14] 51±12 [1] 49±15 [13] | 0.52±0.07 [17] | 0.91±0.26 [17] | 1.03±0.19 [17] |
| PCA (Р1) | ТТ | 60–70 | Orthograde | 37±10 [14] 44±11 [1] | 0.53±0.10 [17] | 0.95±0.34 [17] | 0.99±0.31 [17] |
| PCA (Р2) | ТТ | 60–70 | Retrograde | 37±10 [13] | |||
| BA | TF | 80–120 | Retrograde | 42±10 [1] | 0.54±0.07 [17] | ||
| VA | TF | 50–85 | Retrograde | 36±12 [14] | 0.57±0.08 [17] | 1.03±0.22 [17] | 1.06±0.40 [17] |
PI, pulsatility index; RP, index of Pourcelot/resistance; TF, transforaminal window; TO, transorbital window; TPI, pulsatility transmission index; TT, transtemporal window.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree