28 Transoral Odontoidectomy
I. Key Points
– The transoral approach allows the surgeon ventral midline access from the top of the arch of the atlas to the C2-C3 disc space.1
– A thorough preoperative assessment is necessary to ensure that the patient is free from any oral or dental pathology, which are contraindications to this approach.
– A minimum of 2.5 to 3 cm of dental clearance should be present to allow adequate exposure for odontoid resection.2
II. Indications
– Ventral spinal cord compression from rheumatoid pannus not amenable to posterior decompression and fusion
– Midline ventral cord compression from intradural or extradural spinal tumors
– Irreducible atlantoaxial subluxation with myelopathy and cord compression1
III. Technique
– The patient is positioned supine on the operating room table with a Mayfield headrest (Schaerer Mayfield, Randolph, MA), or in Mayfield tongs for greater control if there is instability of the occipitocervical junction.
• Prophylactic antibiotics consist of intravenous cephalosporin and metronidazole preoperatively and for 72 hours postoperatively.
• Nasotracheal intubation is preferred to avoid manipulation of the occipitocervical junction, and a nasogastric tube should be placed to prevent postoperative wound contamination.
– A transoral tongue retractor is inserted to visualize the oropharynx.
– A lateral fluoroscopic image is taken to localize the odontoid process and anterior arch of the atlas, followed by infiltration of 1% lidocaine with epinephrine into the planned incision site.
– A 2 cm full-thickness vertical incision is made in the midline, dividing the mucosa and pharyngeal constrictor musculature.
– A pharyngeal retractor is placed in a horizontal fashion, exposing the anterior tubercle of the atlas, origin of the longus colli, and anterior longitudinal ligament (Fig. 28.1).
– Cautery is used to skeletonize the ventral aspect of the arch of the atlas and the odontoid.
– The central 10 to 15 mm of the arch of the atlas is removed using a high-speed burr to expose the odontoid process in its entirety.1
– The odontoid is then resected using a high-speed burr for the anterior cortex and cancellous portion.
– Angled curettes are used to detach the apical and alar ligaments to allow the tip of the dens to be removed.
– Kerrison rongeurs (1 and 2 mm) and microcurettes are then used to complete the resection of the posterior dens cortical shell until the posterior longitudinal ligament and dura are identified.
– In patients with rheumatoid arthritis, the retrodental soft-tissue pannus is exposed following odontoid resection. Only loose fragments should be debulked, as complete pannus removal is usually unnecessary and risks a cerebrospinal fluid (CSF) leak.2
– The incision is irrigated with antibiotic solution, followed by closure of the muscle and mucosa in two layers with absorbable 3-0 suture.
– The retractors are removed, and 1% cortisone cream may be applied to the lips and tongue to decrease postoperative edema.
– The patient may be repositioned prone with the Mayfield tongs if a posterior stabilization and fusion procedure is planned.
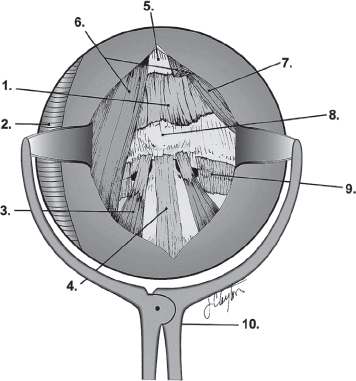
Fig.28.1 Retropharyngealanatomyandretractor. 1, anterioratlanto-occipitalmembrane; 2, armored nasotracheal tube; 3, longus colli muscle; 4, anterior longitudinal ligament; 5, clivus; 6, longus capitis muscle; 7, rectus capitis anterior muscle; 8, anterior tubercle of C1; 9, lateral atlantoaxial joint capsule; 10, retropharyngeal soft-tissue retractor. (From Haher T, Merola A, Surgical Technique for the Spine, Thieme; pg. 5, Fig. 1-5. Reprinted with permission.)
IV. Complications
– Neurologic injury
• Awake nasotracheal intubation avoids manipulation of the craniocervical junction.
• Somatosensory evoked potentials (SSEP) and motor evoked potentials (MEP) can provide intraoperative warning of spinal cord compromise.
• Keep mean arterial pressure (MAP) high to prevent ischemic spinal cord injury.
– CSF leak
• Direct dural repair (if possible), followed by fascial or fat graft
• Placement of subarachnoid lumbar drain postoperatively can be helpful.
– Airway obstruction
• Avoid premature extubation as reintubation can be very difficult and require emergency tracheostomy. Prior to extubation, evaluate for:
 Resolution of retropharyngeal swelling on lateral radiograph (usually 24 to 48 hours postoperatively)1
Resolution of retropharyngeal swelling on lateral radiograph (usually 24 to 48 hours postoperatively)1
 Ability to breathe around orotracheal airway2
Ability to breathe around orotracheal airway2
– Infection
• Can be minimized with meticulous wound closure and 72 hours of intravenous antibiotics
• Delay removal of nasogastric tube and oral fluid administration for 4 to 5 days postoperatively to allow for mucosal healing.
– Vertebral artery injury
• Preoperative CT or MRI scans should be reviewed to determine if there is an aberrant medial course of the vertebral artery, which is more common in patients with atlantoaxial rotatory subluxation.
• Dissection of the atlas should stay within 2 cm of the midline, and dissection at the level of the C2-C3 disc should stay within 1 cm of the midline.1
V. Postoperative Care
– The patient should be kept intubated for 2 to 3 days postoperatively to allow airway edema to subside.2
– Temporary use of an endotracheal cuff leak and tube changer can help anesthetist to guard against a difficult reintubation.2
– Once extubated, patient can be mobilized out of bed to chair in a cervical collar or orthosis depending on stability.
VI. Outcomes
– No level I studies have been performed to evaluate outcomes following transoral odontoid resection.
– Based on a review of smaller case series, improvement of preoperative neurologic deficits can be expected but is dependent on chronicity of spinal cord compression.
– In one 10-year review of 72 cases, there were two postoperative deaths and one pharyngeal infection requiring a repeat operation, with improvement seen in all patients’ neurologic function.3
VII. Surgical Pearls
– Care should be taken to avoid entrapment of the tongue against the teeth with the retractor system.
– As an alternative to palatal retractors, a red rubber catheter can be passed through the nares and sutured to the soft palate; it can then be used as a retractor.2
– The soft palate and mandible can be split to provide extensile exposure in the proximal and distal directions, respectively, although the increased morbidity should be considered.
Common Clinical Questions
1. Which of the following is the minimum clearance between the upper and lower teeth needed for performing transoral odontoid resection?
A. 1 cm
B. 2 cm
C. 3 cm
D. 4 cm
2. Which of the following is not an indication for transoral (anterior) odontoid resection?
A. Irreducible atlantoaxial subluxation with spinal cord compression
B. Spinal cord tumors at the C1 level causing ventral spinal cord compression
C. Rheumatoid pannus not amenable to posterior decompression and fusion
D. Atlantooccipital instability with myelopathy
3. Which of the following is the minimum average distance to the vertebral artery from the midline (in the medial to lateral direction) in the transoral approach to the odontoid?
A. 1 cm at the atlas
B. 2 cm at the C2-C3 disc
C. 2 cm at the atlas
D. 3 cm at the C2-C3 disc
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







