28 Transsellar/Transdorsal Approach via a Pituitary Transposition to the Interpeduncular Cistern
Daniel M. Prevedello, Amin B. Kassam, Juan C. Fernandez-Miranda, Paul A. Gardner, Ricardo L. Carrau, and Carl H. Snyderman
 Introduction
Introduction
Few locations in the human body are guarded by as many vital structures as the interpeduncular fossa. Its anatomical boundaries consist of the optic apparatus and the third ventricle superiorly, the mamillary bodies and mesencephalon posteriorly with the basilar artery and posterior cerebral arteries, and the posterior communicating artery with its perforators along with the oculomotor nerve bracketing the region laterally.1–3 The entire region is bordered anteriorly by the sella and its contents, including the pituitary gland and infundibulum.3–6 Therefore, access to this region is a challenge irrespective of the surgical approach.
Conventional anterolateral skull base approaches to the interpeduncular fossa have been described. However, they all require manipulation of the lateral contents of the interpeduncular cistern, and in particular of the oculomotor nerve and posterior communicating artery.2,7–13 Despite significant and extensive dissection, the final working space is often a small corridor between the optic nerves and tracts, cranial nerve III, and the branches of the posterior communicating artery. Ipsilateral visualization of the region directly located under the optic nerve and tract is particularly challenging.
Advances in endoscopic endonasal techniques have made possible the resection of skull base pathologies (expanded EEA endoscopic endonasal approaches).4,14–17 This work is performed by a skull base team consisting of two surgeons working with four hands through both of the patient’s nostrils. A dynamic and real-time movement of the endoscope facilitates the visualization and bimanual dissection. Endoscope holders are not recommended, as the continuous movement of the camera provides magnification as well as depth perception.17
Following a pituitary transposition, the EEA approach provides a direct route to the interpeduncular area without manipulation of cranial nerves. We believe that the pituitary gland is more tolerant of mobilization than any of the other structures within the interpeduncular cistern. In the event of postoperative dysfunction, it can be managed with endocrine replacement. All other surrounding structures, particularly the cranial nerves, are very sensitive, and their manipulation can produce iatrogenic deficits.18
 Indications and Advantages
Indications and Advantages
The indication for this procedure is directly related to the location and site of origin of the pathology. Any lesion behind the pituitary infundibulum requiring resection or decompression constitutes an indication for this approach. Tumors that are commonly located in this area are meningiomas, craniopharyngiomas, chordomas, chondrosarcomas, germinomas, teratomas, and granular cell tumors.
To better understand the advantages of the endoscopic endonasal pituitary gland transposition to reach the interpeduncular fossa, it is important to understand the limitations of the other approaches.
During a standard pterional approach, the structures limiting adequate exposure of the interpeduncular cistern are the optic nerves and the chiasm that limit access, mainly superiorly.1,19 An orbitozygomatic osteotomy augments the angle of exposure; however, the approach is still limited by the position of the optic apparatus.12 Sugita et al20 noted these issues and described the need to retract the optic tract and mamillary bodies to reach superior aspects of the interpeduncular cistern.
The carotid-oculomotor recess can be expanded by drilling the anterior and posterior clinoid processes, unroofing the optic nerve, and opening the cavernous sinus, with mobilization of the internal carotid artery (ICA) and cranial nerve III.1,8,21 Nevertheless, these variations generate greater morbidity by virtue of the need to mobilize neurovascular structures.1 Most, if not all, patients who undergo this procedure suffer a transient third nerve palsy.1,8,18,21
An alternative access to tumors that fill the interpeduncular cistern and extend into the third ventricle involves opening the lamina terminalis through a more anterior subfrontal or interhemispheric approach.22 However, this approach is equally limited in accessing the inferior portion of the interpeduncular cistern, and cannot be used when the floor of the third nerve is not eroded by tumor.22,23
Other approaches through the temporal fossa such as the transsylvian translimen insular approach and transchoroidal approach are other options to access the interpeduncular cistern.12 However, these approaches carry the potential for significant temporal lobe dysfunction.24
The anterior transpetrosal approach proposed by Harsh and Sekhar25 and the petrosectomy proposed by Kawase et al7 provide access to the prepontine cistern, but, as with other approaches, they are limited in exposing the retrosellar area.1
The posterior transpetrosal approach described by Hakuba et al2 in 1985 provides an improved caudal-cranial angle, thereby improving the access to the rostral portion of this region. However, adequate visualization of the interpeduncular cistern is obtained only by aggressive drilling of the petrous bone, which threatens hearing and balance functions.26 Additionally, the approach still takes a lateral to medial trajectory; therefore, a corridor between the optics and the oculomotor nerve is still required. Furthermore, visualization under the ipsilateral optic tract can prove to be difficult.2,26,27
The extended transsphenoidal route has been used by some to approach suprasellar pathologies located in the suprasellar space adjacent to the tuberculum sellae and planum sphenoidale.3,28–36 However, the microscopic transsphenoidal approach is limited in its parasellar exposure, particularly for lesions that extend far superiorly, laterally, or posteriorly into the perimesencephalic cisterns.3,28,30,31,33,36–38 Kouri et al39 pointed out that the presence of a lesion behind the stalk is one of the major limitations of the extended transsphenoidal approach. Others have suggested the use of an endoscope to improve visualization during transsphenoidal-microsurgical approaches. However, the limited working space within the speculum prevents effective maneuverability of instruments, and thus also prevents an adequate dissection.3,14,28,30–33,36–38
The main advantage of the pituitary transposition is to obtain adequate access and visualization to the retroinfundibular region, generating a midline approach to a midline lesion in a caudal to cranial orientation, thus avoiding manipulation of brain or cranial nerves. A total hypophysectomy should be considered when accessing lesions that have already compromised gland function, as is often the case with craniopharyngiomas.6
 Contraindications
Contraindications
Care should be taken when considering a pituitary transposition in children or young adults because there is a risk of pituitary dysfunction and infertility.40 All risks and benefits should be taken into consideration and they should be part of the informed-consent discussion with the patient and family before proceeding. Similarly, elderly patients and patients with comorbidities should be thoroughly evaluated preoperatively because they are prone to systemic complications.
We believe that the lack of multidisciplinary team cooperation is a contraindication for the procedure. The main team should include at a minimum a neurosurgeon, an otolaryngologist, and an endocrinologist, all of whom should have adequate experience. Similarly, the lack of specialized equipment, instruments (endoscope, bipolar, endo-scissors, etc.) or adequate infrastructure (intensive care unit, monitors, etc.) is also considered a contraindication for the procedure. Image-guidance systems are highly recommended.
 Diagnostic Workup
Diagnostic Workup
Physical examination should include a neurologic assessment with special focus on cranial nerve function. A neuro-ophthalmologic examination including a formal visual field test is recommended because many lesions in the suprasellar and retroinfundibular space compromise vision.
A preoperative endocrine evaluation is critical to determine the baseline function of the pituitary gland. Furthermore, confirmation of panhypopituitarism opens the possibility for total gland resection and avoiding unnecessary surgical dissection.
Imaging
Magnetic resonance imaging (MRI) with contrast is performed on all patients to elucidate the relationship among the skull base, brain, pituitary gland, and optic nerves. A computed tomography angiography (CTA) is also performed to better establish the relationship of the tumor with the intracranial vessels, particularly the basilar artery, posterior cerebral arteries, and posterior communicating arteries. Furthermore, the CT provides better visualization of the bone, which helps in planning the approach. MRI and CTA are often fused in the image guidance system to combine all the above-mentioned characteristics.
 Surgery
Surgery
Instrumentation
Adequate instrumentation is paramount for the endoscopic approach to the interpeduncular fossa. Necessary equipment includes high-quality endoscopes (0-, 45-, and 70-degree), preferably high-definition (HD); video equipment (camera and monitor); long endoscopic bipolar forceps; long and precise high-speed drills (hybrid 1-, 2-, 3-, and 4-mm); long dissection instruments; and hemostatic materials such as microfibrillar cellulose and foam/paste of collagen matrix mixed with thrombin.
Operative Setup
Patients are positioned supine on the operating table with their head fixed in a Mayfield head holder, attached to the image guidance system, with the head in a neutral position and the neck slightly rotated to the right side and tilted to the left. The nose is prepared with pledgets soaked with 0.05% oxymetazoline, followed by the external application of povidone iodine solution.
Preparation
The procedure begins with the removal of the right middle turbinate. A nasoseptal flap is elevated from the widest nasal cavity (discussed below; see Repair). A posterior septectomy is performed after disarticulating the rostrum from the sphenoid bone, creating a bilateral binostril exposure to allow freedom of movement.41 The left middle turbinate is generally lateralized and not resected.
The natural sphenoid ostium on the left side is widened to form one single cavity communicating the sphenoid sinuses with the posterior aspect of both nasal compartments. The lateral margins of the anterior sphenoidotomies are extended to the level of the medial pterygoid plates, and wide bilateral sphenoidotomies are performed.
Then, the sphenoidotomy is widened to include the lateral recess of the sphenoid extending lateral to the carotid canal, and the exposure is extended rostrally to expose the posterior cells of the ethmoid sinus to define the junction between the planum sphenoidale and the tuberculum sellae. Intrasphenoidal septations are carefully reduced with a drill, because they often lead to the vertical segment of the cavernous internal carotid artery (ICA).42 Finally, the floor of the sphenoid is drilled back to the level of the clivus, providing adequate space for the endoscope. This creates a caudal-to-rostral trajectory into the subchiasmatic space.
Bone removal over the sellar face is initially extended laterally over the medial portions of each cavernous sinus and rostrocaudally exposing both the superior (SIS) and inferior intercavernous sinus (IIS). The tuberculum is thinned using a high-speed drill and then removed.
Approach
The dura mater over the tuberculum, the SIS, and the entire pituitary fossa is now exposed and can be opened in a cruciate fashion. During the opening, the dura overlying the sella is opened carefully along the midline to avoid transgressing the thinner underlying soft tissue layer that forms the pituitary capsule. Once this plane is established, it is followed superiorly underneath the SIS. The SIS is ligated, clipped, or preferably coagulated with a bipolar electrocautery and then transected, communicating the suprasellar and sellar dural openings.
The sellar opening is completely widened laterally and inferiorly in a cruciate manner, facilitating visualization of the entire anterior face of the gland (Fig. 28.1). As the dissection progresses laterally, one can appreciate that the dense dura of the sellar floor bifurcates in the direction of the cavernous sinus (Fig. 28.2). This fact is well appreciated when openings near the inferolateral corners of the sellar dura result in vigorous venous bleeding from projections of the cavernous sinus in between the two layers of dura. Consequently, the lateral aspect of the IIS has to be clipped occasionally.
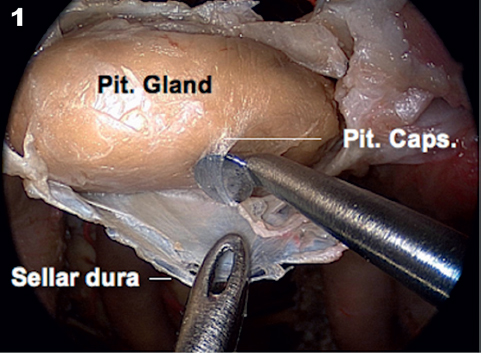
Fig. 28.1 The key for a successful pituitary transposition is preservation of the pituitary capsule, a distinct layer that must be preserved when opening sellar dura. Caps.: capsule; Pit.: pituitary.




