Chapter 47 Transtemporal Approaches to Posterior Cranial Fossa
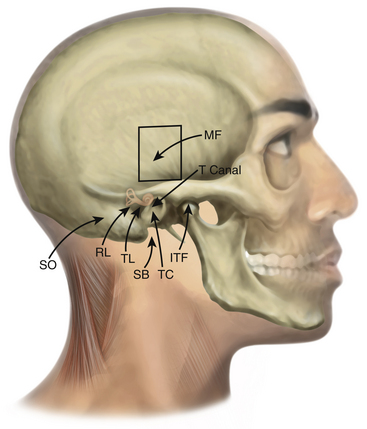
Traditional approaches to the posterior cranial fossa do not permit direct access to complex lesions of the lateral skull base, cerebellopontine angle (CPA), or clivus. To circumvent brain retraction and allow for complete resection, approaches have been developed that position the dissection both lateral and anterior to the brain stem and cerebellum. All of these skull base approaches are combinations and variations of transtemporal bone routes (Table 47-1 and Fig. 47-1). Unlike craniotomies performed elsewhere, entry to the posterior fossa through the temporal bone poses special problems for the surgeon if the internal carotid artery (ICA), sigmoid sinus (SS), cranial nerves VII and VIII, and specialized structures for hearing and balance are to be preserved. Despite the widely varied nomenclature, often only subtle differences exist among these approaches. It is imperative that the location, type, and extent of the lesion dictate the type of the approach. Tailored approaches to the lesion instead of standard ones are recommended for minimal disruption of normal structures. In this respect, transtemporal approaches represent an anatomic continuum of temporal bone dissection, with frequent overlaps and minor discrepancies or differences among the various approaches. The complicated nomenclature has arisen because skull base tumors tend to extend into different anatomic compartments, often necessitating combined approaches. Because of the overlap of neurosurgery and otology in this area, collaboration of neurosurgeons and otologists is mandatory.
TABLE 47-1 Temporal Bone Approaches
| Anterior Approaches |
| Middle cranial fossa |
| Extended middle cranial fossa |
| Middle cranial fossa transtentorial |
| Posterior Approaches |
| Retrolabyrinthine—presigmoid |
| Retrolabyrinthine—trans-sigmoid |
| Retrolabyrinthine—retrosigmoid |
| Translabyrinthine |
| Transotic |
| Transcochlear |
| Infralabyrinthine |
| Transcanal–infracochlear |
| Combined Approaches |
| Petrosal |
| Infratemporal fossa |
| Endoscopic Approaches |
| Endonasal endoscopic approach |
Anterior Transpetrosal Approaches
Middle Fossa Approach
House developed the middle fossa access to the IAC and adjacent structures in 1961 in an effort to remove foci of labyrinthine otosclerosis.1–3 Although he used this approach briefly for the removal of acoustic tumors, he soon directed his efforts to a translabyrinthine approach. Fisch and Mattox further refined the middle fossa approach.4,5
Several techniques for localization of the IAC have been described. House’s technique identifies the greater superficial petrosal nerve (GSPN), follows it to the geniculate ganglion (GG), and then proceeds along the labyrinthine segment of the facial nerve to the IAC.2 Another popular method described by Fisch and Mattox uses the superior semicircular canal (SSC) as the primary landmark.5 Using this method, once the SSC is identified, the meatal plane overlying the IAC is located in a 60-degree plane centered over the SSC ampulla. Garcia-Ibanez and Garcia-Ibanez6 advocate a technique beginning at the bisection of the angle between the GSPN and the arcuate eminence. Lan and Shiao, in a cadaveric study, described the technique of finding the IAC by drilling a point that is 9.9 mm medial from the GG on a line angled with the GSPN by 96 degrees.7 Because the medially IAC dura enlarges threefold, and there are no neural structures anterior to it, the medial or proximal “safe” part of the IAC is first identified and is followed laterally: once the IAC dura is exposed, it can be distinguished from the posterior fossa dura by its “pinkish” color in contrast to the “white” posterior fossa dura.8 Other techniques involve drilling to expose the semicircular canals and exposure of the ossicles in the middle ear as a reference point.9 Because of the wide variations in anatomy4,6 and small working space, no single technique can ensure avoidance of injury to important structures. Careful dissection and a detailed understanding of the regional anatomy are important for success. Image-guided navigation through the temporal bone has been introduced as an accurate alternative method to localize the IAC without the need to expose the GG or the SSC.10,11
Indications
The middle fossa approach is best suited for lesions situated lateral within the IAC that have limited extension into the CPA (less than 1 cm) and where hearing preservation is the goal.2,12 It is especially useful when preoperative computed tomography (CT) of the temporal bone demonstrates the proximity of the posterior semicircular canal (PSC), common crus, or vestibule to the posterior lip of the IAC. In those circumstances, retrosigmoid approaches are less preferable and the middle fossa approach becomes the hearing-preservation approach of choice. Tumors that are medial in position and do not extend to the fundus of the IAC are best approached by posterior approaches (e.g., retrosigmoid approach).
The middle fossa approach provides access to the labyrinthine segment of the facial nerve without sacrificing hearing. Thus, decompression of the facial nerve in trauma or Bell’s palsy, or resection of facial nerve tumors can be accomplished. During vestibular schwannoma removal, early identification of the facial nerve allows better functional preservation. In a recent retrospective literature review that included 296 studies and more than 25,000 patients, facial nerve preservation was highest in patients treated with middle fossa (85%) approach compared to translabyrinthine (81%) and retrosigmoid (78%) approaches.13 However, the main factor contributing to the facial nerve preservation was found to be tumor size, which is consistent with other studies.14 Therefore, bias can be a contributing factor, because most schwannomas treated with the middle fossa approach are small or medium sized. This approach also permits selective sectioning of the vestibular nerve fibers for Ménière’s disease. In theory, it could also be used to expose the horizontal portion of the ICA, eustachian tube, and temporomandibular joint (TMJ). Other indications include advanced otosclerosis, nerve section for tinnitus, facial nerve repair and facial nerve neuroma, repair of middle fossa encephaloceles, and cerebrospinal fluid (CSF) leakage through the tegmen.2
Surgical Approach
The patient is positioned supine on the operating table with the head turned opposite the side of the tumor.2,4,6,12,15 Facial and auditory nerve monitoring is used. An incision is planned that begins at the level of the zygoma just anterior to the tragus and extends superiorly to approximately the superior temporal line. We prefer an S-shaped incision curving first anteriorly and then posteriorly to allow for greater spreading of the soft tissues.
The temporalis muscle is divided and reflected anteriorly. A 4- by 5-cm bone flap is planned approximately two thirds anterior and one third posterior to the EAC. The inferior margin should be placed as close to the middle fossa floor as possible. A subtemporal craniectomy is performed. The dura is then elevated from the middle fossa floor in a posterior to anterior direction. This direction of dissection helps avoid inadvertent elevation of the GSPN and subsequent traction injury to the GG and facial nerve. Injury to the GSPN can produce a dry eye secondary to loss of lacrimal gland innervation. In approximately 16% of cases, the GG is not covered by bone and inadvertent injury can occur.4 To maintain a visible plane of dissection, a self-retaining brain retractor is used. Some retractors are limited to only 4 to 5 cm of spread; thus, too wide a craniotomy can impair the capability of the retractor to elevate the dura adequately.
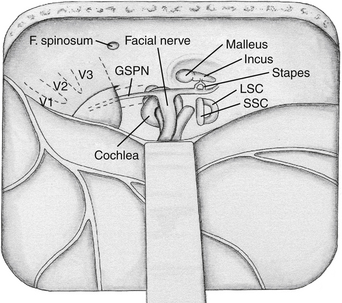
Several landmarks must be identified before bone removal can begin over the IAC: (1) the middle meningeal artery, (2) the arcuate eminence, (3) the GSPN, and (4) the facial hiatus (Fig. 47-2). The first landmark is typically the middle meningeal artery at the foramen spinosum. This can be obliterated and divided if necessary. The foramen may be, albeit rarely, duplicated or absent. It marks the anterior limit of the dural elevation. As dural elevation continues, the arcuate eminence, a rounded elevation of the petrous bone, can be identified. It is usually produced by the underlying SSC. Lateral to the arcuate eminence is the tegmen tympani, a thin lamina of bone that forms the roof of the tympanic cavity. The GSPN originates from the GG, exits through the petrous bone at the facial hiatus, and runs extradurally in an anteromedial direction toward the trigeminal ganglion. The GSPN serves as a landmark for the lateral margin of the horizontal segment of the petrous carotid artery. Care should be taken at this stage not to apply force to the floor of the middle fossa, because the bone over the carotid artery and the area of the tegmen can be quite thin and even dehiscent in up to 20% of cases.4 The arcuate eminence is drilled until the dense bone of the SSC is encountered. The SSC is visualized with a bluish hue through the bone, the so-called blue line. In approximately 15% of cases, however, the arcuate eminence is absent; in 50% of cases where it is present, it is rotated in relationship to the SSC.16
Once the key landmarks have been identified, the IAC can be localized using two key angles. Traditionally, the GSPN-SSC angle (120 degrees)6 and the SSC-IAC angle (60 degrees)17 have been used. Unfortunately, these angles have been shown to be quite variable,15 and in one study the GSPN-SSC angle ranged from 90 to 135 degrees and the SSC-IAC angle from 34 to 75 degrees.4 Thus, simply relying on angles can lead to inadvertent injury to the SSC and hence loss of hearing. House’s technique places the facial nerve at risk, because this structure is first identified and then followed to the IAC.2 Fisch’s technique places the SSC at risk. Orientation can be aided by removal of the tegmen and identification of the head of the malleus.9 This can help predict the location of the GG and IAC because these structures are usually collinear, at the expense of risking a CSF leak through the middle ear.2 None of these techniques is failsafe, and the best method of localizing the IAC is what the surgeon finds most comfortable in his or her own experience.
Once the IAC has been identified, exposure proceeds from lateral to medial until the entire IAC has been exposed along its superior surface. A safer technique is to begin medially, expose the porus acousticus first, and then work laterally, taking advantage of the larger margin for error in the region of the porus.8,12,15 At the fundus of the IAC, the vertical crest (Bill’s bar), a bone spicule that separates the superior vestibular nerve from the facial nerve, is identified. Finally, the dura over the IAC is opened, first posteriorly over the superior vestibular nerve to avoid facial nerve injury.
In the case of vestibular schwannomas, the tumor can be removed by separating the superior vestibular nerve and tumor from the facial nerve. The tumor is usually delivered posteriorly away from the facial nerve. Small hooks are necessary to palpate the limits of the IAC and gently free the tumor, particularly from its inferolateral portion, where the view is especially obscured. The approach carries a higher risk to the facial and cochlear nerves when the tumor less commonly arises from the inferior vestibular nerve. A rigid 0- or 30-degree endoscope can be used at the end of the procedure to inspect for residual tumor, facial and cochlear nerve integrity, and opened air cells.18 Closure of the IAC defect is accomplished with a small free graft or temporalis muscle.
Complications and Disadvantages
The middle fossa approach requires retraction of the temporal lobe;19 therefore, injury can potentially occur (e.g., aphasia, hemiparesis, or seizure). There is potential for CSF leakage through unwaxed air cells or through the middle ear, if the tegmen is opened. Careful hemostasis and tenting sutures can lessen the risk of postoperative hematoma (e.g., epidural hematoma).
Extended Middle Fossa Approach (Anterior Petrosectomy)
The traditional middle fossa approach works well for lesions in the IAC;2,3 however, the exposure is limited. For that reason, extensions of the middle fossa approach have been developed to permit wider access to the petrous apex, clivus, and posterior fossa. The extended middle fossa approach involves a petrous apex resection, in addition to the temporal craniotomy described for the middle fossa approach.20 The horizontal segment of the carotid artery and the cochlea limit the inferior exposure to the level of the inferior petrosal sinus. The TMJ, ossicles, and petrous carotid artery laterally; the trigeminal ganglion anteriorly; and the SSC and vestibule posteriorly represent the limits of the extended middle fossa approach.
Indications
The anterior petrosectomy provides access to the petrous apex and superior clival region. It provides access to the posterior fossa past the carotid artery and trigeminal and facial nerves. Although the extended middle fossa approach is considered a hearing-preservation approach, it can provide additional exposure in the posterior fossa by sacrificing the SSC and labyrinth—and thus hearing.20,21 Sacrifice of the cochlea improves visualization of the lateral extreme of the IAC, the medial wall of the tympanic cavity, and the jugular foramen if needed.
The extended middle fossa approach permits resection of vestibular schwannomas that extend more medially in the CPA. Meningiomas and chordomas of the anterior CPA and clivus can be resected through this approach, as well as lesions of the petrous apex (i.e., cholesteatomas and petrositis). The middle fossa approach is not recommended for cholesterol granulomas because of the absence of permanent aeration and the need for temporal lobe retraction.22 Large lesions may be difficult to resect by this approach, and the angled endoscope can be used to deal with blind spots.23 Lesions of the posterior cavernous sinus, basilar artery, and anterior brain stem up to the level of pontobulbar junction can also be approached.24 The petrous carotid artery can be also approached for bypass anastomosis.25
Surgical Approach
A temporal craniotomy is performed, similar to the middle fossa approach. Occasionally, a zygomatic osteotomy is added for exposure of the middle fossa floor. The middle meningeal artery, foramen ovale, GSPN, and arcuate eminence are identified. The dural sheath of the trigeminal ganglion and its continuation as V3 forms the superior limit of this approach.24 The petrous carotid artery can be exposed at this point by drilling bone along the course of the GSPN (see Fig. 47-2). This area is also known as the posterolateral or Glasscock’s triangle.26 The boundaries of Glasscock’s triangle are a line extending from the foramen spinosum to the arcuate eminence laterally, the GSPN medially, and the third division of the trigeminal nerve (V3) at the base. Medial to this triangle is Kawase’s, or the posteromedial, triangle, which consists of the bone in the area of the petrous apex. Drilling this bone provides access to the clivus and the infratentorial compartment.27 Kawase’s triangle is defined laterally by the GSPN, medially by the petrous ridge, and at the base by the arcuate eminence. Usually the GSPN is sacrificed to avoid traction to the GG and subsequent facial paralysis. Arcuate eminence is absent in significant number of the patients. Therefore, foramen ovale and spinosum can be used alternatively as landmarks to start drilling.24 The cochlea represents the posterolateral limit of exposure within Kawase’s triangle. Infracochlear lesions are hard to access with the conventional approach, and an endoscope can be helpful.23
The IAC is identified by one of the means described in the previous section. Once the IAC is identified, bone is removed, exposing the canal widely and the dura of the posterior fossa. The otic capsule bone is particularly dense and lighter in color than the remaining bone of the petrous apex. To identify the cochlea, Miller et al.28 advocate drilling bone along an imaginary line extending from the tip of the vertical crest to the junction of the petrous carotid artery and cranial nerve V3 until the cochlea is identified. With this exposure, the dura along the medial temporal lobe and infratentorially to the level of the inferior petrosal sinus can be exposed. The superior petrosal sinus (SPS) can be clipped and divided. A dural incision can be extended across the SPS and then inferiorly into the posterior fossa. Occasionally, the dura over Meckel’s cave is divided to mobilize the trigeminal nerve anteriorly and increase exposure of the petroclival region.
The approach can be extended into the infratemporal fossa by removing the bone from lateral to medial toward the foramen ovale. This maneuver eventually connects the temporal and infratemporal fossae, allowing tumor removal, especially in the case of trigeminal schwannomas, with extension along V3.19
Middle Fossa Transtentorial Approach
The middle fossa transtentorial approach was first reported by Kawase et al.27 in 1985 for approaching aneurysms of the midbasilar artery through the petrous pyramid. In 1991, Kawase et al.29 applied this approach for resection of petroclival meningiomas that extended into the parasellar region (sphenopetroclival meningiomas). This approach uses a combination of the extended middle fossa approach with the addition of intradural resection of the tentorium to allow wider posterior fossa exposure. It is in many ways similar to the subtemporal transtentorial approach, with the added advantage of drilling the anterior petrous ridge.
Indications
The middle fossa transtentorial exposure can be accomplished with an anterior or posterior petrosectomy or a combined petrosal approach.20,29–31 It is suitable for meningiomas extending along the superior and middle clivus or along the posterior wall of the petrous ridge, which can have long dural attachments. Hearing is preserved with this approach, as with all middle fossa approaches. It also permits resection of tumors that extend to the parasellar region and posterior cavernous sinus. It is particularly attractive for small tumors in the petroclival region, laterally located pontine lesions (cavernous malformations and gliomas), or basilar trunk aneurysms. Compared with the extended middle fossa approach, it provides wider posterior fossa exposure because of sectioning of the tentorium.
Surgical Approach
The extent of petrous pyramid resection is similar to that obtained by the extended middle fossa approach. The dura is opened above and below the SPS. Cranial nerves IV and V are identified. The SPS is clipped between cranial nerves V and VII, with care taken to avoid sacrificing the petrosal vein. Alternatively, the SPS can be embolized preoperatively.24 The tentorium is cut until the tentorial notch is seen. The tentorium can then be tented open with retention sutures, exposing the petroclival region from cranial nerves III through VII.30 The inferomedial triangle of the cavernous sinus can be visualized, mobilization of the trigeminal nerve can be accomplished by opening Meckel’s cave, and Dorello’s canal can be seen through this exposure.
Posterior Transpetrosal Approaches
Retrolabyrinthine Approaches
Presigmoid Approach
The retrolabyrinthine presigmoid approach was first described by Hitselberger and Pulec32 in 1972, and was popularized by Norrell and Silverstein33 in 1977 and by House et al.34 in 1984. It is performed through the mastoid air cells, with elevation of a dural flap between the labyrinth and the SS. The concept of this procedure is based on its allowing entry into the CPA anterior to the SS, thus lessening the need for cerebellar retraction. It was originally described as being useful for partial sectioning of the fibers of the sensory roots of cranial nerve V for trigeminal neuralgia. It has been used for selective sectioning of the vestibular division of cranial nerve VIII for treatment of vertigo and for endolymphatic duct surgery. It can occasionally be used to remove small acoustic tumors when preservation of hearing is desirable. The major advantage of this approach is that it provides direct access to the CPA without sacrificing hearing and without extensive cerebellar retraction. Its major disadvantage is the limited exposure, which can be compromised even further by a large dominant SS or when the mastoid air space is contracted (“crowded mastoid”).
Trans-sigmoid Approach
The trans-sigmoid approach can be used as part of any posterior transpetrosal approach. Exposure is increased by ligating the SS, usually between the superior and the inferior petrosal sinuses or between the inferior anastomotic vein (vein of Labbé) and the SPS. Thus, the inferior anastomotic vein drains into the transverse sinus and retrogradely into the opposite jugular system. A preoperative angiogram or magnetic resonance venogram is essential to ensure patency of the torcular. A nondominant sinus in the presence of a patent torcular can be sacrificed in selected cases. Temporary clipping across the SS is recommended to assess for the presence of temporal lobe or cerebellar swelling. The SS can be opened and packed with Surgicel and its lumen sutured, or it can be ligated and clipped. Uyar et al.35 described an original technique for sinus closure without opening the dura or the sinus itself. Posterior fossa and presigmoid dura are exposed first, and parallel suture is passed in front and back of the sinus. The muscle graft is placed between and sutures are tied, resulting in bending and obliteration or the lumen. Cadaver and angiographic studies show that the incidence of unilateral transverse sinus is rather infrequent (2.5%) and absence of any communication at the torcular is even rarer.36,37 Despite this, given the catastrophic results of ligating a unilateral SS, a preoperative arteriogram or magnetic resonance venogram is recommended. This approach is advantageous in cases of tumor growth into the SS with spontaneous obstruction. Jugular foramen tumors spreading into the jugular bulb and SS can be managed by ligation of the internal jugular vein in the neck followed by opening the SS, packing, and tumor removal.38
Retrosigmoid (Suboccipital) Approach
The retrosigmoid approach, also known as the lateral suboccipital approach, is not a true transtemporal approach. This approach is most familiar to neurosurgeons and has been the traditional exposure used for resection of tumors of the CPA.39,40 This approach provides wide entry into the posterior fossa, with maximal exposure for tumors such as vestibular schwannomas. Using this approach, the neurovascular structures of the temporal bone are avoided at the expense of cerebellar retraction. The development of monitoring techniques using evoked response methods has greatly increased the practicality of this approach.
Surgical Approach
The retrosigmoid approach can be done with the patient sitting, lateral, or three fourths prone. The head position is carefully adapted to the procedure type that is performed. With upper complex exposure (cranial nerve V and SCA) the vertex should be tilted downward. If the procedure involves the middle complex (cranial nerves VII and VIII, anteroinferior cerebellar artery) or the lower complex (cranial nerves IX-XI, posteroinferior cerebellar artery), the degree of tilt decreases or is reversed. An incision is made approximately 2 cm posterior to the mastoid tip, extending cephalad to slightly above the transverse sinus and caudally into the suboccipital musculature. The asterion has been used as a useful landmark for the junction of the transverse sinus and SS. However, a study showed that it is a quite unreliable landmark and that placing a bur hole over it can potentially lead to sinus damage.41 Neuronavigation alternatively has been shown to locate the position of the transverse sinus–SS junction more accurately.42 Craniectomy or “silver dollar” craniotomy can be performed such that the edges of the transverse sinus and SS and their junction are clearly identified. In difficult reoperative cases, a line drawn from the root of the zygoma to the inion can reliably locate the course of the transverse sinus.43 Bone removal can include the posterior lip of the foramen magnum, as well as the upper cervical lamina. The arachnoid at the foramen magnum should be opened first to permit CSF egress and facilitate cerebellar retraction.
The “extended retrosigmoid approach” involves removing of the bone over the SS to expose its entire length from the transverse sinus to the jugular bulb. This allows some degree of sinus retraction when the dura is reflected anteriorly, lessening the degree of cerebellar retraction.44,45 However, venous flow can be impaired intra- or postoperatively. so frequent reassessment should be performed.44
In the case of vestibular schwannoma resection, the tumor is immediately visualized. It can be explored initially with a rigid endoscope to verify the position of neurovascular structures to the tumor and extent of the tumor to the IAC.18 The facial nerve usually lies anterior to the tumor. For tumors that extend into the IAC, the porus is drilled until the dura over the IAC is seen. In a cadaver study, the amount of posterior IAC that can be safely unroofed averaged 5.9 mm (range 4-8 mm). The best available way to avoid critical labyrinthine structures during the suboccipital approach is to use preoperative high-resolution CT. A line is drawn on axial CT images from the medial aspect of the SS to the fundus of the IAC. If this line crosses any labyrinthine structures, the risk of injury and hearing loss during drilling of the IAC significantly increases.46 In addition, air cells can be encountered during drilling with possibility of postoperative CSF leakage. Alternatively to drilling of the IAC a 70-degree rigid endoscope can be used to visualize the canal and remove tumor remnants.47
Complications and Disadvantages
This exposure requires a certain amount of cerebellar retraction; thus, cerebellar edema or hematoma can occur. This is especially true for large tumors requiring lengthy surgery. If the surgeon maintains gentle retraction (1-2 cm), these types of complications can usually be avoided. In cases of small or medium-sized tumors, an endoscope alone can be used for tumor removal to reduce the amount of cerebellar retraction.48 The extended retrosigmoid approach also reduces the degree of cerebellar retraction. However, there is risk of postoperative sinus thrombosis.44 The facial nerve lies on the anterior surface of the tumor somewhere between the superior and the inferior poles. Therefore, some amount of tumor removal is required to visualize the nerve. This is one of the disadvantages, because manipulation alone can cause nerve traction injury. A possible way to avoid injury to the facial nerve is to start medial to the tumor close to the brain stem or lateral in the region of IAC, where the nerve relation to tumor is relatively constant. After identification of the nerve, tumor removal can be performed safely. Other complications include CSF leakage and postoperative incisional pain attributed to adherence of the suboccipital muscles to the dura. The incisional pain can be lessened by either replacing the bone flap, in the case of a craniotomy, or performing a cranioplasty to fill the bone defect. The incidence of CSF leakage may be lessened by identifying and waxing small air cells in the IAC with the use of an endoscope. In 9% of cases, a high jugular bulb may make drilling of the meatus through the retrosigmoid approach impossible and is associated with increased risk of bleeding and air embolism.49 As previously mentioned, loss of hearing can occur during drilling of the posterior aspect of the IAC.
Translabyrinthine Approach
The first report of a translabyrinthine approach was in 1904 by Panse,50 who advocated this approach for its shortest distance to the CPA. In 1961, House3 described the middle fossa approach for resection of vestibular schwannomas located laterally in the IAC with minimal CPA extension. Because of limited exposure, incidence of facial paresis, need for temporal lobe retraction, and limited control of vascular structures, House and Hitselberger51 introduced the translabyrinthine approach for resection of vestibular schwannomas. This was a more lateral approach and gave direct control of the facial nerve by drilling through the labyrinth. They emphasized the vertical crest at the lateral end of the IAC as a landmark. Differentiation between the superior and the inferior vestibular nerves was more readily apparent with this approach.
Variations of the translabyrinthine approach have been described for more extensive exposure of the SS, with mobilization of the jugular bulb, as well as drilling out of the infralabyrinthine air cells to increase access for large tumors.52 Furthermore, there is evidence that in rare cases hearing preservation may be possible with the translabyrinthine approach, such that in one case ablation of all three semicircular canals with preservation of the cochlea and saccule left the patient with useful, though decreased, hearing.53 Another variation of the translabyrinthine approach is the addition of a suboccipital approach with a partial labyrinthectomy, such that only those elements that are required for visualization of the vertical crest and the lateral IAC are removed.54
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree