Eye opening
Motor response
Verbal response
Response
Score
Response
Score
Response
Score
Spontaneous
4
Obeys
6
Oriented
5
To speech
3
Localizes
5
Confused
4
To pain
2
Withdraws
4
Inappropriate
3
None
1
Abnormal flexion (decorticate rigidity)
3
Incomprehensible
2
Extension response (decerebrate rigidity)
2
None
1
None
1
The mildest head trauma is a concussion leading to rapid but transient neurologic impairment. In very mild concussions, the patient may experience only a brief period of disorientation and amnesia for the event. Typically, patients will have a brief loss of consciousness after impact but a concussion can occur even without loss of consciousness. The loss of consciousness is associated with suppression of reflexes with a fall if they are standing, transient arrest of respiration, brief period of bradycardia, and a transient fall in blood pressure. Patients complain of headache, nausea and vomiting, confusion, disorientation, attention deficit, dizziness , and unsteadiness. Concussions are frequent, occurring in 15 % of sports-related injuries. Having one concussion predisposes to repeated concussions from new sports injuries. These patients have normal neuroimaging.
Moderate to severe head trauma produces loss of consciousness for a longer duration, usually more than 5 min. Awakening is slow, confused, and often with retrograde and anterograde amnesia .
Pathophysiology
Brain damage from TBI is divided into two mechanisms: primary and secondary brain injury. Primary injury describes the initial structural injury to the brain as a direct result of the impact on the brain. It occurs at the moment of head trauma with several factors contributing to the brain damage. An acceleration–deceleration force transmitted to the head causes distortion of the brain in various areas depending on the part of head impacted first and the severity of the blow.
Diffuse axonal injury occurs in the majority of moderate to severe TBI patients when the patient has a low Glasgow coma scale score for over an hour. Axonal injury occurs from stretching or tearing the axon at the moment of impact primarily, but additional axonal destruction develops later when excess calcium entry and swelling further damages axon segments (Fig. 18.1). Common sites of axonal injury include medial frontal gyrus, temporal lobes, cerebral white matter, corpus callosum, cingulate gyrus, thalamus, and upper brainstem. Initially, an axon bulb (retraction bulb) develops followed in a few weeks by accumulation of microglia at the injury site. Wallerian degeneration of the axon tract occurs months after the initial injury.
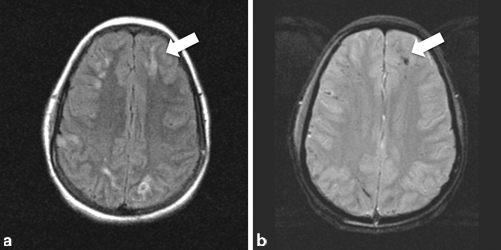
Fig. 18.1
a Axial MRI FLAIR sequence showing bright signal ( arrow) of diffuse axonal injury and b Axial MRI gradient sequence showing dark signal ( arrow) indicating hemorrhage in same area. (Courtesy of Dr. Blaine Hart)
Secondary brain injury begins at the time of brain trauma and progresses remote from the injury. It can develop from a compressive force like a depressed skull fracture or secondary intracranial mass from cerebral edema, parenchymal hemorrhage or extraparenchymal epidural or subdural hematoma . A mass lesion can lead to decreased consciousness from mass effect exerted directly by the lesion on the diencephalon, mesencephalon , or brainstem or indirectly by increased intracranial pressure—both mechanisms could lead to herniation. Secondary brain injury also develops from a cascade of metabolic events including abnormal cellular metabolism, loss of autoregulated cerebral blood flow, disruption of extracellular and intracellular ions, and abnormal release of neurotransmitters . Axonal stretching and shearing often leads to acute release of neurotransmitters such as glutamate and causes abnormal neuronal firing releasing a potassium efflux, accelerated glycolysis, lactate accumulation, alterations in cerebral blood vessel blood–brain barriers, and cerebral edema.
Skull fractures portend considerable brain injury and are found in 3 % of head trauma patients seen in emergency rooms, in over 50 % of patients who are hospitalized, and in 80 % of those who die. Over half the patients have a linear skull fracture , and 4 % of these fractures are depressed from their normal location. Less common skull fractures may involve the petrous bone resulting in a CSF leak or blood accumulating behind the tympanic membrane, blood leakage into the mastoid area, blood leakage into periorbital tissues around the eyes, or CSF leakage through the nose (otorrhea) from a fracture involving the cribriform plate.
The pia-arachnoid membrane remains intact over a contusion but in a brain laceration, it tears producing bleeding into the subarachnoid space. Contusions and lacerations characteristically occur on the inferior surfaces of the frontal and temporal lobe poles where the brain comes in contact with bony protuberances of the skull base such as the frontal and temporal lobes. The crests of the gyri suffer the greatest injury. Contusions usually develop at the site of injury (coup) or in the brain diametrically opposite the site of injury (countercoup).
Diffuse vascular injury is commonly seen in severe TBI. Petechial hemorrhages are seen throughout the hemispheres, basal ganglia, and brainstem from shearing damage to small blood vessels. Intracerebral hematomas develop in 10–15 % of patients, may be single or multiple, and often locate in the frontal and temporal lobes.
The effects of secondary injury may not present clinically until later. Brain swelling, an important cause of secondary injury, begins shortly after the trauma. Local edema develops at areas of brain necrosis from contusion, expanding intracerebral hematomas, or pockets of subarachnoid blood. As the intracranial pressure (ICP) elevates, diffuse brain ischemia may develop if the cerebral blood flow falls to critical levels and no longer perfuses brain tissue. Subdural or epidural hematomas may also contribute to increasing ICP. Once ICP reaches a critical level (above 20–25 mmHg), ischemic brain damage develops. One study found ischemic brain damage present in 90 % of TBI patients (severe in 27 %, moderate in 43 %, and mild in 30 %). The most common locations of ischemic damage were the hippocampus, basal ganglia, and cerebral hemispheres in the watershed territories (boundary zones between the anterior and middle cerebral arteries and middle and posterior cerebral arteries).
Clinical Features and Immediate Evaluation
Mild TBI (GCS 13–15) is the most common. These patients experience a simple concussion (brief loss consciousness without permanent brain damage) or may not lose consciousness but are stunned (see “stars”). They may not recall the event. Such patients may experience short-term memory and concentration difficulties that persist for days to months. In the emergency department, they have a normal neurologic examination and no signs of body injury. Some complain of immediate posttraumatic symptoms such as headaches, fatigability, insomnia , and nervousness, but these symptoms may also arise within a few days of the head trauma. These patients have a good prognosis and usually can be released from the emergency department after several hours of observation to a competent caregiver who will bring the patient back should he deteriorate.
For moderate to severe TBI, immediate attention to the patient at the scene of the trauma or in the emergency department is important. A quick but thorough systemic trauma evaluation should be done according to advanced trauma life support guidelines. Care should be taken to evaluate the potential of spine or neck injury as 10 % of patients with moderate to severe head trauma also have spine injuries. A Glasgow coma scale (GCS) should be done. Monitoring of blood pressure, heart rate, respiration rate, and oxygen saturation is important.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








