Chapter 38 Tumors Involving the Cavernous Sinus
Until 1965, when Parkinson’s landmark article describing the direct surgical approach to carotid-cavernous fistulas was published, little reference was made in the neurosurgical literature to direct operative attack on lesions of the cavernous sinus.1 This lack of information was largely a result of the inability in the premicrosurgical era to address effectively the extreme risks of significant hemorrhage and damage to the cranial nerves in the region. This anatomic locale has long been considered a true “no man’s land” for direct surgical approaches. The modern era of microneurosurgery has realized expanded capabilities in microsurgical technique and has fostered the work of several neurosurgeons who have made great strides in effectively approaching this region with reduced morbidity.2–20 In particular, the work of Dolenc should be recognized for the development of his combined epidural and subdural approach, which has become the standard method used to directly access lesions in this region.6
More recently, within the last decade, endonasal endoscopic approaches to the cavernous sinus region have been developed as an alternative to an open craniotomy.21–24 These approaches are not commonly utilized, but the current trend in anterior and middle cranial base surgery is to incorporate these strategies as a minimally invasive alternative. These techniques are mentioned as they are becoming an important element of the armamentarium in dealing with these lesions. However, they are complex enough to warrant a separate and entire chapter themselves. Here we will focus on the transcranial techniques in detail.
Indications
The indications for direct operative attack on neoplastic lesions arising in or involving the cavernous sinus have been a matter of debate. New forms of therapy, such as stereotactic radiosurgery, are providing alternatives in our armamentarium for treating these difficult tumors.25–27 A more restrictive set of indications for operative intervention has evolved within the past decade. We briefly consider the presently acceptable indications for a direct operation on these lesions.
The presence of a mass in the cavernous sinus, of course, does not itself constitute an indication for a direct operation. Many variables must be taken into account, including the age and medical condition of the patient, imaging characteristics, adjacent structures involved, time course of the process, and functional severity of symptoms. Many patients, because of poor medical condition or refusal to undergo surgery, may not be candidates for intracavernous microsurgery under any circumstances. The primary indications for surgery in most cases at present depend upon whether radiousurgery can be done safely as the primary treatment or not. Patients that have direct involvement, for example, of the optic apparatus by extension of tumor, cannot have radiosurgical treatment without significant risk of radiation delivery over acceptable minimums to these structures. In such case, an expert debulking of the lesion with creation of sufficient space between residual tumor and the optic apparatus is indicated. Patients with symptoms such as severe retro-orbital pain are also considered candidates for a debulking procedure, in order to relieve them of symptoms. Reports have demonstrated that stereotactic radiosurgery presents a viable alternative in patients with most intracavernous meningiomas.27 At present, most patients who harbor lesions of the cavernous sinus are considered for radiosurgical treatment as primary treatment, with the possibility of surgery as an adjunct to their overall treatment. In some cases, patients with benign, well-circumscribed tumors in the cavernous sinus are candidates for a primary surgical approach for resection of the lesion. Most of these patients have lesions that are consistent with benign tumors of the region (e.g., neurinomas, cavernous hemangiomas, pituitary adenomas, dermoids, chordomas, and chondrosarcomas). These tumors tend to be well-encapsulated masses that are dissectible from the surrounding structures.
Patients with apparent meningiomas of the cavernous sinus, although their tumors are benign, are considered for surgery only in select circumstances. Patients who are able to undergo surgery who have debilitating symptoms, such as rapid visual loss or painful ophthalmoplegia, are offered an operation with the goal of decreasing the mass of the tumor and providing space for the tumor to expand via decompression at the skull base. The goal of such an operation is decompression of the involved structures, with a total resection attempted only when circumstances are very favorable. Patients with asymptomatic, small meningiomas are followed up with serial scans until they show enlargement of the mass or neurologic symptoms. A select few patients with tumors that are located at the lateral wall of the cavernous sinus and involve the temporal dura propria without cavernous invasion may be offered surgery. This is reasonable in such situations as the tumor can be completely removed with a minimum of risk of permanent neurologic deficits. These decisions rely on the judgment of the surgeon experienced with tumors in this area.
Difficult decisions are made in cases in which cavernous sinus involvement occurs by extensions of malignant processes from the paranasal sinuses and pharynx. Procedures treating such disorders are palliative because of the characteristically aggressive nature of these tumors, such as squamous cell carcinoma. En bloc resection of the cavernous sinus and adjacent areas may represent merely a heroic effort on the patient’s behalf, with little realistic chance of long-term survival. Localized malignancies are an entirely different prospect in most cases. Local invasion by chordomas or chondrosarcomas can be effectively resected almost totally in many cases, with long-term recurrence-free survival, even though these tumors are incurable.13
Surgical Anatomy
Work focusing on the microsurgical anatomy of the cavernous sinus and its adjacent structures has made a critical contribution to our understanding and capabilities in dealing with neoplasms involving the cavernous sinus.7,28–32 The individual surgeon’s facility with the anatomic details of this complex region cannot be overemphasized as a basis for successful surgical therapy. The anatomy as presented in conventional texts, although an important initial basis, provides insufficient knowledge for the neurosurgeon operating in this region. An intimate comprehension of the multiple entry corridors and their specific anatomic substrates and boundaries is critical to the safe implementation of these procedures. Adequate preparation, including judicious use of the cadaver dissection laboratory, enhances the chances for a successful approach to these lesions. This has become especially important with the introduction of advanced endonasal endoscopic techniques. These techniques introduce an entirely separate skill set that requires development in the laboratory to gain comfort and facility with the endoscope and the special instruments.
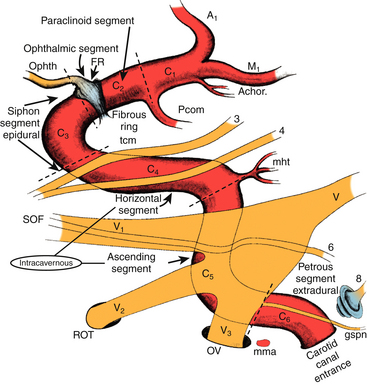
The anatomy of the intracavernous carotid artery deserves special attention. The artery enters the cavernous sinus, piercing the true cavernous membrane, at the foramen lacerum. It is surrounded here by a thickening of this connective tissue, which forms a fibrous ring around the artery. The artery then bends anterosuperiorly toward the superior orbital fissure. Just distal to this bend, the meningohypophyseal trunk typically arises on the superomedial side. This trunk has three branches: (1) the tentorial (Bernasconi-Cassinari), (2) the dorsal meningeal, and (3) the inferior hypophyseal arteries, all of which display some variability. The carotid artery usually gives rise to the artery of the inferior cavernous sinus on its lateral side as it courses anteriorly. This vessel traverses the sinus, usually crossing over cranial nerve VI, and anastomoses with several branches of the internal maxillary artery. These anastomoses include: (1) the recurrent meningeal artery at the superior orbital fissure, (2) the artery of the foramen rotundum, (3) the accessory meningeal artery at the foramen ovale, and (4) the middle meningeal artery at the foramen spinosum. The tentorial artery is absent from the meningohypophyseal trunk in some cases, and in these situations, a marginal tentorial artery is typically found arising from the artery of the inferior cavernous sinus.29 In a few patients (~10%), branches off the medial side of this segment (known as McConnell’s capsular arteries) supply the capsule of the pituitary gland.29
The artery makes another bend in the anterior portion of the cavernous sinus superomedially. This segment of the artery exits the cavernous sinus and pierces the enveloping membrane. The membrane in this region is called the carotico-oculomotor membrane, because it spans the gap between the oculomotor nerve in the medial wall of the cavernous sinus and the carotid artery.29,33 This loop is then completed in the extracavernous, extradural space under the anterior clinoid process. This loop has been designated the siphon segment, or clinoidal segment, and continues posteriorly a short distance before piercing the dura. Here, it is surrounded by a fibrous ring of dura, and the ophthalmic artery typically originates just inside this fibrous dural ring.33–35
The ICA has been assigned nomenclature that divides it into several segments by different authors. We have been using the system described by Fischer in 1938, which numbers the segments beginning from the carotid bifurcation.36 We make a small modification to the original system with regard to numbering the petrous carotid segment (Fig. 38-1). The C1 segment begins at the carotid bifurcation and extends to the origin of the posterior communicating artery. C2 is the ophthalmic segment described by Day, stretching from the posterior communicating artery to the fibrous dural ring.33 The extradural, extracavernous clinoid segment is given the designation of C3. C4 is the true intracavernous segment of the artery and is delimited by the carotico-oculomotor membrane anteriorly and the origin of the meningohypophyseal trunk posteriorly. From the meningohypophyseal trunk, the artery is designated as C5 until it has passed under the trigeminal nerve. The intrapetrous portion begins at the point at which V3 crosses over the artery and extends to its entrance into the carotid canal in the infratemporal fossa. This segment is designated as C6.
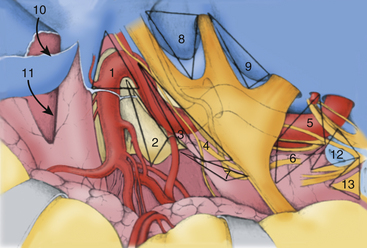
Crucial to the surgeon’s understanding of the relevant surgical anatomy of the cavernous sinus is a thorough working knowledge of the multiple triangular entry corridors into the region. The various entry points have been described by various authors and were brought together into a unified geometric construct of the region in 1986 by Fukushima.7 This scheme is illustrated in Fig. 38-2. Surgical facility with cavernous sinus lesions requires intimate knowledge of the entry spaces into the cavernous sinus in order to minimize morbidity. The anatomy as encountered from the endonasal endoscopic approaches is an important additional consideration. Understanding of the cavernous sinus from this additional perspective is an absolute prerequisite to such procedures.
Anterior Triangle
The anterior triangle describes an epidural space that contains the C3 portion of the ICA. It is exposed by removal of the anterior clinoid process, either intradurally or extradurally. The boundaries of the triangle are the extradural optic nerve, the fibrous dural ring, and the medial wall of the superior orbital fissure.4–637 The C3 carotid segment enters this space by piercing the carotico-oculomotor membrane. It is important to bear in mind the proximity of the oculomotor nerve, which runs in the medial wall of the superior orbital fissure, thus in apposition to the lateral boundary of this space.
Medial Triangle
The medial triangle is delimited by the intradural carotid artery, the posterior clinoid process, the porus oculomotorius, and the siphon angle of the carotid artery.9 This space is the primary corridor of access to the C4 portion of the carotid and thus is used for the direct approach to most intracavernous aneurysms. This space is also critical in terms of exposure for most intracavernous tumors.
Superior Triangle
The medial and lateral boundaries of the superior triangle are cranial nerves III and IV, respectively.7 The posterior margin is the edge of the dura along the petrous ridge. This triangle is the entry corridor used to locate the meningohypophyseal trunk.
Lateral Triangle
Described by Parkinson in 1965, the lateral triangle is a very narrow space that is delimited by the trochlear nerve medially and by the ophthalmic division of the trigeminal nerve laterally.1 Again, the dura of the petrous ridge forms the posterior margin. This triangle can be opened to expose cranial nerve VI as it crosses the C5 segment of the carotid artery.
Posterolateral Triangle
The posterolateral triangle, first described by Glasscock in 1968, describes the location of the horizontal intrapetrous carotid artery.38 Exposure of the artery in this space is a critical maneuver in gaining proximal control of the carotid artery. The foramen ovale, foramen spinosum, posterior border of the mandibular division of the trigeminal nerve, and cochlear apex define this space. Removal of the bone of this triangle exposes approximately 10 mm of the C6 segment of the carotid artery.39,40
Posteromedial Triangle
The posteromedial triangle describes the anterior petrous projection of a volume of bone that can be removed to make a window in the petrous apex to the posterior fossa. First described by Kawase and colleagues, this space is delimited by the cochlea, the porus trigeminus, and the posterior border of V3 at the posterior apex of the posterolateral triangle.41,42 If this triangle is used to make a window in the petrous bone, the anterior brain stem and root of the trigeminal nerve can be reached without encountering neural or vascular structures in the bone.
Anterolateral Triangle
The anterolateral triangle is defined by the area between the first and second divisions of the trigeminal nerve as they exit the middle cranial fossa. The anterior border of the triangle is an imaginary line drawn from the lateral edge of the superior orbital fissure to the medial lip of the foramen rotundum. This space is the entry point for exposure of the superior orbital vein and cranial nerve VI and is used to gain access to carotid-cavernous fistulas.43
Lateralmost Triangle (Lateral Loop)
Analogous to the anterolateral triangle, this space is bounded by V2, V3, and an imaginary line from the foramen rotundum to the foramen ovale. Lateral extensions of cavernous sinus tumors are also reached through this route. In some patients, the sphenoidal emissary foramen and vein are found here, communicating the cavernous sinus with the pterygoid venous plexus.29
Premeatal Triangle
The premeatal triangle is used to help define the location of the cochlea from the middle fossa angle of view. The boundaries are the medial lip of the internal acoustic meatus, the intrapetrous carotid genu, and the geniculate ganglion. The cochlea is located in the basal portion of this triangle. This triangle is important in cases in which the petrous apex is removed through the extradural middle fossa approach.39,40
Postmeatal Triangle
The postmeatal triangle delimits the volume of bone located between the internal auditory canal (IAC) and the superior semicircular canal and is used to maximize bone removal of the petrous apex through an extradural middle fossa approach.39 The boundaries are the geniculate ganglion, the lateral lip of the internal acoustic meatus, and the posterior end of the arcuate eminence.
Anesthetic and Monitoring Techniques
The ability of modern neuroanesthesia to facilitate operative procedures by providing increased relaxation of neural tissue and pharmacologic protection against ischemia has realized great improvements over the past forty years. Several maneuvers are used in transcranial cases to help maximize exposure while minimizing retraction of the brain. Administration of osmotic diuretic agents is routine at the beginning of each surgery. We infuse 20% mannitol solution (0.5 mg/kg) along with furosemide (20–40 mg) at the time of skin incision. Further relaxation is attained by maintenance of end-tidal carbon dioxide in the range of 25 to 30 mm Hg. In some cases, these maneuvers alone may not be adequate to provide adequate relaxation, necessitating the use of cerebrospinal fluid (CSF) drainage. This procedure is performed either through a ventricular catheter or a lumbar drain. We rarely use lumbar drainage of CSF in our transcranial cases, mainly because of personal preference. Patients with significant elevation of intracranial pressure are not well served by insertion of a lumbar drain at the beginning of the operation. If necessary, the safest and least complicated method is insertion of a catheter into the frontal horn of the lateral ventricle; this provides ample and accurate drainage of CSF throughout the operation. Administration of osmotic diuretic agents is not on the whole necessary in endonasal endoscopic trans-sphenoidal approaches to the cavernous sinus. In some cases, the pressure gradient between the intracranial compartment and the sphenoid sinus works to the advantage of the surgeon in terms of delivery of tumor into the field for removal. In general, lumbar drains are inserted in these cases when diversion of cerebrospinal fluid is necessary for help in closure of dural defects.
Neurophysiologic monitoring is routinely used in all cases. The specific configuration is tailored to each case, taking into consideration the operative approach and the neural and vascular structures likely to be compromised. Somatosensory-evoked potentials and electroencephalographic data are always recorded when there is a potential for temporary occlusion of the carotid artery. When the operative approach involves exposure of any part of the facial nerve, facial nerve monitoring is employed.44 Visual and brain-stem auditory-evoked potentials have not found much application in our cases of tumors involving primarily the cavernous sinus. But certainly in cases of posterior fossa skull base tumors with cavernous sinus extension, facial nerve monitoring is mandatory.
Surgical Approaches
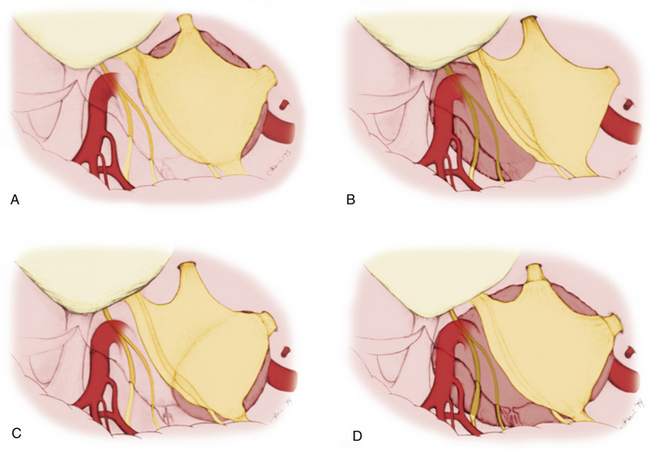
Mainly the specific entry corridors to the cavernous sinus expected to be used to resect the lesion dictate surgical strategy. The cavernous sinus can be divided into four separate quadrants. Lesions involving the anteromedial region are approached via the anteromedial and anterolateral triangles. Because these two triangles are exposed extradurally, in selected cases (e.g., neurinoma of V2), opening the dura might not be necessary in resecting such a lesion. This concept similarly applies to lesions located in the anterolateral quadrant, approached via the lateral loop and posterolateral triangles (Fig. 38-3A). This location of tumor also invites consideration of an endonasal endoscopic extended trans-sphenoidal approach. More posterior lesions, involving the posteromedial and posterolateral regions of the cavernous sinus, usually require exposure through the medial, superior, and lateral triangles (see Fig. 38-3B). These triangles, although possible to open through an extradural route, are typically entered intradurally. Posteromedial lesions without extension lateral to the cavernous carotid artery may also be considered for an endonasal endoscopic approach. Masses confined mainly to the posterolateral quadrant of the region are best approached in our opinion laterally through the middle fossa (see Fig. 38-3C). Lesions involving more than one of these four areas, for example, a mass with extensive posterior cavernous involvement with extension into the posterior fossa, may require a combined approach for adequate exposure (see Fig. 38-3D). This type of lesion requires a combined strategy via an anterolateral and middle fossa transpetrosal approach. Many lesions require more than one of the standard approaches for satisfactory exposure, and the experience and judgment of the surgeon are necessary to adequately plan the procedure. We outline the standard approaches to intracavernous neoplasms used in our practice and discuss the general indications for their use.
Frontotemporal Epidural and Subdural Approach to the Cavernous Sinus
Dolenc is credited with the initial development and use of the combined epidural and subdural frontotemporal approach (anteromedial transcavernous approach), originally used to directly approach intracavernous aneurysms.4,6 This technique has become the standard by which lesions within the cavernous sinus are approached. This strategy effectively exposes lesions confined to the cavernous sinus and those with extension to the supratentorial compartment. Lesions with extension into the petroclival area and the posterior fossa are not well exposed by this approach. The method is, however, easily combined with a more lateral approach (e.g., middle fossa transpetrosal) to gain access to such posterior extensions of tumor. Dolenc’s combined epidural and subdural strategy has been modified in several ways.37,47–49 These modifications largely center around the bone flap used and the extent of extradural bone removal at the skull base. The following discussion presents these modifications as alternatives to the basic approach; the modifications are selected on the basis of the exposure expected to be necessary.
Incision and Flap Elevation
We use three different methods of initial scalp incision and elevation, the choice of which depends mainly on the amount of inferior-to-superior exposure desired. Also, three different methods of craniotomy are used, again depending on the degree of inferior-to-superior exposure necessary.
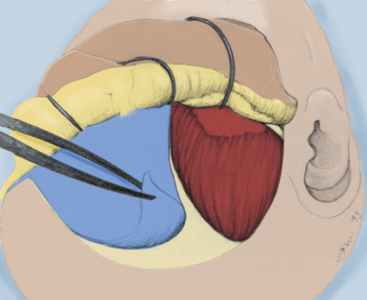
Two-Layer Technique
The two-layer technique is used when increased inferior-to-superior trajectory is necessary, because this technique results in reflection of the temporalis muscle inferiorly and laterally. This method rotates the muscle away from the orbital rim and frontozygomatic recess, thus preventing the muscle mass from creating an obstruction when the microscope is radically rotated to obtain a more rostral view. The skin incision is typically started slightly more inferiorly, exposing the entire zygomatic root. Beginning medially, the galeal layer is elevated from the pericranium, and the areolar bands, which span the two layers, are sharply divided. Again, the supraorbital and supratrochlear nerves must be preserved with the galeal layer. As the superior temporal line is reached, the areolar connective tissue that is continuous with the pericranial layer is elevated with the galea, which exposes bare temporalis fascia. The critical step in this maneuver is handling the temporal fat pad. This fat pad consists of superficial and deep components. The superficial fat pad is surrounded by the loose areolar connective tissue overlying the temporalis fascia and contains the frontalis branches of the facial nerve. The fat pad is elevated with the areolar tissue and the galeal layer. The galeal layer is elevated to expose the supraorbital rim, lateral orbital rim, and entire zygomatic process, which is covered by fascia. The deep fat pad is situated over the inferior portion of the temporalis muscle as it passes under the zygomatic arch and is covered by fascia. This pad of fat is left in place and retracted with the muscle (Fig. 38-4).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree